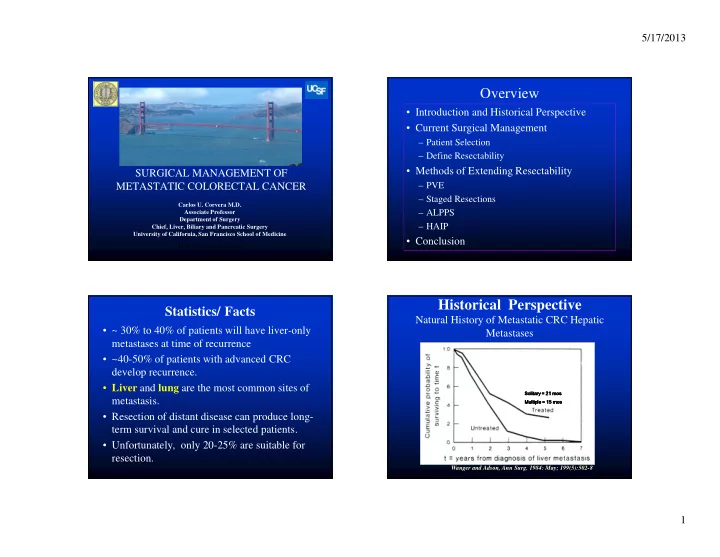
5/17/2013 Overview • Introduction and Historical Perspective • Current Surgical Management – Patient Selection – Define Resectability • Methods of Extending Resectability SURGICAL MANAGEMENT OF – PVE METASTATIC COLORECTAL CANCER – Staged Resections Carlos U. Corvera M.D. – ALPPS Associate Professor Department of Surgery – HAIP Chief, Liver, Biliary and Pancreatic Surgery University of California, San Francisco School of Medicine • Conclusion UCSF 2013 Postgraduate Course Historical Perspective Statistics/ Facts Natural History of Metastatic CRC Hepatic • ~ 30% to 40% of patients will have liver-only Metastases metastases at time of recurrence • ~40-50% of patients with advanced CRC develop recurrence. • Liver and lung are the most common sites of Solitary = 21 mos Solitary = 21 Solitary = 21 Solitary = 21 mos mos mos metastasis. Multiple = 15 mos Multiple = 15 mos Multiple = 15 Multiple = 15 mos mos • Resection of distant disease can produce long- term survival and cure in selected patients. • Unfortunately, only 20-25% are suitable for resection. Wanger and Adson, Ann Surg. 1984: May; 199(5):502-8 1
5/17/2013 Historical Perspective Improved Mortality Rates Scheele ‘ 91 Author Rosen ‘ 92 N Operative Mortality (%) Gayowski ’ 94 219 6 Arch Surg. 1989 Sep;124(9):1021-2. Review Scheele ‘ 95 280 4 Nordlinger ’ 95 204 0 469 4 Fong ’ 99 1568 2 Belghiti ’ 00 Jamison, ’97 280 4 1001 3 747 4 Hunt M.T., Annals of the Royal College of Surgeons of England (1990) vol. 72, 199-2053 Management of Colorectal Metastases Management of Colorectal Metastases Factors Associated with Recurrence • Stage of primary • Size of metastasis • Timing of liver metastases • Number of metastases • Preoperative CEA 5 yr survival rates remained the same from the 1980 ‘ s- Leonard et al. JCO 2005;23:2038-48 • Level Bilobar disease • Perioperative blood transfusion 2003, and only recently, have the 5 year survival rates • Positive Resection margin now been approaching ~50% with modern chemotherapy. • Extrahepatic disease 2
5/17/2013 Management of Colorectal Metastases Management of Colorectal Metastases Clinical Risk Score* Patient Selection for Hepatectomy 1. Lymph node-positive primary 2. Dz-free Interval < 12 months 3. Size of liver Tumors > 5 cm 4. Number of Liver tumors > one 5. Preop CEA >200 ng/mL *The sum of the positive characteristics is the total score Fong et al. Ann Surg 1999;230:309-18 Fong et al. Ann Surg 1999;230:309-18 Current Management of Colorectal Who Should Undergo Resection? Metastases Fong-Score • Severe co-morbidities • Single (<5cm) • Non – resectable EH Dz • Metachronous (>1year) • Synchronous, Multiple • Favorable primary cancer Bilobar Dz • Low CEA • No tumour – free margin * i.e Low Fong Score • NO RESPONE TO CHEMO • >4 lesions, especially when synchronous • Synchronous liver and lung metastases Unresectable---->Chemo---->Resectable (~15%) • Fong et al. Ann Surg 1999;230:309-18 3
5/17/2013 Definition of Resectability Technical Considerations Ability to remove all gross disease (R0 resection) • and leave an adequate inflow, outflow, and remnant liver volume •Defining Resectability •Methods for Improving Resectability -Portal vein embolization -Two-staged hepatectomy -* ALPPS Procedure--Controversial -Hepatic Arterial Infusion Pump • High quality cross-sectional imaging • Selective 3D rendering and CT volumetrics • FDG PET to rule out more extra hepatic disease Categories of Resectability Management of Colorectal Metastases 1. Initially resectable disease by standard approach 2. Initially resectable but requires extended approach BORDERLINE • staged resections • preoperative portal vein embolization • resection plus RFA or Microwave ALPPS procedure • 3. Initially unresectable but likely convertible with response 4. Initially unresectable and unlikely convertible Adam et al. Ann Surg 2004; 240:644-658 4
5/17/2013 Current Management of Colorectal Conversion Chemotherapy Metastases • Aim: to achieve potentially Resection of the Previously Unresectable curative surgical resection RESPONSE • A correlation between response rate and resection rate is shown. • But for many patients resection will not occur therefore consideration must be given to the continuum of ■ studies/retrospective analyses with non-resectable metastases confined to the liver (‘selected patients’, r = 0.96, P=0.002) care. ▲ Studies with non-selected patients with colorectal cancer. Due to the heterogeneity of these studies, the observed correlation is less strong (r = 0.74, P <0.001, solid line). (phase III trials (filled triangles) were separately analyzed (r = 0.67, P=0.024, dashed line). 1. Folprecht, G., et al. Annals of Oncology, 2005. 16(8): p. 1311-1319. Adam et al. Ann Surg 2004; 240:644-658 Timing of Hepatic Resection Issues with Conversion Chemotherapy 1. Chemotherapy induced hepatotoxicity • Traditional Approach: Two-stage approach – Increases with duration of chemotherapy 1)Colorectal resection (Primary) – Oxaliplatin induced sinusoidal obstruction syndrome >50% 1-2 2) F/b chemo and delayed hepatic resxn. – Irinotecan induced steatohepatitis – Possible association with increased Disadvantage = dz progression of CLM b/w the colorectal perioperative complications 2-5 and hepatic surgery 2. “Disappearing” metastases • Simultaneous resxn of Primary & CLM -Majority contain viable tumour on resection 6-8 , – Disadvantage = increased post-op complications when a - Found in ~25% of patients treated with preop chemo 8 -Approximately 50% are detected during surgery with IOUS 8 major hepatic resection of CLM is performed -True path CR predicted by normalising CEA, inability to detect lesion on MRI 7 • Liver First ( Reverse ) Approach: chemo given Minimize treatment duration upfront f/b hepatic resxn and finally colorectal Surgery as soon as possible 8,9 cancer resection 1. Rubbia-Brandt , L, et al, Ann Oncol. 2004;15(3):460. 2. Soubrane, O., et al, Ann Surg. 2010;251(3):454 3. Aloia, T., et al., Journal of Clinical Oncology, 2006. 24 (31): p. 4983-4990. 4. Vauthey, J.-N., et al., . Journal of Clinical Oncology, 2006. 24 (13): p. 2065-2072. 5. Tamandl, D., et al., Ann Surg Oncol, 2011. 18 (2): p. 421-30. 6. Benoist et Mentha et al. 2006 al, Journal of Clinical Oncology, 2006. 24 (24): p. 3939-3945. 7. Auer, R.C., et al., Cancer, 2010. 116 (6): p. 1502-1509. 8. vanVledder et al J Gastrointest Surg. 2010 Nov;14(11):1691-700. 9 Nordlinger, B., et al., Ann Oncol, 2009. 20 (6): p. 985-92. 5
5/17/2013 Technical Considerations Technical Considerations Metastasis Parenchymal-preserving Resections Right Right hepatic hepatic vein vein •Offer greater technical flexibility •Less extensive resections in patients with limited disease •Bilateral resections in patients with multiple tumors Technical Considerations Technical Considerations Posterior Sectorectomy-(Bisegmentectomy) Central Hepatectomy RHV Resection of segments VI/VII 6
5/17/2013 Methods of Improving Resectability Methods of Improving Resectability Preoperative Portal Vein Embolization 1. Conversion Systemic Chemotherpay 2. Preoperative Portal Vein Embolization 3. Two-Stage Hepatectomy 4. “ALPPS” for Associating Liver Partition and Portal vein Ligation for Staged hepatectomy. 5. HAIP Technical Considerations Technical Considerations Preoperative Portal Vein Embolization PV embolization - regeneration before resection Tumor Before Embolization After Embolization Required resection Normal Portal Vein Post Embolization Left Left Right Right Anticipated liver remnant 7
5/17/2013 Methods of Improving Resectability Technical Considerations Two-Stage Hepatectomy PVE- regeneration before resection Gallbladder Technical Considerations n =25/33 Jaeck et al. Ann Surg 2004; 240:1037-51 Jaeck et al. Ann Surg 2004; 240:1037-51 8
5/17/2013 Technical Considerations Methods of Improving Resectability One year after resection N = 25; 5 centers in Germany 14 patients = metastatic colorectal cancer Jaeck et al. Ann Surg 2004; 240:1037-51 Schnitzbauer et al, 2012 Methods of Improving Resectability Methods of Improving Resectability “ALPPS” -Associating Liver Partition and Hepatic Arterial Infusion Pump Portal vein Ligation for Staged hepatectomy. This procedure leads to explosive hypertrophy of ~ 75% of the Left lat. Seg in ~ 9 days. Kemeny, JCO 23:4888-4896, 2005 de Santibanes and Clavien; 2012 9
Recommend
More recommend