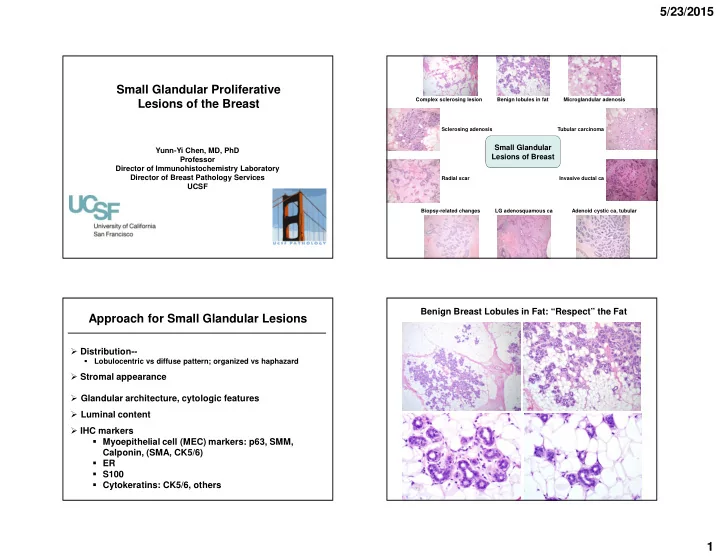
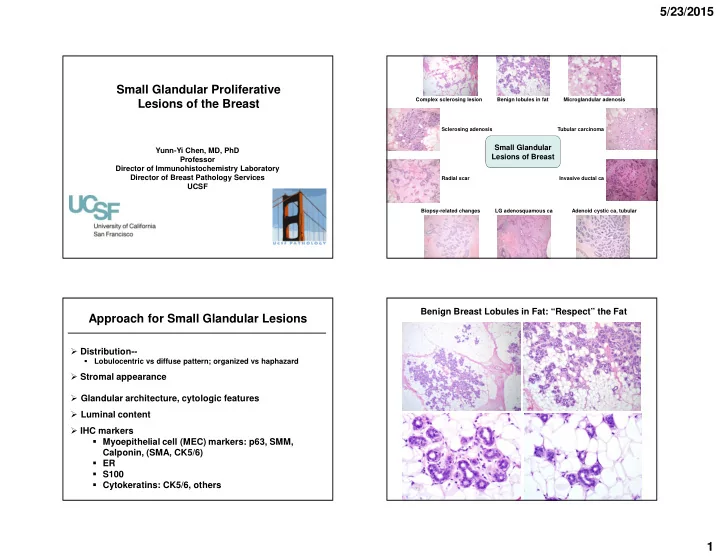
5/23/2015 Small Glandular Proliferative Complex sclerosing lesion Benign lobules in fat Microglandular adenosis Lesions of the Breast Sclerosing adenosis Tubular carcinoma Small Glandular Yunn-Yi Chen, MD, PhD Lesions of Breast Professor Director of Immunohistochemistry Laboratory Director of Breast Pathology Services Radial scar Invasive ductal ca UCSF Biopsy-related changes LG adenosquamous ca Adenoid cystic ca, tubular Benign Breast Lobules in Fat: “Respect” the Fat Approach for Small Glandular Lesions � Distribution-- Lobulocentric vs diffuse pattern; organized vs haphazard � � Stromal appearance � Glandular architecture, cytologic features � Luminal content � IHC markers � Myoepithelial cell (MEC) markers: p63, SMM, Calponin, (SMA, CK5/6) � ER � S100 � Cytokeratins: CK5/6, others 1
5/23/2015 Radial Sclerosing Lesion: “Respect” the Fat Invasive Ductal Carcinoma: Invade the Fat Sclerosing Adenosis (SA) � Lobulocentric � Stroma: collagenous, myxoid � Glands and epithelial cells: � Glands compressed/central, open/peripheral; basement membrane � Luminal epithelial and myoepithelial cells (MEC) � Epithelial cells: flat to cuboidal, bland � Lumen: Calcifications � IHC: Positive MEC markers 2
5/23/2015 Nodular Adenosis Sclerosing Adenosis � Florid sclerosing adenosis, nodular contour � Incidental or mammographic calcifications � Mammographic mass or palpable lesion � Mimic invasion � Also “adenosis tumor” (connotation of neoplasm) � Nodular adenosis � Involved by lobular neoplasia or DCIS � Apocrine cytology � Perineural invasion 3
5/23/2015 Sclerosing Adenosis and Nodular Adenosis Biopsy for Mammographic Mass with Calcifications p63 Nodular adenosis SMM CK5/6 Apocrine Adenosis Lobular Neoplasia Involving SA � Mimic invasive carcinoma � Lobulocentric � MEC markers 4
5/23/2015 Apocrine Adenosis Apocrine Adenosis � SA with apocrine cytology � Eosinophic granular or foamy cytoplasm � Mimic carcinoma � Lobulocentric, MEC markers � Atypical apocrine adenosis Atypical Apocrine Adenosis-- Invasive Apocrine CA Mimicking Apocrine Adenosis 3x nuclear enlargement with prominent pleomorphic nucleoli SMM (O’Malley FP and Bane AL. Adv Anat Pathol 2004) 5
5/23/2015 DCIS with Apocrine Features Apocrine Adenosis � SA with apocrine cytology � Eosinophic granular or foamy cytoplasm � Mimic carcinoma � Atypical apocrine adenosis � 3x nuclear enlargement, prominent pleomorphic nucleoli � Long-term breast cancer risk: not well-defined � On CNB: recommend excision to exclude DCIS � On excision: regular follow-up (Carter D et al: Mod Pathol 1991; Seidman J et al: Cancer 1996; Fuehrer N et al: Arch Pathol Lab Med 2012) CNB for a Palpable Lesion Sclerosing Adenosis with Perineural “Invasion” p63 6
5/23/2015 Sclerosing Lesion with Perineural “Invasion” SMM p63 Radial Scar Peri- and Intraneural “Invasion” in Benign Breast Lesions � Ackerman: 1 st description in 1957 � Taylor and Norris (AFIP): series of 20 patients in 1967 � Incidence: ~2% � Also reported in benign lesions of other anatomic sites � In breast: SA, radial scar, sclerosing papilloma � Pathogenesis unclear : post-traumatic, involvement by the proliferative process 7
5/23/2015 Radial Scar (RS) Radial Scar � Tumor-like or pseudoinfiltrative lesion � Stellate appearance � Mimic malignancy on imaging and pathology � Central fibroelastotic core with entrapped distorted tubules, surrounded by radiating ducts and lobules � Radiating ducts and lobules: variable changes (UDH, papillomatosis, adenosis, apocrine metaplasia, cysts) RS: Fibroelastotic and Hypocellular Center with Entrapped Distorted Glands Radial Scar Invasive Ductal CA 8
5/23/2015 Radiating Ducts and Lobules Entrapped Glands in Fibroelastotic Stroma � Distorted, compressed, angulated � Variable epithelial changes � Luminal epithelial cells: flat to cuboidal � UDH, papillomatosis, adenosis, apocrine metaplasia, cysts � Myoepithelial layer Complex Sclerosing Lesion Radial Sclerosing Lesion (RSL) � Include radial scar and complex sclerosing lesion � Radial scar: Smaller ( ≤ 1 cm) lesions, stellate � Complex sclerosing lesion: larger lesions, more complex and extensive features 9
5/23/2015 Complex Sclerosing Lesion Attenuated Myoepithelial (MEC) Staining in RSL SMM p63 CK5/6 Phenotypic Alterations in Myoepithelial Cells Radial Sclerosing Lesions Associated with Sclerosing Lesions and DCIS � Organized � Expression of MEC markers: reduced or focally absent in various benign sclerosing lesions and DCIS � Stroma: Fibroelastotic � Frequency: � Glands and epithelial cells: � Distorted, compressed, angulated � SMM > p63, calponin > SMA � Radial scar > sclerosing adensois � Luminal epithelial and myoepithelial cells (MEC) � Epithelial cells: flat to cuboidal, bland � Panel of MEC markers � Lumen: Calcifications � Avoid over-diagnosis � IHC: Positive MEC markers � When in doubt about the presence of invasion, diagnose as � Reduced or focally absent for MEC expression non-invasive (Hilson JB et al: Am J Surg Pathol 2009 and 2010) 10
5/23/2015 Tubular Carcinoma-- Tubular Carcinoma-- Diffuse/infiltrative growth Desmoplastic or elastotic stroma Tubular Carcinoma with FEA 11
5/23/2015 Tubular Carcinoma Diagnosing Tubular Carcinoma � Infiltrative � > 90% with tubular morphology � Desmoplastic cellular stroma, ± elastosis � Incompatible features-- � Open round, oval, or angulated tubules Complex architecture � � Cytology Multiple layers of cells � Single layer, non-stratified, cuboidal to columnar cells, Significant nuclear pleomorphism � � prominent cytoplasmic apical snouts Frequent mitoses � Minimal pleomorphism, basally located round to oval nuclei � Mitosis rare � � Lack all MEC markers � Diffusely and strongly positive for ER Diagnosis of TC on CNB?-- Tubular Carcinoma-- Prognosis � IDC may have focal tubular morphology � 10-year survival: ~100% � Dx: Invasive ductal ca with tubular features with a comment � LN metastasis: rare, 1 node, no significant impact on survival � Luminal A ER/PR +, HER2 -, low Ki-67 � 12
5/23/2015 Radial Sclerosing Lesion Tubular Carcinoma-- ddx � Well-differentiated IDC � Radial sclerosing lesions � Microglandular adenosis p63 Distinguishing Pathologic Features for TC and RSL Tubular carcinoma RSL Distribution Infiltrative Lobulocentric Tubular carcinoma Gland size/shape Slightly irregular, Distorted, elongated, angulated flattened Lumen Open Compressed, open Cytology Mild atypia, cuboidal to Bland, flat to cuboidal columnar Luminal content Basophilic secretion; ± ± calc Radial sclerosing lesion calc Stroma Desmoplastic, elastotic, Fibroelastotic, cellular hypocellular Basement memb. - to partial +, complete ME layer Absent Present Background FEA/ADH/DCIS, LN Benign Biomarkers ER diffusely + ER patchy + 13
5/23/2015 Well-differentiated IDC? Well-differentiated IDC? Microglandular Adenosis (MGA) Well-diff IDC Tubular carcinoma Irregular glands Slightly irregular, angulated � Randomly distributed glands � Hypocellular dense collagenous stroma or fat ± Trabeculae and ribbons Open glands � Uniform small round glands, eosinophilic secretion � Cytology Branching and anastomosis No branching or anastomosis Single layer, flat to cuboidal cells, clear to amphophilic (may have cribriform glands) � cytoplasm, bland round nuclei Mild to moderate pleomorphism Minimal pleomorphism � Immunophenotype MEC markers (p63, SMM, calponin, SMA) –; S100 diffusely + Stratified cells, loss of polarity Single layer of cells, basal nuclei � ER - � Laminin and type IV collagen + � Sclerotic to desmoplastic stroma Desmoplastic/elastotic stroma 14
5/23/2015 Microglandular Adenosis-- Microglandular Adenosis-- Hypocellular collagenous stroma Haphazard distribution Microglandular Adenosis Microglandular Adenosis-- calponin SMM Uniform small glands, open lumen, eosinophilic secretion PAS stain p63 Laminin 15
5/23/2015 Distinguishing Pathologic Features for MGA and TC Microglandular Adenosis MGA Tubular carcinoma Distribution Random Infiltrative Gland size/shape Uniform, small, round Slightly irregular, angulated S100 ER Lumen Open Open Cytology Bland, flat to cuboidal Mild atypia, cuboidal to columnar Luminal content Eosinophilic secretion Basophilic secretion; ± calc Stroma Collagenous to fatty Desmoplastic, elastotic, cellular Basement memb. +, complete - to partial ME layer Absent Absent Background Benign FEA/ADH/DCIS, LN Biomarkers ER -, S100 + ER diffusely + CNB for a Palpable Mass Follow-up Lumpectomy Microglandular Adenosis Metaplastic ca Atypical MGA Regular MGA (Courtesy of Dr. Timothy Jacobs) 16
Recommend
More recommend