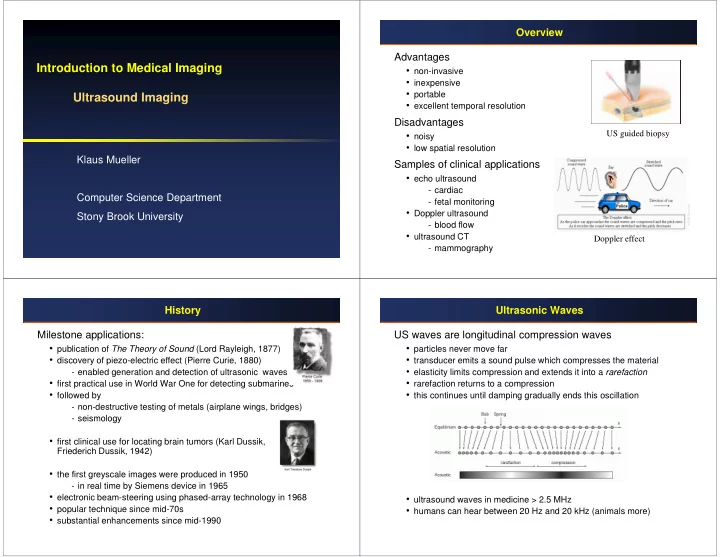
Overview Advantages Introduction to Medical Imaging • non-invasive • inexpensive • portable Ultrasound Imaging • excellent temporal resolution Disadvantages US guided biopsy • noisy • low spatial resolution Klaus Mueller Samples of clinical applications • echo ultrasound - cardiac Computer Science Department - fetal monitoring • Doppler ultrasound Stony Brook University - blood flow • ultrasound CT Doppler effect - mammography History Ultrasonic Waves Milestone applications: US waves are longitudinal compression waves • publication of The Theory of Sound (Lord Rayleigh, 1877) • particles never move far • discovery of piezo-electric effect (Pierre Curie, 1880) • transducer emits a sound pulse which compresses the material • elasticity limits compression and extends it into a rarefaction - enabled generation and detection of ultrasonic waves • first practical use in World War One for detecting submarines • rarefaction returns to a compression • followed by • this continues until damping gradually ends this oscillation - non-destructive testing of metals (airplane wings, bridges) - seismology • first clinical use for locating brain tumors (Karl Dussik, Friederich Dussik, 1942) • the first greyscale images were produced in 1950 - in real time by Siemens device in 1965 • electronic beam-steering using phased-array technology in 1968 • ultrasound waves in medicine > 2.5 MHz • popular technique since mid-70s • humans can hear between 20 Hz and 20 kHz (animals more) • substantial enhancements since mid-1990
Generation of Ultrasonic Waves Wave Propagation Via piezoelectric crystal Two equations • deforms on application of electric field � generates a pressure wave • wave equation: 2 • induces an electric field upon deformation detects a pressure wave ∂ ∆ 1 p 1 2 ∇ ∆ = = p c • such a device is called transducer 2 2 0 ∂ ρ β c t 0 0 s 0 ∆ p: acoustic pressure, ρ 0 : acoustic density , β s0 : adiabatic compressibility • Eikonal equation: 2 2 2 ∂ ∂ ∂ t t t 1 + + = 2 2 2 2 ∂ ∂ ∂ x y z F ( , , ) x y z 1/F: “slowness vector”, inversely related to acoustic velocity v - models a surface of constant phase called the wave front - sound rays propagate normal to the wave fronts and define the direction of energy propagation. Effects in Homogeneous Media Effects in Non-Homogeneous Media (1) Attenuation Reflection and refraction • models the loss of energy in tissue • at a locally planar interface the wave’s frequency will not change, only its speed and angle n e − a f z = H f z ( , ) 0 θ θ θ sin sin sin i = r = t • f : frequency, typically n =1, z : depth, c c c 1 1 2 a 0 : attenuation coefficient of medium, • for c 2 > c 1 and θ i > sin -1 (c 1 /c 2 ) the Non-linearity reflected wave will not be in phase • wave equation was derived assuming that ∆ p was only a tiny when disturbance of the static pressure c 2 θ = − 2 θ cos 1 ( sin ) • however, with increasing acoustic pressure, the wave changes shape t i c and the assumption is violated 1 is complex Diffraction • the amplitude changes as well: T + R =1, Z = ρ v • complex interference pattern greatest close to the source θ θ − θ A 2 Z cos A Z cos Z cos • further away point sources add constructively = t = 1 t = r = 2 i 1 t T R θ + θ θ + θ A Z cos Z cos A Z cos Z cos i 2 i 1 t i 2 i 1 t simulation with a circular planar source
Effects in Non-Homogeneous Media (2) Data Acquisition: A-Mode Scattering ‘A’ for Amplitude • if the size of the scattering object is << λ then get constructive Simplest mode (no longer in use), basically: interference at a far-enough receiver P • clap hands and listen for echo: • if not, then need to model scattering as many point scatterers for a complex interference pattern pulse sent out � echo received ⋅ time expired speed of sound distance = 2 • time and amplitude are almost equivalent since sound velocity is about constant in tissue Problem: don’t know where sound bounced off from • direction unclear small object << λ large object • shape of object unclear • just get a single line Data Acquisition: M-Mode Data Acquisition: B-Mode ‘M’ for Motion ‘B’ for Brightness Repeated A-mode measurement An image is obtained by translating or tilting the Very high sampling frequency: up to 1000 pulses per second transducer • useful in assessing rates and motion • still used extensively in cardiac and fetal cardiac imaging motion of heart wall during contraction blood fetus heart muscle continuous pericardium normal heart
Image Reconstruction (1) Image Reconstruction (2) Filtering Log compression • remove high-frequency noise • brings out the low-amplitude speckle noise Envelope correction • removes the high frequencies of the RF signal • speckle pattern can be used to distinguish different tissue Attenuation correction • correct for pulse attenuation at increasing depth • use exponential decay model Acquisition and Reconstruction Time Doppler Effect: Introduction Typically each line in an image corresponds to 20 cm • velocity of sound is 1540 m/s � time for line acquisition is 267 µ s • an image with 120 lines requires then about 32 ms � can acquire images at about 30 Hz (frames/s) • clinical scanners acquire multiple lines simultaneously and achieve 70-80 Hz
Doppler Effect: Fundamentals (1) Doppler Effect: Fundamentals (2) Received pulse ( N oscillations) 2 c • the duration of the received pulse is ∆ = − = − ∆ t t t ( 1) t R re rb T − c v Assume an acoustic source emits a pulse of N oscillation a N N • writing it as frequencies = = f f within time ∆ t T T R ∆ t ∆ t T R • a point scatterer P s travels at axial velocity v a: − − θ 2 v 2 v cos • the Doppler frequency is then = − = a ≈ a f f f f f D R T T T • the locations of the wave and the scatterer are: = = + c + v c P t ( ) ct ( ) P t d v t b s 0 a a • the start of the wave meets P s at: • to hear this frequency, add it to some base frequency f b d = → = 0 P t ( ) P t ( ) t • finally, to make the range smaller, f d may have to be scaled b ib s ib ib − c v a • the end of the wave meets P s at: + ∆ d c t c Example: = → = 0 T = + ∆ P t ( ) P t ( ) t t t b ie s ie ie ib T − − c v c v • assume a scatterer moves away at 0.5 m/s, the pulse frequency is 2.5 a a • the start of the wave meets the transducer at = MHz, and a base frequency of 5 kHz, then the shift is an audible t 2 t rb ib 5 kHz - 1.6 kHz = 3.4 kHz • the end of the wave meets the transducer at = − ∆ t 2 t t re ie T Doppler: CW Doppler: PW (1) ‘CW’ for Continuous Wave ‘PW’ for Pulsed Wave Compare frequency of transmitted wave f T with frequency of Does not make use of the Doppler principle received wave f R • instead, received signal is assumed to be a scaled, delayed replica of − θ − 2 v 2 v cos • the Doppler frequency is then: the transmitted one a a f = f − f = f ≈ f = π − ∆ D R T T T s t ( ) A sin(2 f ( t t )) + c v c T a ∆ t is the time between transmission and • Doppler can be made audible, where pitch is analog to velocity reception of the pulse it depends on the distance between transducer and scatterer • in fact, we only acquire one sample of each of the received pulses, at t R : = π − ∆ s t ( ) A sin(2 f ( t t )) R T R • now, if the scatterer moves away at velocity v a , then the distance increases with v a T PRF ( T PRF : pulse repetition period) • this increases the time ∆ t (or decreases if the scatterer comes closer)
Doppler: PW (2) Doppler: PW (3) Thus, the sampled sequence s j is: ⋅ 2 v T = − π ⋅ a PRF + s A sin( 2 f ( j ) B ) j T c • therefore, the greater v a , the higher the frequency of the sampled sinusoid: 2 a v = − f f D T c • to get direction information, one must sample more than once per pulse (twice per half oscillation) : Color Flow Imaging: Technique Ultrasound Equipment Calculates the phase shift between two subsequently received pulses ⋅ 2 v T ∆ ϕ = 2 π f ( a PRF ) T c • measure the phase shift by sampling two subsequent pulses at two specific time instances t R1 and t R2 • since this can become noisy, usually the results of 3-7 such samplings (pulses) are averaged Left: Linear array transducer. • divide the acquired RF line into segments (range gates) allows Right: Phased array transducer velocities to be obtained at a number of depths • acquiring along a single line gives a M-mode type display • acquiring along multiple lines enables a B-mode type display commercial echocardiographic scanner red: moving toward transducer blue: moving away from transducer
Ultrasound Applications (1) Ultrasound Applications (2) Left: normal lung, Left: Normal cranial ultrasound. Right: pleural effusion Right: Fluid filled cerebral cavities on both sides as a result of an intraventricular haemorrhage Ultrasound Applications (3) Ultrasound Applications (4) Left: normal liver Right: liver with cyst Left: prostate showing a hypoechoic lesion suspicious for cancer Right: with biopsy needle
Recommend
More recommend