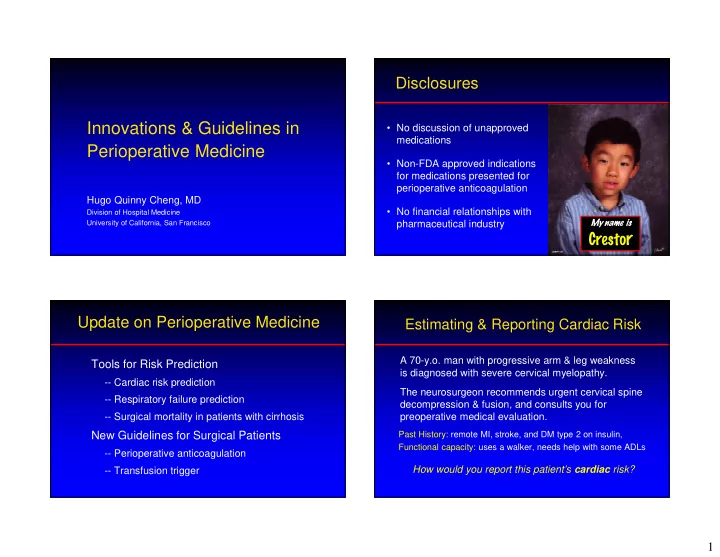
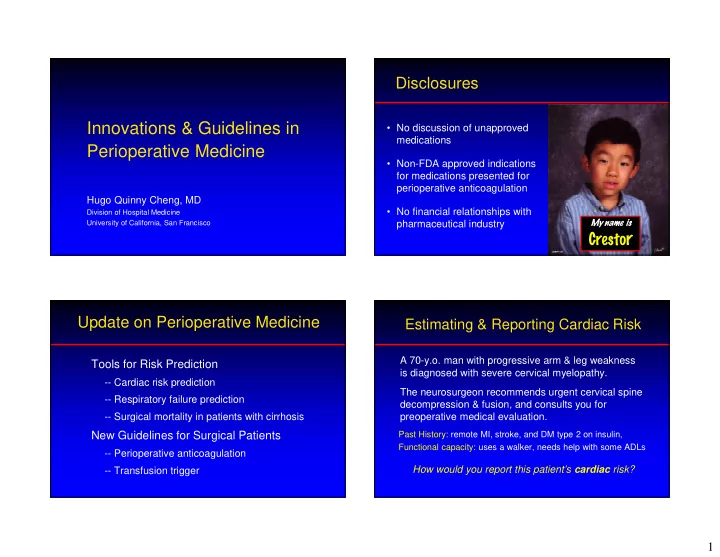
Disclosures Innovations & Guidelines in • No discussion of unapproved medications Perioperative Medicine • Non-FDA approved indications for medications presented for perioperative anticoagulation Hugo Quinny Cheng, MD • No financial relationships with Division of Hospital Medicine University of California, San Francisco pharmaceutical industry My name is Cresto r Update on Perioperative Medicine Estimating & Reporting Cardiac Risk A 70-y.o. man with progressive arm & leg weakness Tools for Risk Prediction is diagnosed with severe cervical myelopathy. -- Cardiac risk prediction The neurosurgeon recommends urgent cervical spine -- Respiratory failure prediction decompression & fusion, and consults you for -- Surgical mortality in patients with cirrhosis preoperative medical evaluation. New Guidelines for Surgical Patients Past History: remote MI, stroke, and DM type 2 on insulin, Functional capacity: uses a walker, needs help with some ADLs -- Perioperative anticoagulation How would you report this patient’s cardiac risk? -- Transfusion trigger 1
70-y.o. with remote MI, stroke, IDDM is undergoing Revised Cardiac Risk Index cervical spine surgery for arm & leg weakness. How would you estimate this patient’s cardiac risk? # of RCRI Complications Predictors: Serious Predictors Any – Ischemic heart disease 1. I use the Revised Cardiac 39% – Congestive heart failure 0 0.5% 0.4% Risk Index (RCRI), so ~ 10% – Diabetes requiring insulin 30% 2. I use the RCRI, so ~ 5% 1 1.3% 1% – Creatinine > 2 mg/dL 3. I use the “NSQIP” prediction 2 4% 2.4% – Stroke or TIA tool, so ~ 1% 17% 13% ≥ 3 9% – “High Risk” operation 4. My gut says surgery will be 5.4% like “death-on-a-stick” (intraperitoneal, intrathoracic, Any : MI, cardiac arrest, complete or suprainguinal vascular) heart block, pulmonary edema . . . . . . . . . . . . i R I Q u v s e C S Serious : MI & cardiac arrest R R N s y “ e e a h h e s t t h t e e t u s s e g u u u s y I I M I Devereaux PJ et al. CMAJ 2005; 173:627. New Cardiac Risk Prediction Tool ASA Class (a brief digression) Derived from National Surgical Quality Improvement American Society of Anesthesiologists Physical Program (NSQIP) database: Classification • > 400 K patients in derivation & validation cohorts 1. Healthy, normal • Wide range of operations 2. Mild systemic disease • “Complication” = 30-day incidence of MI & cardiac arrest 3. Severe systemic disease Independent 4. Severe systemic disease that is a constant threat to life 1. Type of surgery Predictors 5. Moribund patient not expected to survive without surgery 2. Age 3. Serum creatinine > 1.5 mg/dL Death-on-a-Stick TM 4. Functional status (dependency for ADLs) 5. American Society of Anesth (ASA) class Gupta PK et al. Circulation 2011; 124:681 2
70-y.o. with h/o remote MI, stroke, IDDM undergoing cervical spine surgery. Needs help with some ADLs. NSQIP Cardiac Risk Calculator Age 70 Cr < 1.5 ASA Class 3 Partially dependent Spine surgery www.qxmd.com/calculate-online/cardiology/gupta-perioperative- www.qxmd.com/calculate-online/cardiology/gupta-perioperative- cardiac-risk cardiac-risk 70-y.o. with h/o remote MI, stroke, IDDM undergoing Which Prediction Tool is Better? cervical spine surgery for progressive weakness. RCRI NSQIP 0.72% Sample size ~4000 ~400,000 www.qxmd.com/calculate-online/cardiology/gupta-perioperative-cardiac-risk # of hospitals 1 > 200 Other findings: Currency of data ’89 −’94 ’07 − ’08 • Excellent performance (AUC = 0.88) Performance (AUC) 0.75 0.88 • MI/Cardiac arrest strongly predicts mortality (61% vs . 1%) Screen for MI? CK-MB, ECG No Guideline Adoption ACC/AHA None Caveats: • Didn’t look at all possible variables (e.g., TTE, stress test) 3
Respiratory Failure Prediction Tool 2007 ACC/AHA Guideline yes Good Functional Capacity? Go to OR • Derived from National Surgical Quality Improvement Program (NSQIP) database: no or ? • > 400 K patients in derivation & validation cohorts • Wide range of operations no predictors* 1 or 2 predictors ≥ 3 predictors • “Respiratory Failure” = on vent > 48 hrs or reintubation no Vascular surgery? Independent 1. American Society of Anesth (ASA) class yes Predictors 2. Functional status (dependency) Go to OR Consider stress test Control HR & 3. Type / location of surgery or if results will change go to OR (IIa) 4. Emergency surgery (IIb) management (IIa) 5. Preoperative sepsis or SIRS * CAD, CHF, DM, CKD, CVA/TIA Gupta PK et al. Chest 2011; 110:1207 70-y.o. with h/o remote MI, stroke, IDDM undergoing 70-y.o. man with h/o MI, stroke, IDDM having spine surgery for cervical spine surgery for progressive weakness. progressive weakness. Non-emergent 3.01% ASA Class 3 www.qxmd.com/calculate-online/respirology/postoperative-respiratory-failure-risk-calculator Other findings: • Excellent performance (AUC = 0.9) Partially dependent • Respiratory failures strongly predicts mortality (25% vs . 1%) Spine surgery Caveat: No sepsis/SIRS • Didn’t look at all possible variables (e.g., OSA, VTE, PFTs) www.qxmd.com/calculate-online/respirology/postoperative- respiratory-failure-risk-calculator 4
Surgical Risk in Cirrhotic Patients 65-y.o. man with cirrhosis from HCV desires a hip arthroplasty. He’s asymptomatic and has no signs of encephalopathy or ascites. A 65-y.o. man with cirrhosis from HCV desires a hip arthroplasty. He feels well and has no current signs 58% 1. Patients with cirrhosis are not of ascites or encephalopathy on examination. candidates for elective surgery 42% 2. Your mild cirrhosis (Childs-Pugh Labs: Creatinine = 1.6 class A) makes you an acceptable Total Bilirubin = 1.9 surgical candidate Albumin = 3.5 3. Perioperative risk is acceptable, INR = 1.6 but long-term mortality risk makes surgery unappealing 0% How would you advise this patient about his perioperative mortality risk? . . . . . . . . . r h r e t i v i c w t i d a s i l r t m e n p e r o i u t i a o r Y e P P Surgical Risk in Cirrhotic Patients MELD Score as Risk Predictor Question: How does his cirrhosis affect mortality risk? MELD Score (Model for Endstage Liver Disease): Background: • Main use in organ allocation • Risk traditionally assessed by Childs-Pugh classification • Variables: INR, bilirubin, creatinine ( http://www.mdcalc.com/child-pugh-score-for-cirrhosis-mortality) Retrospective multivariate analysis of 772 cirrhotic • Mortality after GI surgery: Class A = 10% patients undergoing GI, orthopedic, and CV surgery Class B = 30% • Predictors of mortality: Age, MELD Score, ASA Class IV Class C = 70% • Predicts mortality @ 1 wk, 1 mo, 3 mo, 1 yr, 5 yr • Limitations: single time point, less known about non-GI www.mayoclinic.org/meld/mayomodel9.html surgery; sensitive to minor laboratory result differences Teh et al. Gastroenterology, 2007 5
65 y.o. man with stable HCV-related cirrhosis. He has Managing Perioperative Anticoagulation no current signs of encephalopathy or ascites. Your orthopedic colleague asks your advice on how to manage Labs: Creatinine = 1.6 anticoagulation in two patients who had hip fractures. Childs-Pugh Class A Total Bilirubin = 1.9 One has atrial fibrillation due to HTN � Albumin = 3.5 The other has a mechanical AVR MELD Score = 19 � INR = 1.6 Neither has any other relevant comorbidity � Mortality Prediction: 1. Heparin bridge for AVR only 57% • Childs-Pugh: 10% in-hospital mortality 2. Heparin bridge for AF only 29% 3. Heparin bridge for both • MELD Score: 6.5% 1 week mortality 4. Heparin bridge for neither 24% 1 month mortality 7% 7% 36% 3 month mortality y y h r l l e n n o t h o o b i t R F r e V A o n f A r r 50% 1 year mortality r o e o o f g f f e d e g i g e r d g d b d r i n i r i b b r r i b n a n n i p i r e a r r i a H p a p p e e e H H H Thromboembolic Risks with Thromboembolic Risks with Atrial Fibrillation Mechanical Valves CHADS-2 Score: 1 point for CHF, HTN, Age>75, Diabetes Annual Stroke Risk Annual Incidence 2 points for Stroke/TIA Score 0 - 2: < 5% annual stroke risk Score 3 - 4: 5-10% Score 5 - 6: > 10% Ansell J. Chest. 2004;126:204S-233S. Cannegieter, et al. Circulation , 1994 6
Recommend
More recommend