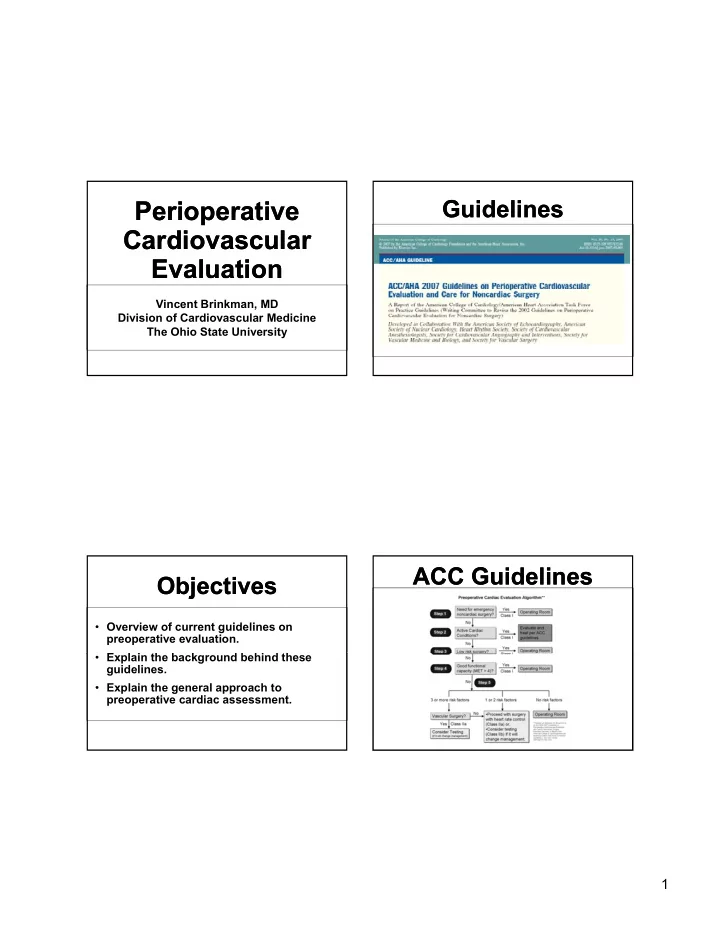
Perioperative Perioperative Guidelines Guidelines Cardiovascular Cardiovascular Evaluation Evaluation Vincent Brinkman, MD Division of Cardiovascular Medicine The Ohio State University ACC Guidelines ACC Guidelines Objectives Objectives • Overview of current guidelines on preoperative evaluation. • Explain the background behind these E l i h b k d b hi d h guidelines. • Explain the general approach to preoperative cardiac assessment. 1
ACC Perioperative ACC Perioperative Active Cardiac Conditions Active Cardiac Conditions Guidelines Guidelines • Unstable Angina • Or Recent Myocardial Infarction • • Decompensated heart failure Decompensated heart failure • Class IV heart failure • Unstable arrhythmias • Uncontrolled heart rate, heart block, Ventricular Tachycardia... • Severe valve disease ACC Perioperative ACC Perioperative Active Cardiac Conditions Active Cardiac Conditions Guidelines Guidelines • Treat these according to ACC guidelines • Cardiology consultation • In other words: Does this patient require further treatment of their cardiac condition in the absence of this surgery? 2
ACC Perioperative ACC Perioperative Low Risk Surgery Low Risk Surgery Guidelines Guidelines Major Morbidity and Mortality Within 1 Month of Ambulatory Surgery and Anesthesia Mark A. Warner, MD; Sondra E. Shields, MD; Christopher G. Chute, MD, DrPH • 45,000 Procedures • 14 Myocardial Infarctions • 2 Cardiac Deaths • 17.8 Myocardial Infarctions expected ACC Perioperative ACC Perioperative Risk of Surgery Risk of Surgery Guidelines Guidelines Risk Stratification Examples Vascular Aortic and other major peripheral vascular surgery Risk more than 5% Intermediate Risk Intraperitoneal or intrathoracic surgery Carotid endarterectomy Risk 1% to 5% Head and Neck Surgery Orthopedic surgery Prostate surgery Low Risk Endoscopic procedures Superficial procedures Risk less than 1% Cataract surgery Breast surgery Ambulatory surgery 3
ACC Perioperative ACC Perioperative Functional Capacity Functional Capacity Guidelines Guidelines • Reliable way to determine cardiovascular risk of surgery. • Can be determined with history 1 MET Getting Dressed Walking around the house < 4 METs Light house work > 4 METs Walk on level ground at 4 mph Climb 1-2 flights of stairs Heavy house work Based on the Duke Activity Status Index Risk Factors Risk Factors Functional Capacity Functional Capacity Self-reported Exercise Tolerance and the Risk of • History of ischemic heart disease Serious Perioperative Complications • Prior history of heart failure Dominic F. Reilly, MD, et al. Archives of Internal Medicine 1999 • Diabetes • Renal Insufficiency • 600 patients undergoing “major” surgery. • Cerebrovascular Disease • Poor functional tolerance defined as inability to climb 2 flights of stairs or walk 4 blocks. Based on the “Revised Cardiac Risk Index” • Serious complications inversely related to the number of blocks one could walk. Derivation and Prospective Validation of a Simple Index for Prediction of Cardiac Risk of Major Noncardiac Surgery; Thomas H. Lee, MD, et al., Circulation 1999 4
Step Five Step Five Step Five Step Five • No risk factors • 1-3 risk factors had increasing cardiac � Even among highest risk surgeries, events during surgery. absence of risk factors predicted a low incidence of events incidence of events. Derivation and Prospective Validation of a Simple Index for Prediction of Cardiac Risk of Major Derivation and Prospective Validation of a Simple Index for Prediction of Cardiac Risk of Major Noncardiac Surgery; Thomas H. Lee, MD, et al., Circulation 1999 Noncardiac Surgery; Thomas H. Lee, MD, et al., Circulation 1999 Step Five Step Five Step Five Step Five 5
Why Vascular Surgery? Why Vascular Surgery? Intermediate Risk Patients Intermediate Risk Patients • Highest cardiovascular risk • Most studied in terms of cardiac risk • High risk patient population • Older patient population • 1,500 patients undergoing vascular surgery (700 intermediate risk). • All patients received beta blockers with goal of heart rate less than 65 bpm. • Patients randomized to stress testing or proceeding with surgery. • If extensive ischemia found, patients underwent revascularization. Should Major Vascular Surgery Be Delayed Because of Preoperative Cardiac Testing in Intermediate-Risk Patients Receiving Beta-Blocker Therapy With Tight Heart Rate Control? Don Poldermans, et. al, JACC 2006 Stress Tests Stress Tests Intermediate Risk Intermediate Risk Functional assessment • Multiple studies show that risk of cardiac events increases as the extent of ischemia increases. • Fixed defects (ie. Prior scar with no inducible ischemia) confer no additional • No significant difference between stress increased risk. testing and beta blocker treatment groups Should Major Vascular Surgery Be Delayed Because of Preoperative Cardiac Testing in Intermediate-Risk Patients Receiving Beta-Blocker Therapy With Tight Heart Rate Control? Don Poldermans, et. al, JACC 2006 6
Step Five Step Five Does Does Revascularization Revascularization Revascularization Revascularization Help? Help? Can the surgery be delayed? Timing of Surgery Timing of Surgery CARP Trial CARP Trial • 510 patients with CABG PCI “stable,” significant CAD Balloon Bare Metal Drug Eluting randomized to Angioplasty Angioplasty Stent Stent Stent Stent CABG or medical CABG di l therapy before vascular surgery. Two Weeks One Month One Year of • No difference in of Aspirin of Aspirin Aspirin and survival. and Plavix and Plavix Plavix Coronary-Artery Revascularization before Elective Major Vascular Surgery Edward O. McFalls, M.D., Ph.D., et al., NEJM 2004 7
Revascularization Revascularization Beta Blockers Beta Blockers Before Surgery Before Surgery • Controversial • Does not appear to offer any significant � Historically, studies have shown benefit benefit except in those patients that would in reducing mortality and cardiovascular require it independent of surgery. require it independent of surgery. events events. • However, jury is still out . . . � Wide variation in type, dose and timing of beta blockers in previous studies. Class I Indications for Revascularization � May not be class effect •3 vessel disease •Left main disease or left main equivalent •High risk unstable angina •ST elevation MI Medical Therapy Medical Therapy POISE Trial POISE Trial • 8351 patients with or at risk for CAD undergoing • Statins non-cardiac surgery. • Aspirin • Randomized to metoprolol or placebo. • Decreased incidence of myocardial infarctions, � Probably does not need held for surgery. but increased stroke and mortality. y � May increase bleeding, but not mortality or severity of • Criticisms bleeding • Plavix • Beta blockers started immediately before surgery • Single dosing (100mg of sustained release metoprolol). � Conflicting evidence – No titration � Some evidence that stopping 5 days before surgery may reduce risk of major bleeding events. • Sepsis / hypotension / stroke Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial; POISE Study Group, The Lancet 2008. 8
Summary Summary POISE Trial POISE Trial Summary • Beta blockers are not indicated for everyone undergoing surgery • Dose titration and initiation prior to surgery may be necessary Pre-op Beta Blockers Pre-op Beta Blockers Preoperative Preoperative • Class I Indications: Pulmonary Evaluation Pulmonary Evaluation � Beta blockers should be continued in patients who are receiving beta blockers to treat angina arrhythmias or to treat angina, arrhythmias or hypertension. Jennifer McCallister, MD • Class II Indications: Assistant Professor The Ohio State University Medical Center � Beta blockers titrated to heart rate and blood pressure control are reasonable in high risk patients 9
Objectives Objectives Importance of PPC Importance of PPC • Incidence 2-19% in non-thoracic surgery 1 • Review types of postoperative pulmonary • Morbidity & mortality similar to cardiac complications (PPC) complications 2 complications • Describe risk factors for PPC • Better predict mortality 3 • Discuss strategies for risk factor • May double hospital length of stay 4 assessment 1. Fisher et al, 2002. Am J Med;112(3):219. 2. Smetana et al, 2006. Ann Int Med;144(8):581. 3. Manku et al, 2003. Anesth Analg;96:583. 4. Lawrence et al, 1995. J Gen Int Med;10(12):671. Types of post-op pulmonary Types of post-op pulmonary Preoperative Pulmonary Evaluation Preoperative Pulmonary Evaluation complications (PPC) complications (PPC) • “Preoperative clearance” • Atelectasis � Implied permission, all-or-none • Pneumonia • Identification of risk factors • Respiratory failure/prolonged mechanical R i t f il / l d h i l � Patient-related ventilation � Procedure-related • Exacerbation of chronic underlying • Risk assessment pulmonary disease • Post-operative risk reduction or • Death modification 10
Recommend
More recommend