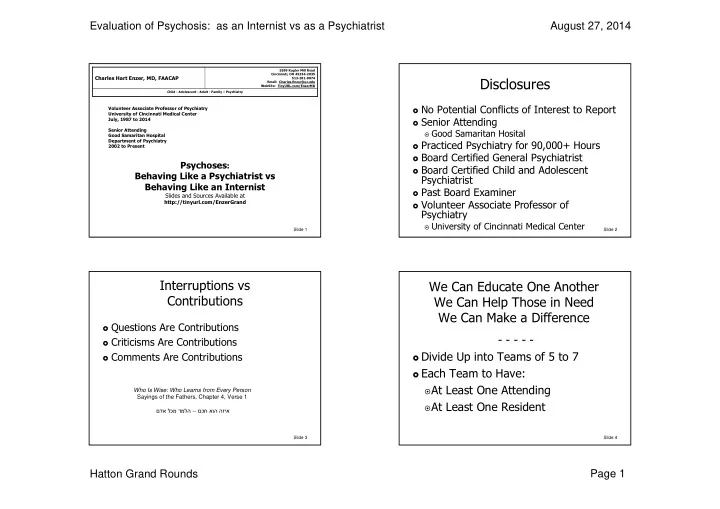
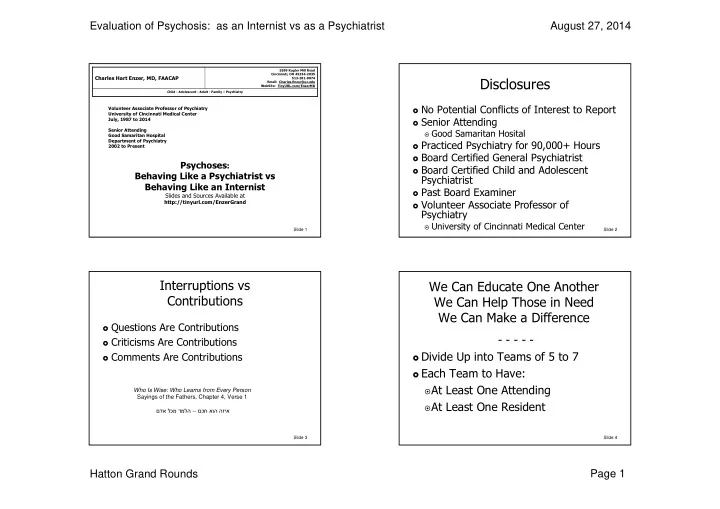
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 5599 Kugler Mill Road Cincinnati, OH 45236-2035 Charles Hart Enzer, MD, FAACAP Disclosures 513-281-0074 Email: Charles.Enzer@uc.edu WebSite: TinyURL.com/EnzerMD Child - Adolescent - Adult - Family – Psychiatry � No Potential Conflicts of Interest to Report Volunteer Associate Professor of Psychiatry University of Cincinnati Medical Center � Senior Attending July, 1987 to 2014 Senior Attending � Good Samaritan Hosital Good Samaritan Hospital Department of Psychiatry � Practiced Psychiatry for 90,000+ Hours 2002 to Present � Board Certified General Psychiatrist Psychoses : � Board Certified Child and Adolescent Behaving Like a Psychiatrist vs Psychiatrist Behaving Like an Internist � Past Board Examiner Slides and Sources Available at � Volunteer Associate Professor of http://tinyurl.com/EnzerGrand Psychiatry � University of Cincinnati Medical Center Slide 1 Slide 2 Interruptions vs We Can Educate One Another Contributions We Can Help Those in Need We Can Make a Difference � Questions Are Contributions - - - - - � Criticisms Are Contributions � Divide Up into Teams of 5 to 7 � Comments Are Contributions � Each Team to Have: � At Least One Attending Who Is Wise: Who Learns from Every Person Sayings of the Fathers, Chapter 4, Verse 1 � At Least One Resident םכח אוה הזיא -- םדא לכמ דמלה Slide 3 Slide 4 Hatton Grand Rounds Page 1
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 You See: Violent Movement of Extremities Entering the Room, You Hear Prolonged with Clench Fists Screaming with Gasping Inhalations Your Next Step ? ? ? ?? Your Next Step ? ? ? ?? Slide 5 Slide 6 1- 31 Year Social Worker 4- Recent Anxiety Attacks FBS = 94 mg/dL 3 Hour = 15 mg/dL 2- Long Standing Apathy 5- Recent Impotency 1 Hour = 74 mg/dL 4 Hour = 64 mg/dL 3- Authority Conflicts 6- Recent “Immaturity” 2 Hour = 53 mg/dL 5 Hour = 51 mg/dL Your Next Step ? ? ? ?? What is Your Assessment ? ? ? ?? Slide 7 Slide 8 Hatton Grand Rounds Page 2
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 Man 38: Athletic, Self-Confident, Disciplined, Creative Until Findings and Course 11 years Ago Became restless and nervous 2 Years Ago � Hypopituitarism Personality Change, Depressions, Anxieties and Stress Stomach � Insulin Producing Lesions in Abdomen What Would Have Been Your Next Step ? ? ? ?? [11] � Surgical Treatment Slide 9 Slide 10 After Many Medical Consultations, Started Psychoanalysis About a Half Year Later Petite Mal Hours Later, Grand Mal Seizure One Year Later Still Healthy Looking Irritable, Melancholy, Complained of a Loathsome, Severe Photophobia Loneliness Repulsive Smell What Would Have Been Your Next Step ? ? ? ?? [11] What Would Have Been Your Next Step ? ? ? ?? [11] Slide 11 Slide 12 Hatton Grand Rounds Page 3
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 He Had Many Exams and then 3 Days in Hospital Working Assessment: Hysteria == Somatization Disorder Normal Physicals & Severe Photophobia Petite Mal with Attempt to Push Chauffer out of Car Neurologicals Petite Mal with Smearing Gift Chocolates as a Cream over Body Normal Skull Films Normal Labs What Would Have Been Your Next Step ? ? ? ?? [11] What Would Have Been Your Next Step ? ? ? ?? [11] Slide 13 Slide 14 1- 78 Yr Man: Hallucinations 4- Dizziness Course 2- Headache: Dull, Frontal, 5- Unsteady Gait Continuous � Admitted to Prestigious Los Angeles Hospital 3- Malaise 6- Agitated � Opening Spinal Pressure of 400 mm What Is Your Next Step ? ? ? ?? � One Cell � Colorless � Protein 30 mg � Pressure Lowered 400 � 220 mm � Doctor Harvey Cushing in Baltimore Called � 24 Hours Later, Neurosurgery Begun � 3.5 Hours Later Tumor Located � 3.5 Days after Admission, Dies of Pleocytic Astrocytoma [38] Slide 15 Slide 16 Hatton Grand Rounds Page 4
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 Strange Behavior, Mood Changes, What Is Hunger ? ? ? ?? Abnormal Thinking Are Symptoms of [23] A Physical Symptom 1. Medical Disorders 1. A Psychological 2. Toxic Disorders 2. Symptom 3. Psychiatric Both 3. Disorders Neither 4. 4. Medical & Toxic 5. Toxic and Psych. 6. All of the Above 0% 0% 0% 0% 0% 0% 0% 0% 0% 0% 1 2 3 4 1 2 3 4 5 Slide 17 6 Slide 18 What Type of Symptom Is Pain � Strange Behavior ? ? ? ?? � Mood Changes � Abnormal Thinking A Physical Symptom 1. A Psychological 2. - These Are Symptoms of Psychoses - Symptom Both 3. � Whether Physical Psychoses Neither 4. � Or � Functional – Psychiatric - Psychoses 0% 0% 0% 0% 1 2 3 4 Slide 19 Slide 20 Hatton Grand Rounds Page 5
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 Percent of Psychiatric Patients Having Undiagnosed Physical 58% of Psychiatric Patients Have Illnesses? Physical Illnesses Undiagnosed [23] 0 – 20% - - - - 1. 21 – 40% 2. 21 Studies 41 – 60% 3. 61 – 80% 4. 81 – 100% 5. 0% 0% 0% 0% 0% 1 2 3 4 5 Slide 21 Slide 22 Percent of Physical Disorders Producing Symptoms Related Directly to the � 27% of the Physical Disorders “Psychiatric Symptoms” ? ? ? ?? � of Psychiatric Patients 0 – 20% 1. � Produced Symptoms Related 21 – 40% 2. Directly to the “Psychiatric 41 – 60% 3. Symptoms” [23] 61 – 80% 4. 81 – 100% 5. - - - - 0% 0% 0% 0% 0% 1 2 3 4 5 Slide 23 Slide 24 Hatton Grand Rounds Page 6
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 Non-Psychiatric Physicians Miss the Physical Disorders of Referred Patients � Non Psychiatric Physicians How Often ? ? ? ?? � Miss Physical Diagnoses 0 – 20% 1. � In about 30% of Patients 21 – 40% 2. 41 – 60% 3. � They Refer for Psychiatric 61 – 80% 4. Treatment [23] 81 – 100% 5. 0% 0% 0% 0% 0% 1 2 3 4 5 Slide 25 Slide 26 How Often Do Psychiatrists Miss the Physical Disorders of Their Patients ? ? ?? � Psychiatrists � and Psychiatric Institutions 0 – 20% 1. � Missed the Physical Disorders 21 – 40% 2. 41 – 60% 3. � In about 50% of Patients [23] 61 – 80% 4. 81 – 100% 5. 0% 0% 0% 0% 0% Slide 27 Slide 28 1 2 3 4 5 Hatton Grand Rounds Page 7
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 How Often Do Non-Physicians Miss Physical Diagnoses in Patients � Non-Physicians They Refer ? ? ? ?? � Psychologists � Social Workers 0 – 20% 1. � Therapists 21 – 40% 2. 41 – 60% � Patients 3. 61 – 80% 4. � Relatives 81 – 100% 5. � Miss about 86% of Physical Disorders [23] 0% 0% 0% 0% 0% Slide 29 Slide 30 1 2 3 4 5 Among Patients w/ “Psychiatric Physical Disorders Missed by Symptoms”, Why Are Physical Disorders Referral Source: Missed ? ? ? ?? � 18% of These Physical Disorders Caused Symptoms � 31% Coincided with the Psychiatric Morbidity � 51% of These Physical Disorders Aggravated Psychiatric Morbidity [23] Slide 31 Slide 32 Hatton Grand Rounds Page 8
Evaluation of Psychosis: as an Internist vs as a Psychiatrist August 27, 2014 Physical Disorders Are Missed by Why Are Physical Disorders Missed Medical Physicians: so often by Psychiatrists: � We Do Incomplete Histories � Same as for Medical Physicians � Psychiatrist Sees the Physical Not of Concern � We Do Incomplete Examinations � Fail to Ask “What Else May be Going on” � Overt Psychosis or Poor Hygiene Put Us Off � Dislike Doing Physical Examination � We and Patient Communicate Poorly � Fear Litigation Examining Women � Using Language Level above 6th Grade � Elderly May Take too Long to Undress � Patient Doesn’t Feel Safe Note: � Patient Focuses on Consequences – Not Sx Women and Elderly Have Significantly � Don’t Sort Sx: Medical from Mood or Behavior Higher Rates of Undiagnosed Disorders. [23] � See Consultation Merely to r/o Reasons against Meds [23] Slide 33 Slide 34 Making a Diagnosis Nonetheless � Years Ago, Diagnoses Were Made at � Numerous Studies: Bedside � Psychiatric Patients Have � History and Physical Examination Were � a Greater Susceptibility Key � to Medical Disorders � Tests and Studies Were Confirmatory � The Non-Psychiatric Portion � Today, Technologies Have Blossomed � of the Charts of Psychiatric Patients � Physicians Choose What Tests to Run � Weigh Significantly More than the Charts of � Tests Are Viewed as Making the Other Patients Diagnosis [42] Slide 35 Slide 36 Hatton Grand Rounds Page 9
Recommend
More recommend