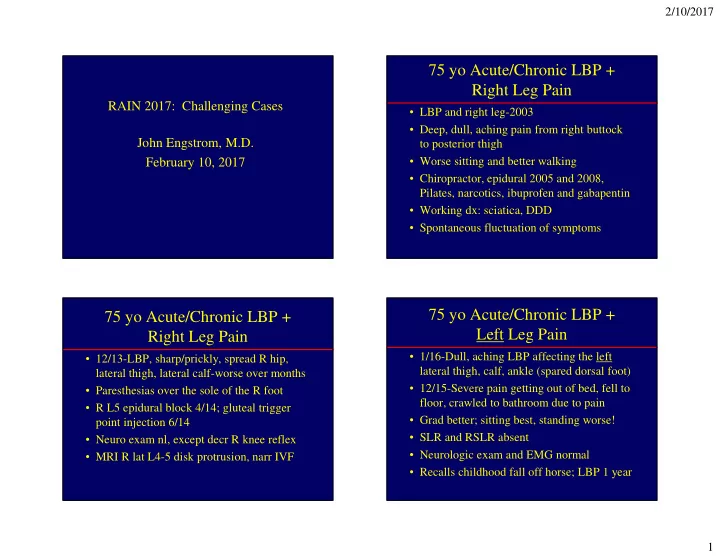
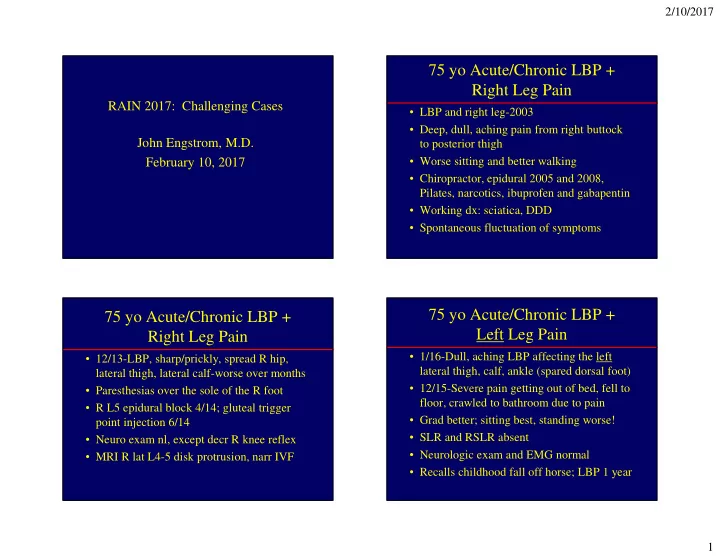
2/10/2017 75 yo Acute/Chronic LBP + Right Leg Pain RAIN 2017: Challenging Cases • LBP and right leg-2003 • Deep, dull, aching pain from right buttock John Engstrom, M.D. to posterior thigh February 10, 2017 • Worse sitting and better walking • Chiropractor, epidural 2005 and 2008, Pilates, narcotics, ibuprofen and gabapentin • Working dx: sciatica, DDD • Spontaneous fluctuation of symptoms 75 yo Acute/Chronic LBP + 75 yo Acute/Chronic LBP + Left Leg Pain Right Leg Pain • 1/16-Dull, aching LBP affecting the left • 12/13-LBP, sharp/prickly, spread R hip, lateral thigh, calf, ankle (spared dorsal foot) lateral thigh, lateral calf-worse over months • 12/15-Severe pain getting out of bed, fell to • Paresthesias over the sole of the R foot floor, crawled to bathroom due to pain • R L5 epidural block 4/14; gluteal trigger • Grad better; sitting best, standing worse! point injection 6/14 • SLR and RSLR absent • Neuro exam nl, except decr R knee reflex • Neurologic exam and EMG normal • MRI R lat L4-5 disk protrusion, narr IVF • Recalls childhood fall off horse; LBP 1 year 1
2/10/2017 Q1-75 yo with LBP and Leg Pain Postural LBP (worse with flexion or extension) and leg pain is least likely to be from which of the following anatomic causes? A. Lumbar radiculopathy 62% B. Spondylolisthesis C. Facet arthropathy with facet joint fluid 16% 13% 9% D. Mild lumbar scoliosis s s y i i h s s t e . . o a h . f i p l s t h o o i t c l l i s u o w r c y l a i y b d d h a n t m r o a r p u a p l S o d b r m h i l t M u r L a t e c a F Q2-75 yo with LBP and Leg Pain What is the nl anatomic pathway for a lumbar motor nerve cell from proximal to distal? A. Conus to cauda equina to intervertebral foramen (IVF) to lateral recess 74% B. Conus to lateral recess to cauda to IVF C. Conus to cauda to lateral recess to IVF to extraforaminal space 18% 8% D. Cauda to lateral recess to IVF 0% . . . . . . . . . . . l . o o t a t s t s r s a e e s n t c a e u i e c l e q r o e l t r a l r a a a e d d r u t u e a t a l a a c l c o o t o o t t s t u s a s u d u n n o n u o o C a C C C 2
2/10/2017 75 yo Acute/Chronic LBP + Leg Referred Pain Pain-Interpret/Localize History • 1893 – Described by Sir Henry Head • Pain quality-Not neuropathic • “Sclerotomal” pain-a correct, but clinically impractical concept – Dull, deep, and achy in 2014 – Sharp and achy in 2016; not electrical/burning • Splenic rupture-pain in the left shoulder • Location-Pain switched sides (R to L) • Angina-pain or paresthesias in neck/left arm and exacerbating positions (from sitting • Vast majority of referred pain occurs in a to standing/walking)! less predictable pattern and varies from • Pseudodermatomal-sole of foot person to person paresthesias; lateral calf sparing dorsal foot 3
2/10/2017 The Challenge of Referred Pain Q3-75 yo with LBP and Leg Pain from the Facet Joints What would be your next management step? • How do facet joints cause pain? – Compress the adjacent nerve root in foramen A. Refer for multidisciplinary chronic pain – Inflamed joint swells with fluid (“mechanical stress”) 44% management may cause axial back pain +/- leg pain B. Repeat the lumbar spine MRI 28% • Can you identify the precise anatomic source of C. Perform lumbar flexion-extension x-rays referred pain? Usually not 14% 13% D. Repeat the EMG • Facet blocks useful, but imperfect-no sham block • We need an imaging ligand for pain G . . . . M . . . . r . e E a n - n i n e i p l s o h p i t i r x t c a e a s b l i f e d m r p i a t u e u l b R l m m e h u r t l o t m f a e r r o e p f e f e r R R e P Extension Flexion-Extension Spine X-rays • To search for “dynamic instability” of spine – Movement of one vertebral body on another that changes alignment between flexion and extension of the neck or low back – Listhesis-misalignment of vertebral bodies on another-with or without dynamic instability • Anterolisthesis-anterior displacement • Posterolisthesis-posterior displacement 4
2/10/2017 Sag T2 Circumstances in Which to Consider Flexion-Extension Spine X-rays L4-5 Facet • Chronic LBP without radiculopathy that is L4-5 synovial cyst worse/better in sitting or standing positions L5 root • Fluid in facet joints at levels commonly L4 L4-5 Facet S1 root prone to movement (L4-5 > L5-S1) L5 L4-5 synovial cyst • Cervical stenosis without abnormal cord signal but with myelopathic signs L5 root • Prior MVA or traumatic spine injury S1 root Coronal T1 L4 Define Spondylolysis L4 lateral recess L5 root L4 root • Spondylolysis-multiple micro fractures in S1 root the pedicles of either L4 or L5 (usually L4) L4-5 facets L5 root L4 root • Congenital predisposition-6% adolescents S1 root L4-5 synovial cyst • Common in teenage athletes-back pain in a teenager is a “different” entity L4-5 lateral disc extrusion L4-5 synovial cyst • Can lead to complete fractures through pars interarticularis disconnecting the anterior vertebral body from posterior elements L4 root 5
2/10/2017 Spondylolisthesis Possible Consequences of Lumbar Spondylolisthesis • Diagnosis: L4-5 spondylolisthesis with dynamic instability and referred pain to legs • Postural low back pain +/- leg pain • Spondylolisthesis-Slippage of one vertebral • L4 or L5 radic from nerve root tension body on another depending on the level/severity of the slip – Fixed-does not change on flexion-extension • Cauda equina syndrome when segmental – Dynamic instability-movement of vertebral movement occurs at a level of severe spinal bodies on one another in flexion or extension stenosis (rare) – Patients may describe a specific point in time • Bridging osteophytes can stabilize segment when symptoms are suddenly worse 75 yo-L4-5 Spondylolisthesis, Dynamic Lumbar Spondylolisthesis-Where Instability and Pain Referred to Legs Does the Pain Come From? • Degenerative spondylolisthesis-Abnormal • Spine surgery procedure motion/inflammation at the facet joints – Fusion L4-5 • Isthmic spondylolisthesis-Abnormal motion • Bone autograft for long term spine stabilization at fractured pars defect • Fusion instrumentation at L4 and 5 • Motion of the vertebral body on the disk at – Posterior L4-5 laminectomy the affected segment-periosteum or annulus – Seen by me in follow-up 5 months later and 11 • L4/L5 root stretching with radicular pain months later (last 12/16) – Pain resolved • Combination of the above 6
2/10/2017 75 yo with LBP and Leg Pain-Patient Take Home Points Perspective on Functional Outcome • Location (dermatomal?), quality (burning, • “Don’t just think of me as your ‘chronic electric), and position dependency of back pain patient’; know I want my life back.” and leg pain matter • “I can now walk/exercise as I want to.” 3 • Consider symptomatic spondylolisthesis miles/day-stops from fatigue, not pain when position dependency is not explained • “I can garden; no longer all on gardener.” by nerve root compression Bends, prunes, up/down from ground easily • Use flexion-extension x-rays to search for • “I am funny again.” Active social life now, dynamic instability of the spine not when living with chronic pain 7
Recommend
More recommend