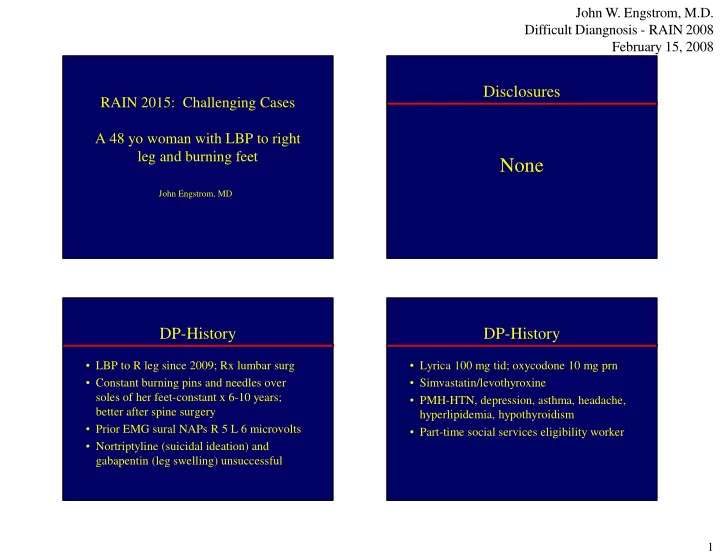
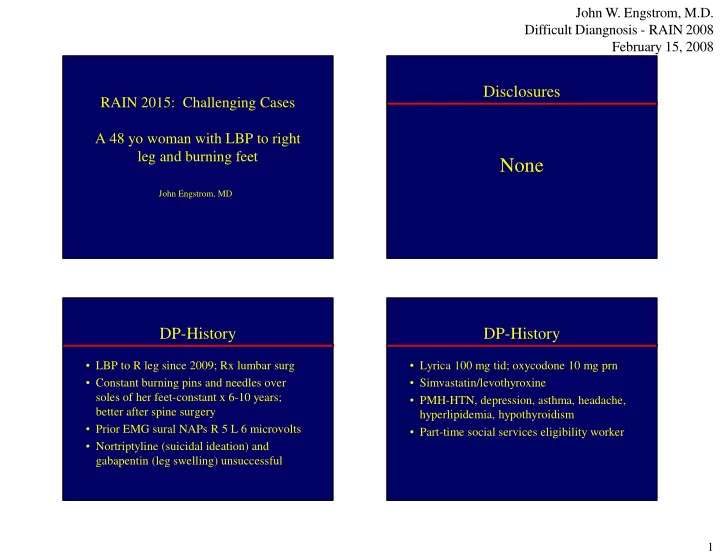
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Disclosures RAIN 2015: Challenging Cases A 48 yo woman with LBP to right leg and burning feet None John Engstrom, MD DP-History DP-History • LBP to R leg since 2009; Rx lumbar surg • Lyrica 100 mg tid; oxycodone 10 mg prn • Constant burning pins and needles over • Simvastatin/levothyroxine soles of her feet-constant x 6-10 years; • PMH-HTN, depression, asthma, headache, better after spine surgery hyperlipidemia, hypothyroidism • Prior EMG sural NAPs R 5 L 6 microvolts • Part-time social services eligibility worker • Nortriptyline (suicidal ideation) and gabapentin (leg swelling) unsuccessful 1
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Q1-What is your working diagnosis DP-Examination based on the presented exam findings? • BP 157/90; Afebrile; P70, reg; Wt 267 lbs A. Distal symmetric polyneuropathy B. Erythromelalgia 68% • Mental status and cranial nerves-normal C. Distal symmetric small fiber • Motor-normal bulk, tone, coordination, gait polyneuropathy • Power-nl foot plantar flexion, eversion, and D. Burning feet syndrome dorsiflexion; great toe dorsiflexion 13% 12% E. Syringomyelia 4% 3% • Reflexes-2+, including ankle reflexes • Sens-LT/pos nl; Pin decr mid-calves bilat Erythromelalgia Syringomyelia Burning feet syndrome Distal symmetric polyn... Distal symmetric small fi... DSFPN-unmyelinated and thinly Distal Small Fiber Polyneuropathy myelinated sensory and autonomic fibers • Na chan mut-Nav 1.7-inher erythromelalgia • Idiopathic • Big 3: Vasculitis, Sarcoid, Lymphoma • Glucose intol or Rx-induced; HgBA1c, hx • Hepatitis • Alcohol abuse; hx…occult hx • Hereditary-AIP, Fabry’s Dz, HSAN1 • HIV; HIV Antibody • Meds-discuss alternative medications • MGUS-SPEP/IEP • -Anti-retrovirals (ddC,ddI,d4T); • -Leflunomide, chloramphenicol 2
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Q2-Which one of the following DP-More History statements is true? • Her primary care physician told her the A. The decreased pin sensation probably reflects loss of sensory neurons symptoms are probably from diabetes 92% B. The preservation of some pin sensation • Patient: “How can I have both burning feet reflects the preserved function of sensory + decreased sensation to pin? Am I crazy?” neurons C. The burning sensation reflects the • Your credibility is on the line dysfunction of sensory neurons 7% D. All of the above 1% 0% e . . . . v . . . . e . o t f b a m e r a s o n n s e e o h f s o i t t n a f i n o p s o n i l l d t e A e s a s v g a r n e e i r s n c e e r r u d p b e e e h h h T T Q3-What is most impt to add to The Weak Patient: Key Evaluation Features her neurologic exam? Power Reflexes Sensation A. Funduscopic exam � or normal AHC Patchy normal 58% � or normal � * � or normal Nerve Root (i.e. - Radiculopathy) B. Flexion of the toes � distal � distal � distal Nerve-Axonal (i.e. – DSPN) C. Repeat ankle reflexes � diffuse � diffuse � patchy/ normal Nerve - Demyelination (i.e. - GBS) � proximal NMJ (i.e. -Myasthenia) normal normal 23% D. Her exam is complete (+/- bulbar) 11% 9% � proximal Muscle(i.e. - Polymyositis) normal normal m s s e e e t a o x e x e l * - in distribution of affected root t p e e f l e m c h i t r o p c o f e o l s c k i s n n u m o a d i a n x t e a x u e e F l F p r e e R H 3
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 DP-Labs DP-Exam and EMG • CRP 35.7 (< 6.3 nl); ESR 47 • SSA/B negative; cANCA/pANCA negative • Toe flexors are 5 in power bilaterally • SPEP/IEP normal • Sens nerve conduction studies (microvolts) • RF 47 (mildly inc) CH50 58.1 (elevated), – Sural R 4; L 7 • Cr 1.17 (eGFR 49); UA esterase + – Superficial peroneal R 4; L no response • ALT 19, AST 23, Alk phos 85, T bili 0.7 • Tibial and peroneal motor NCS normal • ANA + > 640, mixed; anti-DS DNA neg • Needle EMG of distal leg muscles normal • Hep B/C serologies negative DP-More History/Lab Q4-Which statement is true? • No arthritis, photosensitive skin rash, Raynaud’s phenomenon A. The patient has systemic vasculitis • No dry eyes/mouth; no asthma, sinusitis 85% B. The patient has lupus • No genital ulcers; 1 episode of oral apthous C. The patient has rheumatoid ulcers in last year arthritis • Cryoglobulins negative D. The labs need to be correlated 10% • Polyarthralgia (knees, shoulders, ankles) 3% with other clinical symptoms and 2% signs • A diagnostic test was performed s . u . . . . p o . . . u t r c a r i l o m s m c a e u e h t e b s t h y o s n r e t s s a t i a d h a h e p e t t e n n n e h e s i b t i T t a a a l p p e e e h h h T T T 4
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 DP-Right Sural Nerve Bx Results • Perivascular/intramural inflam consisting of plasma cells and CD3-positive lymphocytes • Inflammatory infiltrate invades walls of multiple arterioles • No fibrinoid necrosis seen • Immunohistochemical stains for plasma cell neoplasm negative • Diagnosis: Small vessel vasculitis Q5-What is most common pattern seen on Nonsystemic Vasculitic Neuropathy neuro exam in vasculitic polyneuropathy? A. Mononeuropathy multiplex • ¼ of vasculitic neuropathy B. Distal symmetric polyneuropathy • Fever, weight loss uncommon 63% C. Mononeuropathy • Indolent, not fatal if untreated 30% D. Demyelinating polyneuropathy • May treat with steroids +/- cytotoxic drug • Average duration of symptoms 11 years! 5% 2% • 10% go on to systemic vasculitis y x e . h l . t . p . . e a . i n p r t u l y o e u r m o l n u p e y y l c n o h o p r i t n a t g p e o n m M o i r t m a u n e y i n s e l o a l y n m t o s M i e D D 5
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 DP-Course Take-Home Points • Rx with prednisone (60mg/d initially with • Vasculitic neuropathy often presents with taper to 10 mg/d now) an apparent symmetric pattern on neuro • Azathioprine (200 mg/d) x 2 months exam, but NCVs reveal asymmetries • Pain with neuropathy better; cont Lyrica • Routine screen for treatable causes of • Prednisone keeps her awake; on taper polyneurop should include CRP and ESR • CRP 14.5 • Search for disorders assoc with vasculitis • Nonsystemic vasculitic neuropathy • Nerve biopsy characterizes the nature of the – Yes: indolent course over 6+ years! infiltrate and type of vessels affected – No: arthralgias; renal insuff; serologic markers 6
Recommend
More recommend