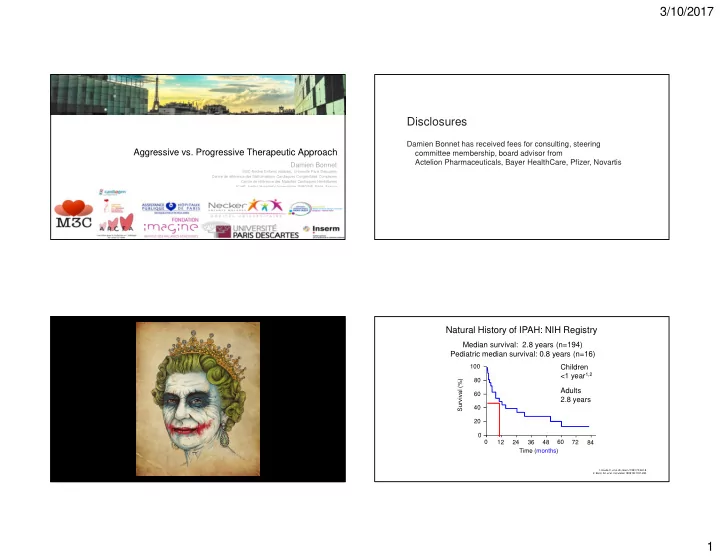
3/10/2017 Disclosures Damien Bonnet has received fees for consulting, steering Aggressive vs. Progressive Therapeutic Approach committee membership, board advisor from Actelion Pharmaceuticals, Bayer HealthCare, Pfizer, Novartis Damien Bonnet M3C-Necker Enfants malades, Université Paris Descartes Centre de référence des Malformations Cardiaques Congénitales Complexes Centre de référence des Maladies Cardiaques Héréditaires ICarP, Institut Hospitalo-Universitaire IMAGINE, Paris, France Natural History of IPAH: NIH Registry Median survival: 2.8 years (n=194) Pediatric median survival: 0.8 years (n=16) 100 Children <1 year 1,2 80 Survival (%) Adults 60 2.8 years 40 20 0 0 12 24 36 48 60 72 84 Time (months) 1. Houde C, et al. Br Heart J 1993;70:461-8. 2. Barst, RJ, et al. Circulation 1999; 99:1197-208. 1
3/10/2017 Improved survival in pediatric PH Initial treatment in the TOPP1 registry This improvement occurred with mono therapy with off label use of drugs approved in adults Barst R, et al. Circulation 1999; 99:1197-208. Fraisse et al. ACVD 2010 Humpl T et al. CiTY 2016 Van Loon, et al, Am J Cardiol, 2010. iPAH/fPAH and CCB treatment Differences in survival of PAH in children according to cause First, treat your patient with drugs adapted to their hemodynamic profile n (brackets) and predicted survival over 5 years are shown. Douwes M et al. JACC 2016 Haworth SG, et al. Heart 2009; 95:312-7. 2
3/10/2017 Survival of adults with Eisenmenger syndrome according to Immortality bias in Eisenmenger syndrome type of lesion Standardised mortality ratio 3.8; 95% CI 2.0 – 7.0; p<0.0001 Diller et al EHJ 2006 Survival of patients with Eisenmenger syndrome according Individual susceptibility for the time course of PVR increase to type of lesion and age at diagnosis of PH ASD-PAH > 40y Prevalent cases Incident cases ASD-PAH < 40y Van Loon, et al. Am J Cardiol, 2010. Hascoet S et al. ACVD 2017 3
3/10/2017 RCTs with monotherapy in PAH Sequential combination therapies in RCTs Improvement in exercise capacity (3-4 months) Pbo-adjusted effect of sequential combo therapy on primary EP (6MWD) Epoprostenol Treprostinil Iloprost Bosentan Ambrisentan Sildenafil Tadalafil + 26 m Drug tested Background Placebo-corrected effect on 6MWD (m) p=0.051 (IPAH) (PAH-SSc) (AIR) (BREATHE-1) (AERIES) (SUPER-1) (PHIRST) 80 STEP ILO BOS Active treatment + 20 m 60 PACES SIL EPO + 28.8 m p=0.01 Change in 6MWD (m) p<0.001 TRIUMPH Inh TREP ERA or PDE5i 40 FREEDOM Oral TREP ERA &/or PDE5i 20 0 + 11 m + 10 m -20 p=0.072 p=0.089 Control* -40 Treatment effect + 47 m + 108 m* + 18 m + 36 m + 44 m + 44 m + 42 m + 44 m # p < 0.003 < 0.001 0.005 0.004 0.0002 < 0.001 < 0.001 < 0.001 N=64 N=277 N=235 N=350 N=310 * Control = placebo except for epoprostenol trials (‘Conventional therapy’) #: monotherapy only 1. McLaughlin VV , et al. AJRCCM 2006. 2. Simonneau G, et al. Ann Intern Med 2008. Barst, NEJM 1996. Simonneau, AJRCCM 2002. Rubin, NEJM 2002. Galiè, NEJM 2005. 3. McLaughlin VV, et al. J Am Coll Cardiol 2010. 4. Tapson V, et al. Chest 2012. 5. Tapson V, et al. Chest 2013. Badesch, Ann Int Med 2000. Olschewski, NEJM 2002. Galiè, Circulation 2008. Galiè, Circulation 2009. Meta-analyses have provided conflicting evidence on combination therapy SERAPHIN primary end-point according to pretreated status Naive patients Pretreated patients ComboRx MonoRx RR 95%-CI W Risk reduction 55% Risk reduction 38% Study Events Total Events Total (random) 100 100 PHIRST-1b 2 42 1 45 2.14 [0.20; 22.77] 12.1% TRIUMPH-1 4 115 6 120 0.70 [0.20; 2.40] 29.8% Freedom from event (%) PACES 10 134 36 133 Freedom from event (%) 80 Macitentan 10 mg 80 Macitentan 10 mg STEP 0 34 5 33 0.28 [0.14; 0.53] 49.4% Random 0.09 [0.01; 1.53] 8.8% 60 60 effects model 16 325 48 331 0.42 [0.17; 1.04] 100% Placebo 40 40 Placebo Heterogeneity: I-squared = 38.2%, p = 0.1829 0.1 0.5 1 2 10 20 20 Difference between arms 10 mg Difference between arms 10 mg Favours Favours Hazard ratio (HR) 0,45 Hazard ratio (HR) 0,62 p (test Log-rank) 0,009 p (test Log-rank) < 0,001 combination therapy monotherapy 0 0 0 6 12 18 24 30 36 0 6 12 18 24 30 36 Months since initiation of treatment Months since initiation of treatment A meta-analysis of 6 short-term RCTs could not show a beneficial effect of sequential Patients at risk Patients at risk 88 74 68 64 58 38 17 154 134 119 107 97 53 24 96. 66 54 45 42 24 13 154 122 106 90 80 40 combination therapy on a combined clinical worsening endpoint 10 Fox BD, et al. Am J Cardiol 2011; 108:1177-82. Pulido T, et al. N Engl J Med 2013; 369:809-18. 4
3/10/2017 Case 1 Risk assessment in pulmonary arterial hypertension Enzo 3.5 years old male referred for syncope at school while running No personal or family history of PH No overt heart failure CT no argument for PVOD RHC PAP 129/86-103 mmHg PAo 85/50-65 mmHg PWp 7 mmHg Rap: 6 mmHg CI 4.3 L/min/m 2 Non responder to NO° NT-proBNP : 350 ng/L What would you do ? Galie N et al. Eur Respir J 2015; Galie N et al. Eur Heart J 2016. Pediatric PAH Treatment Goals Evidence-based treatment algorithm Combination therapy and interventional procedures LOWER RISK DETERMINANTS OF RISK HIGHER RISK No Clinical evidence of RV failure Yes No Progression of symptoms Yes No Syncope Yes Growth Failure to thrive I,II WHO functional class III,IV Significantly elevated, Minimally elevated BNP / NTproBNP rising syst CI > 3.0 L/min/m 2 syst CI < 2.5 L/min/m 2 mPAP/mSAP < 0.75 mPAP/mSAP > 0.75, rising Level of evidence C Hemodynamics RAP > 10mmHg PVRI > 20 WU*m 2 Acute Vasoreactivity Echocardiography Severe RV dysfunction, PE > 450 m, stable 6MWD ≤ 350m (> z-2 ; % predicted) (if ≥ 8 yr and developmentally able) decreasing Galiè N, et al. ESC/ERS Guidelines Eur Heart J. 2015. 5
3/10/2017 How to treat this patient ? Case 1-Follow-up Treated with PDE5i + ERA WHO-FC I NT-proBNP 32 ng/L TAPSE 22 mm RVEF 45% RHC after 6 months PAP 70/30-45 mmHg mPWp 7 mmHg PAo 116/60-83 mmHg PVRi decreased from 23 to 6.2 WU.m 2 6 weeks after treatment initiation Escalate therapy at time of clinical worsening Clinical worsening as composite study endpoint or disease progression in pediatric PAH Event-free survival of 6 endpoint combinations Only the first occurrence of endpoint components are incorporated as events Component 1 = death Component 2 = lung-transplantation Clinical Clinical Component 3 = non-elective PAH-related hospitalization Baseline Good ! Good ! worsening worsening Component 4 = initiation of intravenous prostanoid Component 5A = functional deterioration (defined as worsening of WHO-FC only) Component 5AB = functional deterioration (defined as worsening of WHO FC 6 months and/or ≥ 15 % decrease in 6-MWD) CW-endpoint = Full composite clinical worsening endpoint consisting of death, lung- transplantation, non-elective PAH related hospitalization, initiation of intravenous First line Continue Escalation Continue prostanoids and functional deterioration. therapy first line therapy escalated therapy therapy Ploegstra MJ et al. Eur Respir J 2015. 6
Recommend
More recommend