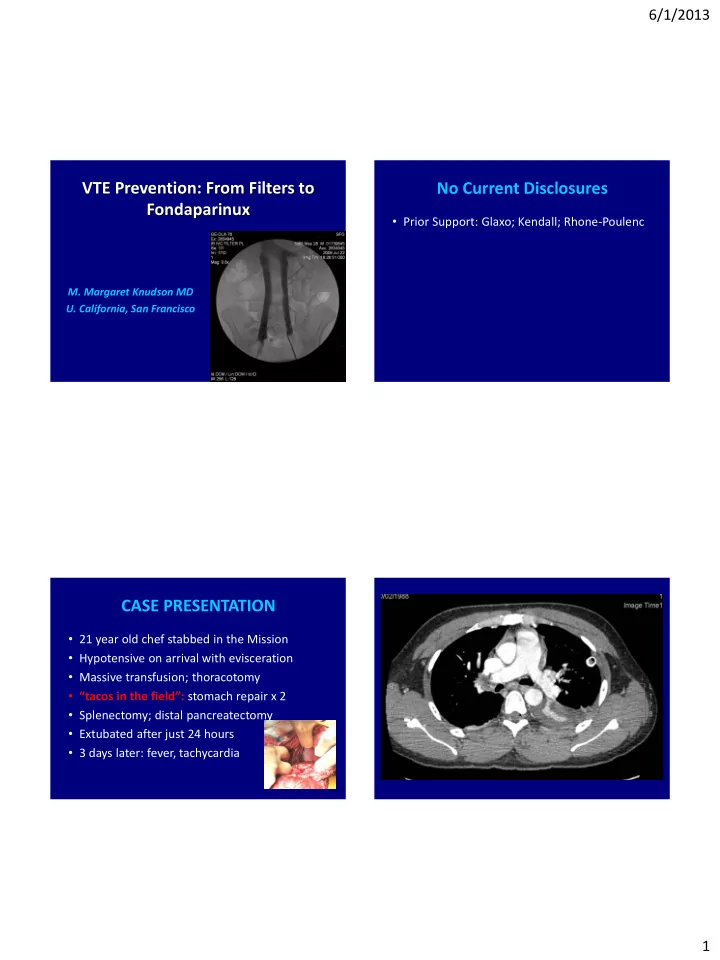
6/1/2013 VTE Prevention: From Filters to No Current Disclosures Fondaparinux • Prior Support: Glaxo; Kendall; Rhone-Poulenc M. Margaret Knudson MD U. California, San Francisco CASE PRESENTATION • 21 year old chef stabbed in the Mission • Hypotensive on arrival with evisceration • Massive transfusion; thoracotomy • “tacos in the field”: stomach repair x 2 • Splenectomy; distal pancreatectomy • Extubated after just 24 hours • 3 days later: fever, tachycardia 1
6/1/2013 Case Presentation Continued • Full-dose anticoagulation with heparin • Lower GI bleed with drop in Hematocrit • Transfused; IVC Filter placed • Prophylatic doses of enoxaparin • Eventually transitioned to Coumadin Historical Perspectives Historical Perspectives “ A study of protocols of 9,882 postmortem exams • 124 trauma patients: venograms including death from injury…in the traumatic • Fracture patients: 35% venous thrombosis group embolisms were found in 61 cases(3.8%) • Thrombus found within 24 hours of injury and in the non-traumatic group in 222 cases (2.6%). Statistically, this appears to be a • Both injured/uninjured extremity significant difference.” • 2/3rds with DVT-asymptomatic Freeark et al, 1967 J.S. McCartney, 1934 2
6/1/2013 Incidence of Occult PE after INCIDENCE: OCCULT DVT Trauma • 349 injured patients: screening venography* • 90 consecutive patients; ISS> 9 • None receiving prophylaxis • Asymptomatic; no DVT • Proximal DVT rate: 18% • Chest CT: between 3-7 days • PE rate: 2% (43% mortality!!) • 22 had clot on CT; 4 were major! • 30% were receiving prophylaxis * Geerts et al, NEJM 1994 Schultz et al J Trauma 2004 METHODS THROMBOEMBOLISM AFTER TRAUMA AN ANALYSIS OF 1602 EPISODES FROM THE ACS NATIONAL • Data source: NTDB (1994-2001) TRAUMA DATA BANK Annals of Surgery 2004 • Data analysis: - Demographics M. Margaret Knudson MD Danagra G. Ikossi MD - Nature/severity of injuries Linda Khaw BA Diane Morabito RN, MPH - Complications/outcomes Larisa S. Speetzen BA • Survey: participating trauma centers The University of California, San Francisco - VTE risk factors/protocols 3
6/1/2013 RISK FACTOR ANALYSIS RESULTS • 450,375 patients included Risk Factor * Odds Ratio • 84% blunt injuries Shock on admission (BP < 90 mHg) 1.95 • 31% ISS>10 Age > 40 yrs. 2.29 • 998 pts: DVT (0.36%) Head injury (AIS > 3) 2.59 • 522 pts: PE (0.13%) • 82 pts: both DVT/PE Pelvic fracture 2.93 • PE mortality: 18.7% Lower extremity fracture 3.16 Spinal cord injury with paralysis 3.39 * Greenfield 1997, 2000; Knudson 1994, 1996 p < .0001 for all factors MULTIVARIATE ANALYSIS RISK FACTOR ANALYSIS (CONT’) Risk Factor Odds Ratio Risk Factor Odds Ratio Head injury (AIS 3) 1.24 Major surgical procedure 4.32 Major operative procedure 1.53 Lower extremity fracture (AIS 3) 1.92 Venous injury 7.93 Age 40 years 2.01 Ventilator days > 3 10.62 Venous injury 3.56 Ventilator days > 3 8.08 p < .0001 for all factors p 0.0125 for all factors 4
6/1/2013 PROPOSED ALGORITHM “APPEARANCES ARE DECEPTIVE”* Injured Patient High Risk Factor VERY High Risk Factor (OR for VTE = 4-10) (OR for VTE = 2-3) • Age ≥ 40 • Major operative procedure • Pelvic fx • Venous injury • Lower extremity fx • Ventilator days > 3 • Shock • 2 or more high risk factors • Spinal cord injury • Head trauma (AIS ≥ 3) Contraindication for heparin? No Yes Contraindication for heparin? Mechanical compression Yes No LMWH* and *Critical Evaluation of Vena Cava Plication: and serial CFD mechanical Bergen et al . Arch Surg 1964 OR temporary Mechanical LMWH* compression IVC filter compression *Prophylactic dose Historical Perspectives IVC Plication • IVC Ligation: post-op edema/ulceration • 1850 : Rudolph Virchow described PE • IVC Ligation: Sudden hypotension! • Recognized origin in femoral/pelvic veins • IVC Plication: absorbable sutures: • 1910 : Trendelberg ligated IVC for PE unpredictable • 1948 : Only 48 cases • 1964 : IVC Clip of IVC ligation 5
6/1/2013 “Filter Fever” IVC Filters: Indications • Recurrent VTE despite adequate anticoagulation • Documented VTE but with contraindications to anticoagulation • Complications while on anticoagulation Greenfield: Textbook of Surgery From Filter Fever to Filter Failure Prophylactic Vena Cava Filters? • Problems: • Technical - Recurrent PE: 3% • Timing - No protection against DVT • Truth - 10%: caval thrombosis • Trievable (as in Re) - permanence: leg edema • Tale - migration/IVC perforation - timing: 6% PE within 24 hours 6
6/1/2013 TIMING TRUTH Independent Risk Factors Odds Ratios • PE-occurs within 24 hours of injury: 6%* Head Injury (AIS>3) 1.24 • PE-seen on CT on day 1: 38%** Major Operation 1.53 • Early PE: highest in patients with fractures Lower Extremity Fx (AIS>3) 1.92 • For filter to be effective: placement in ED? Age > 40 years 2.01 Venous Injury 3.56 Ventilator Days >3 8.08 *Owens 1997 **Scalea 2007 Knudson et al: Analysis of 1602 Episodes of VTE; NTDB. Annals of Surgery, 2004 7
6/1/2013 TRUTH: PART II Retrievable Filters: “NOT” • May be retrieved within 5 days • 3,883/450,375: IVC FILTERS • May be left in place: 30 days? • 86%: PROPHYLACTICALLY • Solution for high risk patients? • Leads to 3-fold increase use • 410 PATIENTS: NO RISK FACTOR! • AAST study: >400 patients • Only 22% were retrieved! • $100,000/ PE prevented Antevil J Trauma 2006 Karmy-Jones J Trauma 2007 Hospital-Specific Risk Factors for Filter FICTION FEVER (AS IN “PULP”) Fever • 263 Northern California Hospitals • Frequency of VCF for VTE varied widely • Risk of getting a filter for acute VTE: -Admission to Rural Hospital -Admission to small hospital -Admission to private hospital -Not admitted to Kaiser JAMA 2013 8
6/1/2013 Fondaparinux Fondaparinux For The Prevention Of • Synthetic, non-heparin polysaccharide Venous Thromboembolism In High-risk • Long half life: once-daily dosing Trauma Patients • Excreted unchanged by kidney • Effective in orthopedics and general surgery • Previously untested in trauma J.P. Lu, MD and M. Margaret Knudson U. Of California, San Francisco Mechanism Of Action Study Objectives • To evaluate the efficacy and safety of • Binds to antithromin III, which inactivates factor fondaparinux for DVT prophylaxis in trauma Xa, preventing thrombin formation patients • To implement a VTE prevention protocol based on stratified risk factors • To measure Fondaparinux anti Xa activity in trauma patients 9
6/1/2013 Hypotheses Methods • Subjects: consecutive trauma admissions • VTE rate would be less than 5% in high-risk • Inclusion criteria: trauma patients with Fondaparinux – Age > 18 – Risk factor for VTE • Fondaparinux would NOT cause bleeding – Anticipated hospital stay > 5 days • Exclusion criteria: • Anti-Xa activity would be therapeutic – Prisoners – Pregnant women Proposed Algorithm Protocol Injured Patient High Risk Factor VERY High Risk Factor • Enrollment after (OR for VTE = 2-3) (OR for VTE = 4-10) consent • Age ≥ 40 • Major operative procedure • Ultrasound on • Pelvic fx • Venous injury • Lower extremity fx • Ventilator days > 3 admission and Q 5-7 • Shock • 2 or more high risk factors days • Spinal cord injury • Included both upper • Head trauma (AIS ≥ 3) Contraindication for heparin? and lower extremities • Fondaparinux within 36 No Yes Contraindication for heparin? Mechanical hours compression Yes No FND and and serial CFD mechanical OR temporary Mechanical FND: 2.5mg compression IVC filter compression 10
6/1/2013 Results: Enrollment Results: Risk Factors Enrolled Patient, n = 106 80 65% 70 No fondaparinux fondaparinux 60 n=17 n=89 Percentage 47% 50 40 5 1 5 76 25% 30 20% 19% 12 5 17% 20 2 7% 10 No 0 fondaparinux fondaparinux Major Age>40 LE Fx SBP<90 Mech Pelvic Fx Venous n=81 Operation Vent>72hr injury excluded n=6 excluded DVT risk factor n=2 n=12 excluded after late crossover n=5 Results: Incidence Of DVT Results: Incidence Of DVT 33.3% 33.3% 35 35 30 30 25 25 20 20 % % 15 15 10 10 2.5% 2.5% 5 5 0 0 fondaparinux No fondaparinux fondaparinux No fondaparinux 2/81 2/6 2/81 2/6 11
6/1/2013 Results Results: Anti Xa Activity • 2 DVTs in Fondaparinux: 1 with PIC line; 1 on 0.4 initial scan prior to receiving drug* 0.35 0.3 0.3 0.25 • No bleeding associated with Fondaparinux mg/L 0.2 0.15 • No thrombocytopenia 0.1 0.05 0.05 0 Trough Peak • No other major AEs identified *intent to treat Fondaparinux levels Summary • Fondaparinux has several advantages: – No risk of HIT – Once daily dosing: improves compliance – Cost effective • No major bleeding episodes or AEs 12
Recommend
More recommend