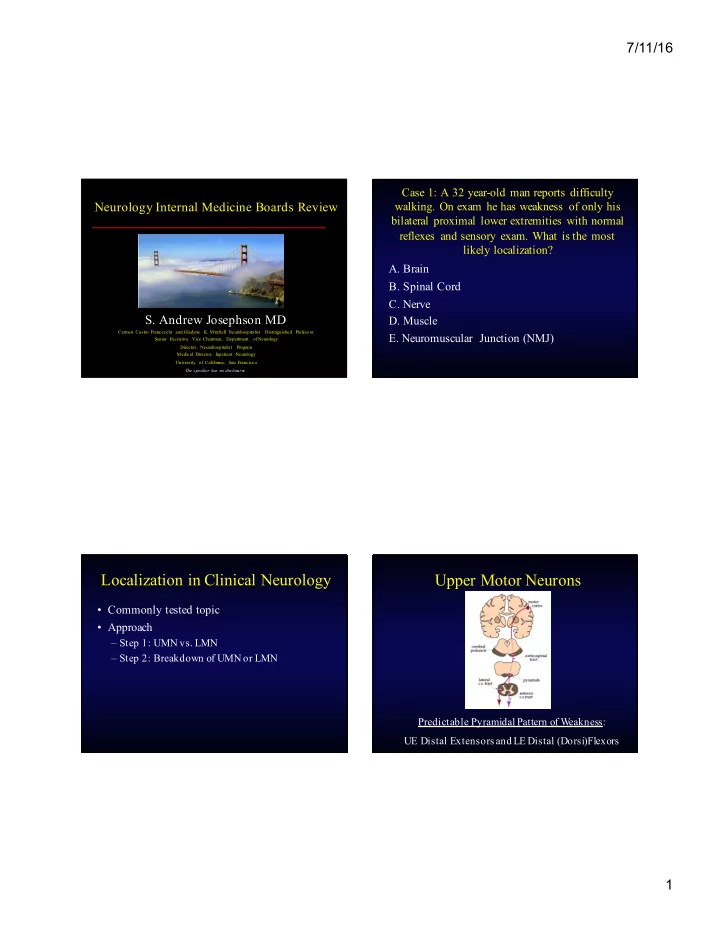
7/11/16 Case 1: A 32 year-old man reports difficulty Neurology Internal Medicine Boards Review walking. On exam he has weakness of only his bilateral proximal lower extremities with normal reflexes and sensory exam. What is the most likely localization? A. Brain B. Spinal Cord C. Nerve S. Andrew Josephson MD D. Muscle Carmen Castro Franceschi and Gladyne K. Mitchell Neurohospitalist Distinguished Professor E. Neuromuscular Junction (NMJ) Senior Executive Vice Chairman, Department of Neurology Director, Neurohospitalist Program Medical Director, Inpatient Neurology University of California, San Francisco The speaker has no disclosure s Localization in Clinical Neurology Upper Motor Neurons • Commonly tested topic • Approach – Step 1: UMN vs. LMN – Step 2: Breakdown of UMN or LMN Predictable Pyramidal Pattern of W eakness: UE Distal Extensors and LE Distal (Dorsi)Flexors 1
7/11/16 Step 1: UMN vs. LMN Step 2: UMN Breakdown UMN LMN • Either: Pattern of weakness – 1. Brain (including brainstem) Pyramidal Variable – 2. Spinal cord Slow alternating Function/Dexterity Variable movements • Pearls Increased Tone Decreased – A sensory level on the trunk = spinal cord Decreased, absent Tendon Reflexes Increased – Bladder dysfunction = spinal cord or normal – “Crossed signs” = brainstem Babinski sign, Atrophy (except for Other signs other CNS signs NMJ disorders) – Facial weakness = brain (above the pons) Step 2: LMN Breakdown Step 2: LMN Breakdown Pearls • Either: • Sensory Symptoms or Signs = Nerve – 1. Anterior Horn Cell (AHC) • Reflexes Decreased = Nerve (or AHC) – 2. Nerve • Proximal Weakness = Muscle or NMJ – 3. Neuromuscular Junction (NMJ) – Fatigue or fluctuating weakness = NMJ – 4. Muscle • Fasciculations = AHC (or Nerve) • Combination of UMN and LMN signs = ALS 2
7/11/16 What treatment should you initiate? Case 2 • A 65 year-old man with a history of DM, HTN A. IV t-PA presents with 9 hours of L sided binocular B. Heparin visual loss C. Aspirin 325 mg • Examination shows left-sided homonymous D. Plavix (clopidogrel) hemianopia and is otherwise unremarkable. E. Aggrenox (ER dipyridamole + ASA) • The patient is on ASA 81mg daily Intravenous t-PA Intravenous t-PA • Important contraindications to remember • Time of onset=last time seen normal – INR greater than 1.7 • Pivotal IV t-PA NINDS trial (0-3 hours***) – Platelets less than 100 – 30% increase in minimal or no disability at 90 days – Seizure at onset, low glucose – Symptomatic hemorrhage risk increased 0.6 to 6.4% – Recent surgery or hemorrhage • Ischemic stroke with significant disability – BP>185/100 sustained despite treatment • No bleed on non-contrast head CT 3
7/11/16 Shrinking Indications for Antiplatelet Options Anticoagulation in Stroke 1. Atrial Fibrillation • 1. ASA – 50mg to 1.5g equal efficacy long-term 2. Some other cardioembolic sources • 2. Aggrenox – Thrombus seen in heart – ?EF<35 – 25mg ASA/200mg ER Dipyridamole • ESPS-2, ESPRIT (Lancet 5/06) – ?PFO with associated Atrial Septal Aneurysm • 3. Clopidogrel (Plavix) 3. Vertebral and carotid artery dissection • MATCH (Lancet 7/04), FASTER (Lan Neurol 11/07) 4. Rare hypercoagulable states: APLA • PRoFESS trial results announced 5/08 Aggrenox vs. Plavix Antiplatelet Options • Aggrenox • If on no antiplatelet medication – Headache in first 2 weeks: 30% discontinue – ASA or Plavix or Aggrenox – Perhaps not compatible with cardiac antiplatelet • If already on ASA goals or with unstable angina – Switch to Aggrenox or Plavix – Cannot be crushed in FT • Plavix – Concerns regarding use with ASA 4
7/11/16 Differential for Transient Focal When to Fix the Carotid? Neurologic Deficit • NASCET in early 1990s • The Big Three – Benefit of endarterectomy in patients with – 1. TIA symptoms ipsilateral to 70-99% stenosis – 2. Seizure • Comparison: best medical management at the time – 3. Complicated Migraine • In stroke management don’t miss carotid disease or atrial fibrillation Case 3 Case 3 • A 67F is hospitalized with a community-acquired • You are called to the bedside and after 3 minutes, pneumonia. On Day#3 she is feeling much better these movements have not stopped. Options for awaiting discharge when her nurse finds her your next course of action are…. unresponsive with rhythmic shaking of all limbs. A. Continue to wait for the spell to subside • PMHx: COPD B. Administer IV Diazepam • Meds: Ceftriaxone, NKDA C. Administer IV Lorazepam • SH: 100pk yr hx tobacco, no hx EtOH D. Administer IV Fosphenytoin • FH: No neurologic disease E. Administer IV Phenytoin 5
7/11/16 Status Epilepticus Case 3 • Changing definition and time window in 2010 • Incidence: 100,000 to 150,000 per year nationally • Following Lorazepam 2mg IV x 3 (2 • Contributes to 55,000 deaths per year nationally minutes apart), the patient is still having • 12 to 30 percent of epilepsy first presents as status these movements (now 7 minutes). What is • Generalized convulsive status most dangerous your next course of action? Lowenstein DH, et al: N Engl J Med 338:970, 1998 Previous Algorithm Status Epilepticus Algorithm: Real World 1. Lorazepam 2mg IV q2 minutes up to 6mg 2. Fosphenytoin 18-20mg/kg (Dilantin Equivalents) IV 2a. Fosphenytoin additional 10mg/kg or Phenobarbital 3. General Anesthesia with continuous EEG a. IV Midazolam gtt b. IV Propofol gtt Lowenstein DH, et al: N Engl J Med 338:970, 1998 6
7/11/16 Monotherapy for Seizures New Drugs: Clinical Pearls • 70 percent of epilepsy can be managed with • IV formulations: VPA, DPH, PHB, LVT monotherapy, most on first drug tried • Levels to Monitor: VPA, DPH, PHB, CBZ • Concept of Maximal Tolerated Dose (MTD) • Lamotrigine (Lamictal) • Rarely check levels – Rash (1/1000) progressing to Stevens-Johnson – Assess compliance • Levetiracetam (Keppra) – Steady state level – Not practically available with newer AEDs – No drug interactions (useful on HAART) • Topiramate (Topamax) – Well tolerated?: weight loss and cognitive side effects N Engl J Med. 2000 Feb 3;342(5):314-9 New Drugs: Clinical Pearls Case 4 • Oxcarbazepine (Trileptal) • A 45 yo man presents with 2 days of progressive tingling and weakness of the – Tegretol pro-drug lower extremities. He now is having trouble – Hyponatremia walking and rising from a chair. • Felbamate (Felbatol) – Aplastic Anemia with required registry • Gabapentin (Neurontin) – Not a great AED 7
7/11/16 What test should you next order? Case 4 A. MRI Brain • Exam B. MRI Thoracic Spine – MS, CN normal C. MRI Lumbar/Sacral Spine – Motor: normal tone throughout, normal power D. Lumbar Puncture in upper ext., 4/5 throughout in the lower extremities E. Blood Cultures – Sensory: decreased PP/Vib/temp patchy in lower extremities, Sensory level to PP at T4 – Reflexes: 1 and symmetric throughout, toes neutral Workup of Myelopathy Case 5 • First step: MRI with contrast – Pick appropriate level A 44 man presents with bilateral numbness of the – Excludes structural disease legs, urinary incontinence and spinal fluid with an • Second Step: If MRI negative, usually elevated white blood cell count consisting of mainly proceed to lumbar puncture lymphocytes. Upon his death, a pathological – Pleocytosis = autoimmune or infectious specimen of his spinal cord is shown. What is the transverse myelitis etiology of his symptoms? – No Pleocytosis = metabolic, vascular, genetic 8
7/11/16 Case 6: 56F with bilateral numbness and Case 7: A 66M presents with tremor. Which of weakness of the legs with macrocytic anemia the following findings makes the diagnosis of Parkinson’s Disease more likely that Essential Tremor? A. Speed: 4-6 Hz B. Tremor is primarily postural C. Tremor relieved with alcohol D. Symmetric Tremor E. +FH of a similar tremor Parkinson’s Treatment ET PD 3 1. Give L-Dopa Speed 5-10Hz 4-6 Hz 1 - Levodopa/Carbidopa 2 Symmetry Symmetric Asymmetric 2. Dopamine Receptor Agonists Most Common -Pramipexole, Ropinirole Postural Rest Component 3. Alter Dopamine/L-Dopa Metabolism No Y es Helped by EtOH -MAO-B Inhibitors: selegeline, rasagiline Common -COMT Inhibitors: entacapone Rare FH? Autosomal Dominant 4. Decrease Cholinergic tone (rarely used) 5. Surgery: Deep Brain Stimulation (DBS) Any sign of Parkinsonism in an ET pt should lead to questioning the diagnosis 9
7/11/16 Parkinson’s Treatment Obscure, but often asked ABIM fact: Pearls Name the disease below www.healthandage.com • Only treat when function is impaired • Start with L-dopa or a dopamine agonist – Agonists are best in those age <70 as they have cognitive side effects (hallucinations) in the elderly • If L-dopa is “wearing off”, increase the frequency or add COMT inhibitor • Reduce the dose if peak-dose dyskinesias are impairing function Case 8: A 54M comes to the ED with the worst Wilson’s Disease headache of his life. Which of the following findings would be most worrisome for SAH? • Consider in any young patient with a movement disorder A. Extremely severe head pain – Especially with LFT abnormalities – Especially with psychiatric findings B. Photophobia • Diagnosis with low serum ceruloplasmin C. Pain reaching maximum intensity in seconds • Usually treat with chelators such as D. Vomiting penicillamine, trientine E. No relief with high doses of opioids 10
Recommend
More recommend