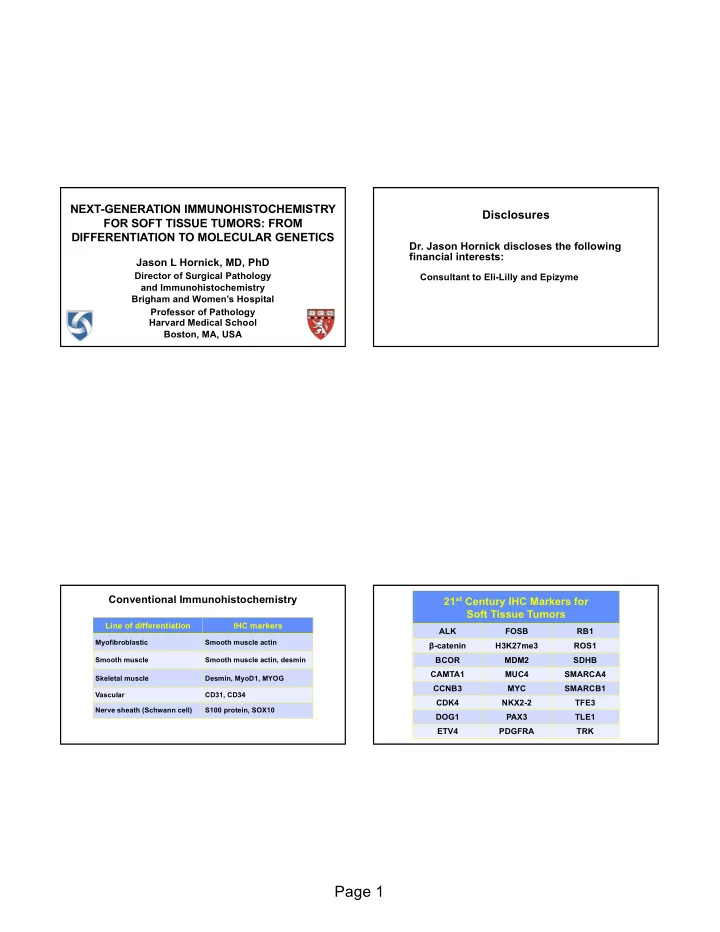
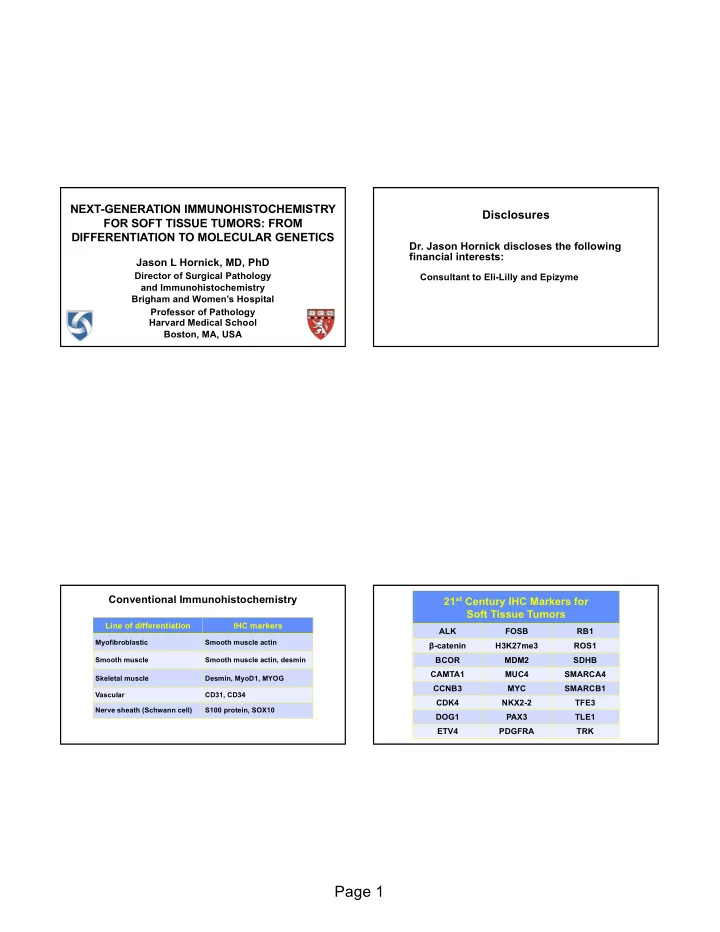
NEXT-GENERATION IMMUNOHISTOCHEMISTRY Disclosures FOR SOFT TISSUE TUMORS: FROM DIFFERENTIATION TO MOLECULAR GENETICS Dr. Jason Hornick discloses the following financial interests: Jason L Hornick, MD, PhD Director of Surgical Pathology Consultant to Eli-Lilly and Epizyme and Immunohistochemistry Brigham and Women’s Hospital Professor of Pathology Harvard Medical School Boston, MA, USA 21 st Century IHC Markers for Conventional Immunohistochemistry Soft Tissue Tumors Line of differentiation IHC markers ALK FOSB RB1 Myofibroblastic Smooth muscle actin β-catenin H3K27me3 ROS1 Smooth muscle Smooth muscle actin, desmin BCOR MDM2 SDHB CAMTA1 MUC4 SMARCA4 Skeletal muscle Desmin, MyoD1, MYOG CCNB3 MYC SMARCB1 Vascular CD31, CD34 CDK4 NKX2-2 TFE3 Nerve sheath (Schwann cell) S100 protein, SOX10 DOG1 PAX3 TLE1 ETV4 PDGFRA TRK Page 1
Malignant Peripheral Nerve Sheath Tumor Protein Correlates of Molecular Genetic • Arise in patients with NF1, sporadically, or following Alterations in Soft Tissue Tumors radiation therapy β-catenin PDGFRA • Challenging diagnosis • Diagnostic criteria: CDK4 RB1 1. Origin from a nerve or a neurofibroma H3K27me3 SDHB 2. Spindle cell sarcoma in a patient with NF1 3. Evidence of Schwann cell differentiation by IHC or EM MDM2 SMARCA4 (BRG1) » S100 protein and SOX10 only 30-50% sensitivity • Diagnosis in sporadic setting relies on distinctive MYC SMARCB1 (INI1) histology and exclusion of mimics Polycomb Repressive Complex Oct 2014 Nov 2014 Epigenetic modification of chromatin: • PRC2 recruits to chromatin and trimethylates histone H3 at lysine 27 Physiologic regulation of cell fate and proper stem cell differentiation Deregulation à cancer development Nov 2014 Modified from Sauvageau et al. Cell Stem Cell 2010 Page 2
Immunohistochemistry for H3K27me3 in PRC2 and MPNST Malignant Peripheral Nerve Sheath Tumors • PRC2 alterations ( SUZ12 or EED mutations) in 85-90% Tumor type H3K27me3 loss of MPNST MPNST, low grade 35% • Homozygous mutations result in loss of H3K27me3 (histone H3 lysine 27 trimethylation) in ~65% of MPNST MPNST, intermediate grade 60% MPNST, high grade 80% • Rate of H3K27me3 loss depends on grade • IHC for H3K27me3 highly specific diagnostic marker Epithelioid MPNST 0% Schaefer et al. Mod Pathol 2016 Schaefer et al. Mod Pathol 2016 Prieto-Granada et al. Am J Surg Pathol 2016 Prieto-Granada et al. Am J Surg Pathol 2016 Immunohistochemistry for H3K27me3 in Other Malignant Peripheral Nerve Sheath Tumor Spindle Cell Neoplasms Tumor type H3K27me3 loss Cellular schwannoma 0% Atypical neurofibroma 0% Monophasic synovial sarcoma 0% Leiomyosarcoma 0% Myxofibrosarcoma 0% Malignant solitary fibrous tumor 0% Low-grade fibromyxoid sarcoma 0% Spindle cell rhabdomyosarcoma 0% Gastrointestinal stromal tumor 0% Fibrosarcomatous DFSP 0% Spindle cell melanoma 7% Dedifferentiated liposarcoma 6% H3K27me3 Page 3
Malignant Peripheral Nerve Sheath Tumor Cellular Schwannoma H3K27me3 H3K27me3 Monophasic Synovial Sarcoma Spindle Cell Melanoma H3K27me3 H3K27me3 Page 4
Solitary Fibrous Tumor Protein Products of Gene Fusions • Anatomically ubiquitous fibroblastic neoplasm (pleura, retroperitoneum, abdomen, head & neck) ALK PAX7 • “Patternless” architecture, varying cellularity, BCOR ROS1 prominent stromal collagen, dilated branching (“staghorn”) vessels CAMTA1 STAT6 • “Hemangiopericytoma” synonymous with SFT CCNB3 TFE3 (uniform hypercellularity) FOSB TRK • CD34 positive in 95% of cases, but not specific (many other tumor types positive) PAX3 WT1 Solitary Fibrous Tumor Solitary Fibrous Tumor Page 5
Hemangiopericytoma = Solitary Fibrous Tumor Cellular Solitary Fibrous Tumor Malignant Solitary Fibrous Tumor Solitary Fibrous Tumor CD34 Page 6
5% of SFTs are CD34 negative CD34-positive soft tissue tumors Tumor type Solitary fibrous tumor Dermatofibrosarcoma protuberans Spindle cell/pleomorphic lipoma Kaposi sarcoma Angiosarcoma (70%) Neurofibroma (subset of cells) Soft tissue perineurioma (65%) CD34 Solitary Fibrous Tumor and STAT6 • NAB2-STAT6 consistent fusion gene • Both genes on chromosome 12q13 in close proximity (overlapping) • Conventional FISH cannot be used • Nuclear STAT6 expression highly specific for SFT Page 7
Solitary Fibrous Tumor STAT6 Doyle et al. Mod Pathol 2014 Malignant Solitary Fibrous Tumor Monophasic Synovial Sarcoma STAT6 Page 8
Monophasic Synovial Sarcoma Epithelioid Hemangioendothelioma • Distinctive sarcoma showing endothelial differentiation; less aggressive than angiosarcoma • Epithelioid cells arranged in cords and nests • Myxohyaline stroma typical • Occasional cytoplasmic vacuoles • Keratin expression common • May be confused with metastatic carcinoma, especially lobular breast and signet-ring-cell gastric STAT6 Epithelioid Hemangioendothelioma Epithelioid Hemangioendothelioma Page 9
Epithelioid Hemangioendothelioma CD31 Immunohistochemistry for CAMTA1 • Nuclear staining in most cases of EHE • Negative in epithelioid hemangioma and epithelioid angiosarcoma • Negative in nearly all carcinomas • Negative in other epithelioid mesenchymal tumors • Useful diagnostic marker for EHE Shibuya et al. Histopathology 2015 Doyle et al. Am J Surg Pathol 2016 Page 10
Epithelioid Hemangioendothelioma CAMTA1 Doyle et al. Am J Surg Pathol 2016 Epithelioid Hemangioendothelioma Epithelioid Hemangioma liver CAMTA1 CAMTA1 Page 11
Epithelioid Angiosarcoma Epithelioid Hemangioma • Subset (head and neck) also known as angiolymphoid hyperplasia with eosinophilia • Head and neck (especially peri-auricular), bone, penis • Small subcutaneous nodule +/- tender or pruritic • 20% multiple lesions • Up to 1/3 recur locally • Cellular examples with poor canalization may be misdiagnosed as malignant (but minimal nuclear atypia) CAMTA1 Epithelioid Hemangioma Epithelioid Hemangioma Page 12
Epithelioid Hemangioma Cellular Epithelioid Hemangioma Cellular Epithelioid Hemangioma SMA Page 13
Epithelioid Hemangioma Cellular Epithelioid Hemangioma FOSB FOSB Epithelioid Hemangioendothelioma Pseudomyogenic Hemangioendothelioma • Distinctive rarely metastasizing endothelial neoplasm • Often presents with multiple discontiguous nodules in different tissue planes of a limb • Histologically mimics a myoid tumor or epithelioid sarcoma FOSB Page 14
Pseudomyogenic Hemangioendothelioma Pseudomyogenic Hemangioendothelioma • Striking male predominance (5:1) • Young adults (peak in 2 nd and 3 rd decades) • Most patients (75%) present with cutaneous nodules • 50% intramuscular; 20% intraosseous lesions • 50% local recurrences or develop additional nodules in same anatomic area • Despite ominous clinical presentation, distant metastasis rare Pseudomyogenic Hemangioendothelioma Pseudomyogenic Hemangioendothelioma Page 15
Pseudomyogenic Hemangioendothelioma Pseudomyogenic Hemangioendothelioma Pseudomyogenic Hemangioendothelioma Pseudomyogenic hemangioendothelioma: Immunohistochemistry Positive Negative Keratins AE1/AE3 Keratins MNF116 ERG EMA FLI1 CD34 CD31 (variable) S100 protein INI1 (retained) Desmin Page 16
Pseudomyogenic Hemangioendothelioma AE1/AE3 ERG Page 17
Pseudomyogenic hemangioendothelioma FOSB FOSB Hung et al. Am J Surg Pathol 2017 Biphenotypic Sinonasal Sarcoma Biphenotypic Sinonasal Sarcoma • Distinctive low-grade sarcoma unique to sinonasal tract • Adults, wide age range • Female predominance • Most common in nasal cavity and ethmoid sinus • Recurrence in 40% • Thus far, no metastases or tumor-related deaths Page 18
Biphenotypic Sinonasal Sarcoma Biphenotypic Sinonasal Sarcoma Biphenotypic Sinonasal Sarcoma Biphenotypic Sinonasal Sarcoma SMA S100 Page 19
75% 5% 20% Biphenotypic Sinonasal Sarcoma PAX3 Page 20
Biphenotypic Sinonasal Sarcoma Diagnostic Markers Identified by Gene Expression Profiling DOG1 (ANO1) NKX2-2 ETV4 SATB2 MUC4 TLE1 PAX3 NKX2-2 NKX2-2 • Homeobox transcription factor involved in neuronal • IHC: diffuse nuclear NKX2-2 sensitive marker for Ewing development and glial/ neuroendocrine differentiation sarcoma (90-95%) • Also positive in Ewing sarcoma with EWSR1-ERG and • Gene expression profiling: NKX2-2 downstream target “atypical” Ewing sarcoma of EWSR1-FLI1 fusion • Imperfect specificity: mesenchymal chondrosarcomas • NKX2-2 required for oncogenic transformation often positive (also olfactory neuroblastomas) Page 21
Ewing Sarcoma EWSR1-FLI1 NKX2-2 Hung et al. Mod Pathol 2016 Ewing Sarcoma CIC-DUX4 Sarcoma EWSR1-ERG NKX2-2 NKX2-2 Page 22
Mesenchymal Chondrosarcoma CIC -rearranged Sarcoma • Most common “Ewing-like” (“undifferentiated”) round cell sarcoma that lacks EWSR1 gene fusions (at least 70%) • Majority with CIC-DUX4 fusions • Wide age range; peak in young adults • Deep soft tissue of extremities and trunk most frequent • Bone and visceral sites rare • Much more aggressive clinical course and worse survival than Ewing sarcoma; currently treated similarly NKX2-2 Page 23
Recommend
More recommend