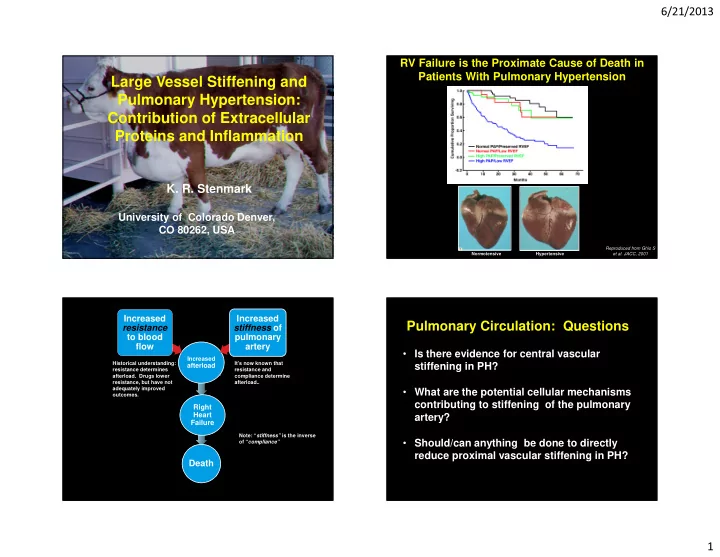
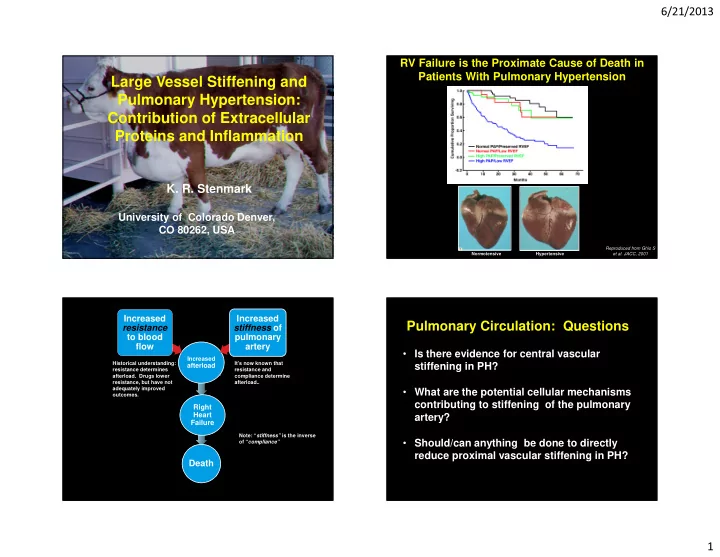
6/21/2013 RV Failure is the Proximate Cause of Death in Patients With Pulmonary Hypertension Large Vessel Stiffening and Pulmonary Hypertension: Contribution of Extracellular Proteins and Inflammation K. R. Stenmark University of Colorado Denver, CO 80262, USA Reproduced from Ghio S et al. JACC, 2001 Normotensive Hypertensive Increased Increased Pulmonary Circulation: Questions resistance stiffness of to blood pulmonary flow artery • Is there evidence for central vascular Increased Historical understanding: It’s now known that afterload stiffening in PH? resistance determines resistance and PAH afterload. Drugs lower compliance determine resistance, but have not afterload.. adequately improved • What are the potential cellular mechanisms outcomes. contributing to stiffening of the pulmonary Right Heart artery? Failure Note: “ stiffness” is the inverse • Should/can anything be done to directly of “ compliance” reduce proximal vascular stiffening in PH? Death 1
6/21/2013 Significant Increases in Impedance are Pulmonary Hypertensive Vessels Observed in Patients with PAH Enlarge and Stiffen. Hypertensive PA Normotensive PA D= 1.6 cm D= 2.5 cm Artery Wall At Systole Wall Deformation Over Cardiac Cycle Measured by MRI (Age, Gender and BSA Matched) • Significant elevation in modulus of impedance for the first three harmonics in patients with PH. • Z 0 : resistance, Z 1 , Z 2 : oscillatory function / capacitance Hunter et al., Am H.J., 2008 PAH-Associated Vascular Physiologic Stiffness is Increased in Remodeling in Human Patients with PAH Circumferential Stress Normal PA Hypertensive PA Collagen PA Stiffening in Severe PH HEALTHY HYPERTENSIVE HEALTHY HYPERTENSIVE Elastin fragmentation Collagen accumulation 2-Photon Second Harmonic Generation Microscopy: Elastin ; Collagen 2
6/21/2013 Chronic Hypoxia Results in Stiffening of the Extralobar Pulmonary Arteries in Mice and Rats Mouse Can Animal Models be Used to Study Proximal Vascular Stiffening in Pulmonary Ex Vivo biaxial stress strain testing of rat PAs Hypertension? Rat Interim Summary: Marked Increases in Resistance and Stiffening PH-Associated Pulmonary Vascular in Chronically Hypoxic Neonatal Calves Remodeling in Human � Significantly elevated stiffness � Early collagen engagement Indices of Pulmonary Vascular Indices of Ventricular Resistance Stiffening � Significant anisotropy (different Neonatal (2 wk-old) longitudinal vs. circumferential Peak Systolic Mean PAP Total Pulmonary Pulse Calves MPA Stiffness mechanics) Matrix Remodeling in PH Pressure (mm Hg) Resistance Pressure FUNCTIONAL (mm KPa) (mm Hg) (mm Hg/L/min) (mm Hg) � Loss of elastin-dependent Control (n=12) 31.0 ± 3 20.1 ± 3 2.1 ± 1.0 20.1 ± 2 112 ± 35 mechanics STRUCTURAL: Moderate PH (n=6) 59.4 ± 7.5 42.3 ± 7.8 5.6 ± 1.4 32.3 ± 7.3 163 ± 51 • Elastin fragmentation � Near total loss of PA capacitive Severe PH (n=8) 101.5 ± 17.7 73.4 ± 10 8.0 ± 2.0 51.2 ± 16.9 287 ± 101 • Collagen accumulation function 3
6/21/2013 Hypothesis: Large Vessel Stiffening is Due to Accumulation and Pulmonary Circulation: Questions Activation of Mononuclear Cells • Is there evidence for central vascular stiffening in pulmonary hypertension? • What are the potential cellular mechanisms contributing to stiffening of the pulmonary artery? • Should/can anything be done to directly reduce proximal vascular stiffening in PH? Elevated mPAP, pulse pressure, and disturbed flow patterns → High Afterload → Right Heart Failure. Humans with PAH: Calf Model Exhibits Greater Similarities Accumulation of Monocyte/Macrophage in to Human PAH than Rodent Models Pulmonary Artery Media, Neointima, and Adventitia Calf Rat Influx of inflammatory cells in PA Adventitia only. Accumulation of inflammatory cells in PA Media, Adventitia, (and Neointima); Elastin • PA media normally contains “resident” immunomodulatory leukocytic cells; fragmentation is observed Medial “resident” immunomodulatory • in PAH, numbers of these cells within cells vascular media markedly increase. 4
6/21/2013 Vascular Inflammation, Elastin Fragmentation, and Vascular Stiffening Extracellular Matrix (ECM) Derived Fragments Can Drive a Vascular Inflammatory Response Activated Macrophages Degradation of Elastin ECM peptides with immune / inflammatory effects: • Elastin Elastin Fragments • Collagen (I and IV) (“Elastokines”) • Fibronectin • Laminin • Thrombospondin Chemotactic Pro- Pro-Mitogenic Anti- • Hyaluron for leukocytes Angiogenic for VSMCs & Fibs Apoptotic Chronic Inflammation Rabinovitch M. 1999; Antonicelli F. et al. 2007 Vascular Remodeling Duca L. et al 2004 Expression of Pro-Inflammatory Mediators, Pro-Fibrotic Bone Marrow-Derived Macrophages (BMDMs) Markers, and Proteolytic Enzymes is Augmented in Vascular – but not SMCs – Media of Hypoxic Hypertensive Calves (Hx) Respond to Elastin Peptide Treatment by Upregulating RT-PCR Pro-Inflammmatory Mediators Ccl12 Ssp1 Il1b Il6 Ccl2 (Osteopontin) (SDF-1) (MCP-1) RT-PCR 500 1200 Expression relative to HPRT Ν os2 (iNOS) 8 210 Il1 β Ccl2 (MCP-1) 375 900 11 168 5 6 9 * * * * ** 250 2 126 600 Relative Expression to HPRT 6 4 * 9 84 4 300 125 2 6 42 2 3 0 0 0 0 0 CO Hx C H CO Hx C H CO Hx O x O x * Col3a1 Thbs-1 Mmp1 Col1a1 ? ? (Thrombospondin-1) (MMP-1) (Collagen I) (Collagen III) 160000 275 600 * 0 120000 125 220 100 400 165 0 80000 75 110 50 200 40000 0 55 25 0 0 0 0 C H Hx CO Hx CO Hx CO O x 5
6/21/2013 Bone Marrow-Derived Macrophages (BMDMs) – but not SMCs – Interim Summary: Responded to Elastin Peptide Treatment by Upregulating Pro-Fibrotic Markers • Normal conduit PA media (human and bovine, Ccl12 (SDF-1) Ssp1 (Osteopontin) Tnc (Tenascin-C) but not rodent) contains “resident” Relative Expression to HPRT * * * * ** inflammatory/immunomodulatory leukocytic cells. • In pulmonary hypertension, increased accumulation of numbers of these leukocytic Thbs1 (Thrombospondin- Col1a1 (Collagen I) Col3a1 (Collagen III) 1) cells is observed. Relative Expression to HPRT ** * * * * • Elastin peptides induce activation of naïve macrophages (BMDMs): upregulated mRNA expression of pro-inflammatory and pro-fibrotic markers. Pulmonary Circulation: Questions Compliance is Fundamental to PH � Low compliance is the leading independent predictor of • Is there evidence for central vascular mortality stiffening in pulmonary hypertension? � Compliance correlates directly with exercise capacity and quality of life • What are the potential cellular � Low compliance accounts for up to 50% of RV afterload � Low compliance stimulates progression of the disease mechanisms contributing to stiffening of � Pulmonary vascular stiffness is increased 25- to 30-fold the pulmonary artery? � etc… • Should/can anything be done to directly reduce proximal vascular stiffening in 1 Campo et al, Am J Respir Crit Care Med , 2009, 2 Mahapatra et al , J Am Soc. Echocardiography , 2006, 3 Mahapatra et al, J Am Col Card , 2006, 4 Gan et al, Chest , 2007, 5 Hunter et al , J Appl Physiol , 2010, 6 Sanz et al, JACC Card. Imag . 2009, 7 Li and Chesler, Pulm. Circ . 2011, 8 Perrot et al, Chest, 2011, 9 Bonderman et al, Chest, 2011, 10 Saouti et al, Am J Respir Crit Care Med , 2010, 11 Milnor et al, Circ Res , 1966, PH? 12 Milnor et al, Circ Res , 1969, 13 Wang and Chesler, Pulm Circ , 2011, 14 Stenmark et al, Circ Res , 2006, 15 Birukov Andiox Redox Sig , 2009 , 16 Li et al, Ann Biomed Eng , 2009 , 17 Stevens et al, JACC, Cardiovascular Imaging, 2012 6
6/21/2013 Potential Mechanisms of HPF-Induced Therapies Aimed at Reducing Perpetuation of Distal PA Remodeling In PH Vascular Stiffening • Renin Angiotensin Aldosterone System (RAAS) blockers • AGE – cross-link breakers (alagebrium) • Statins • Anti-Inflammatory agents • Elafin (serine protease inhibitor) SM Ce SMC hypertrophy SM Ce Fibs--Myofibs differentiation Fibroblst-myod Aria CV’s Device Restores Compliance to PA Bench: Hemodynamic Benefits Pressure in Pulmonary Artery Reservoir 140 120 Pa Pressure (mmHg) 100 SQ access 80 port Off 60 On Conduit 40 Gas filled balloon Systole Diastole & anchor 20 0 0 0.2 0.4 0.6 0.8 Time (s) • Implanted like a pacemaker Device Hemodynamic Effects Expected Patient Effects KV1 • Mimics function of elastic pulmonary artery • Balloon collapses during systole & expands • Increase in exercise Compliance Lower systolic pressure during diastole increased by 0.51 capacity & QOL • reduces RV work & wall stress ml/mmHg (in this • Acts like a passive IABP • increases SV • Decrease in example) mortality likely Higher diastolic pressure • By restoring compliance, it allows more • Increases blood flow blood to flow for less heart work Reduction of pulse pressure • breaks the disease-stimulating feedback loop 7
Slide 27 KV1 Do we want to say that it functions similar to an IABP? Stick in slide with benchtop data in it. Karl Vollmers, 6/17/2013
Recommend
More recommend