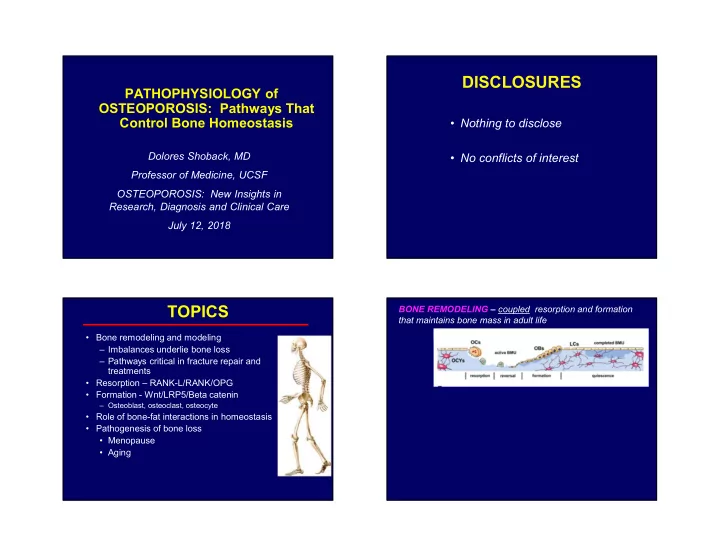
DISCLOSURES PATHOPHYSIOLOGY of OSTEOPOROSIS: Pathways That Control Bone Homeostasis • Nothing to disclose Dolores Shoback, MD • No conflicts of interest Professor of Medicine, UCSF OSTEOPOROSIS: New Insights in Research, Diagnosis and Clinical Care July 12, 2018 TOPICS BONE REMODELING – coupled resorption and formation that maintains bone mass in adult life • Bone remodeling and modeling – Imbalances underlie bone loss – Pathways critical in fracture repair and treatments • Resorption – RANK-L/RANK/OPG • Formation - Wnt/LRP5/Beta catenin – Osteoblast, osteoclast, osteocyte • Role of bone-fat interactions in homeostasis • Pathogenesis of bone loss • Menopause • Aging
BONE REMODELING – coupled resorption and formation Agents that suppress REMODELING – fill in that maintains bone mass in adult life resorption spaces BONE MODELING – process that shapes bones as we grow & develop (childhood, adolescence); also occurs at low rates - Early in menopause, when baseline remodeling throughout life; resorption and formation are uncoupled and rates are high large BMD increases occur they occur on different surfaces; net bone growth - Senile osteoporosis, steroids, disease states – low remodeling rates minimal BMD increases Baron and Hesse, JCEM, 2012 Why Do Bones Remodel? Allows skeleton to -- Agents that stimulate MODELING – grow new bone wherever – considerable potential to rebuild skeletal Respond to mechanical loading (modeling) mass (senile osteoporosis, low bone formation states, Repair microdamage (“wear and tear”) & prevent fracture non-unions, etc) accumulation • Maintains “quality control” Baron and Hesse, JCEM, 2012
Microfracture Is Repaired through Microfracture Is Repaired through Targeted Remodeling Targeted Remodeling Glucocorticoids Apoptosis of OB’s & osteocytes Bisphosp, denosumab Inhibit or deplete Segovia-Silvestre T et al, Hum Genet, 2009 Segovia-Silvestre T et al, Hum Genet, 2009 Why Do Bones Remodel? Allows skeleton to -- RANK-Ligand/ • Respond to mechanical loading (modeling) • Repair microdamage (“wear and tear”) & prevent RANK/Osteoprotegrin accumulation • Maintains “quality control” Pathway Release minerals (Ca and phosphate) & growth factors stored in matrix into circulation (& microenvironment) • Important in skeletal homeostasis Remodeling imbalances – important in aging and post-menopause
Osteoclastogenesis: Hormones, Growth Osteoprotegerin (OPG) Prevents RANK- Factors, Cytokines Stimulate Expression of L/RANK Interaction & Inhibits OC Activity RANK-L {RANK+RANK-L Interact} [OPG=Circulating Inhibitor, product of OB cells ] CFU-M RANKL CFU-M Pre-fusion RANKL PTH Glucocorticoids Pre-fusion Osteoclast Osteoclast PGE 2 RANK RANK Vitamin D OPG Multinucleated X Osteoclast IL-11 Denosumab +mCSF does the Multinucleated IL-6 Osteoclast same thing IL-1 Hormones Growth PTHrP X Factors TNF- Cytokines Activated Activated Osteoclast Osteoclast Osteoblasts Bone Formation Osteoblasts & BM Stromal Cells Bone X Boyle WJ et al. Nature 2003;423:337; Hofbauer LC, Boyle WJ et al. Nature 2003;423:337 Bone Resorption Resorption Schoppet M. JAMA 2004;292:490 . Wnt/ b -Catenin - arrest disrupt Role in Bone Formation differentiation cytoskeleton Antiresorptive drugs act on osteoclasts with different mechanisms of action - Bisphos - OC’s stay on bone surface (drug – internalized, long half-life) - Denosumab – resorbing OC’s never form (MAb not internalized – short half-life) Baron R et al, Bone, 2011
Wnt Signaling Pathway - 1 OSTEOBLAST LINEAGE CELLS (Duan and Bonewald, Int J Biochem Cell Biol , 2016) Mesenchymal stem cells, pre-OB’s, mature OB’s, bone- • Wnt/ b -catenin pathway regulates cell fate throughout lining cells, stromal cells, and osteocytes lifespan • Canonical Wnt pathway – depends on Wnt/ b -catenin • Produce matrix and mineralize it – signaling – Mechanical support – Matrix - reservoir of Ca, phosphate, growth factors, • Non-canonical Wnt pathways – independent of b - hormones catenin (Ca 2+ , other signaling pathways) – Secrete endocrine & paracrine factors – FGF23, DMP1, etc • Many receptors, inhibitors, activators, modulators, • Modulate development of tri-lineages of blood cells phosphatases, kinases, enzymes in Wnt pathway – • Play role in metabolism , male reproduction complex regulation b -catenin – central molecule Function and numbers of cells in OB lineage decline • Key receptors – LRP4, 5, 6 with aging – many factors responsible * Wnt Signaling Pathway - 3 Wnt Signaling Pathway - 2 (Duan and Bonewald, Int J Biochem Cell Biol , 2016) (Duan and Bonewald, Int J Biochem Cell Biol , 2016) • In bone and cartilage, Wnt important in: • Studies in osteocytes Wnt pathway important in sensing mechanical stimuli and responding to – Skeletal development, limb patterning, chondrogenesis them – OB differentiation/function/matrix synthesis – Differentiation and functioning of OC’s • Targeted deletion of b -catenin in osteocytes in • Targeted deletion of b -catenin in OB’s in mice mice – Reduced differentiation of MSC OB and OB survival – Progressive loss of bone mass with growth ( low BMD) – Decreased [OPG], increased resorption – Increased osteoclast activity – due to less OPG – Low bone mass phenotype • Other pathways interact (cross-talk) with Wnt • Targeted deletion of b -catenin in OC’s in mice signaling – estrogen, PTH, prostaglandin, BMP-2 (anabolic) – Less clear-cut – Increased resorption
If no Wnt present, no signaling - β- Canonical Wnt Signaling catenin levels are LOW • Wnt signaling (OB, OB precursors) recruits IC protein Axin which moves to tail of LRP5/6 (because of interaction with Dvl ) • Complex forms, recruits FRAT1 and glycogen synthase kinase-3 β • Complex forms & inhibits β- NEW bone catenin phosphorylation • Non-phos β-catenin formation accumulates in cytosol, goes to (quiescent & nucleus remodeling • β-catenin binds to LEF/TCF surfaces) FINAL elements and activates OB + OPG transcription program ( osteoprotegerin) • RSPO & norrin modulate Wnt Lewiecki et al, Nat Rev Rheumatol, 2011 Baron R, Kneissel M, Nat Med 2013 Sclerostin Made by Osteocytes Negatively Wnt Inhibition Regulates Bone Formation • WIF1 (Wnt inhibitory factor) or SFRP (secreted frizzled related protein) Sclerostin* sequester Wnt ligand Mesenchymal • Axin & APC associate stem cells Mature Pre-osteoblast with GSK-3 β increase Osteoblasts lining cells X X phosphorylation of β- catenin New bone • β-catenin~P ubiquinated proteasome for degradation Bone • NO bone made Osteocyte • Other inhibitors: N- cadherin inhibits • Preclinical studies targeting gene (KO) and Ott SM. JCEM 2005; Semenov M, et al. LRP5/Wnt; sclerostin & transgenic overexpression of protein support JBC 2005; Semenov MV, et al. JBC DKK1 2006; Li X, et al. JBC 2005 these roles for Sclerostin Baron R, Kneissel M, Nat Med 2013
Clinical Studies: Sclerostin As Bone- Specific Molecular Target • Sclerosteiosis – rare recessive genetic disorder of high bone mass (bony overgrowth CNS compression, death) Interaction of Bone and Fat: – Heterozygous family members [1 functional sclerostin (Sost) allele] – healthy, have higher Physiologic and Disease than normal BMD (high Z, high T scores - no other complications) and normal life expectancy States – Reduced level sclerostin (lifetime) tolerated • Multiple clinical trials - Mab blocking sclerostin (romosozumab) dose-dependently increases BMD and reduces fractures Bone Marrow Fat (Devlin M, Rosen CJ, Lancet Diab Endo, 2015) Plasticity – • Bone and fat – juxtaposed in marrow cavities pre-OB and • Dynamic fat depot pre- • Adipocytes release cytokines & adipokines adipocytes • Metabolic processes, hematopoiesis, osteogenesis Bone lining • Osteoblasts and adipocytes come from the cells Communication OB’s & same precursor mesenchymal stem cell osteocytes • Bone and fat function as a ‘niche’ normally & Devlin and Rosen, Lancet Diab, Endo 2015 adipocytes if • BMAT - plays role in modulating • Niche/microenvironment injury osteoporosis, aging, obesity, diabetes • Precursors final cells – classical view; likely to be ‘plasticity’ of cells along the way, phenotypic change
Recommend
More recommend