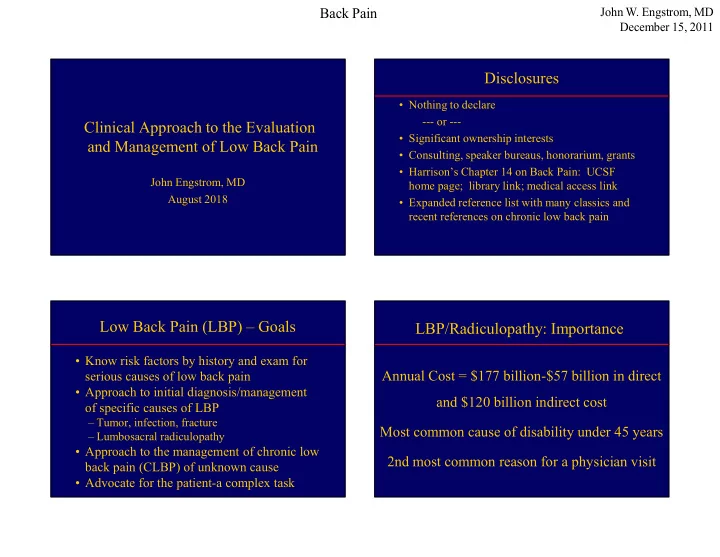
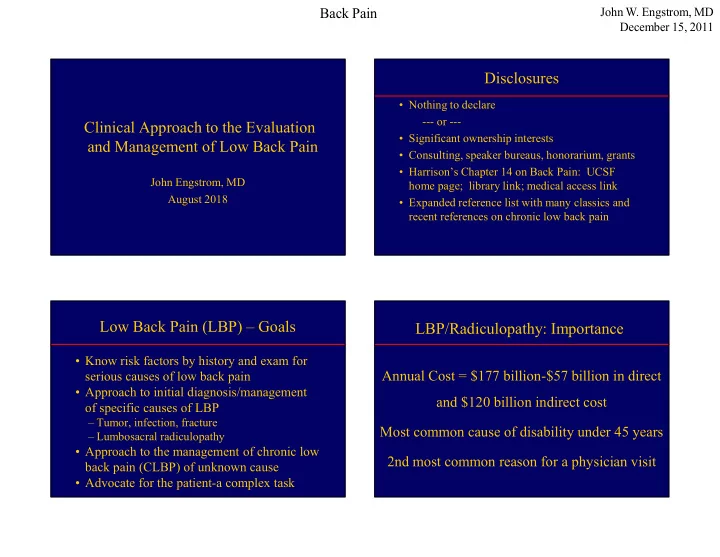
Back Pain John W. Engstrom, MD December 15, 2011 Disclosures • Nothing to declare --- or --- Clinical Approach to the Evaluation • Significant ownership interests and Management of Low Back Pain • Consulting, speaker bureaus, honorarium, grants • Harrison’s Chapter 14 on Back Pain: UCSF John Engstrom, MD home page; library link; medical access link August 2018 • Expanded reference list with many classics and recent references on chronic low back pain Low Back Pain (LBP) – Goals LBP/Radiculopathy: Importance • Know risk factors by history and exam for Annual Cost = $177 billion-$57 billion in direct serious causes of low back pain • Approach to initial diagnosis/management and $120 billion indirect cost of specific causes of LBP – Tumor, infection, fracture Most common cause of disability under 45 years – Lumbosacral radiculopathy • Approach to the management of chronic low 2nd most common reason for a physician visit back pain (CLBP) of unknown cause • Advocate for the patient-a complex task 1
Back Pain John W. Engstrom, MD December 15, 2011 Acute LBP: Risk Factors for Serious Acute LBP: Risk Factors for Serious Cause - History Cause - Examination Prior history of cancer Unexplained, documented fever Pain at rest or at night-most common risk missed Unexplained, documented weight loss History of chronic infection Palpation tenderness over spinous processes-C/T/L History of trauma Abdominal, rectal, or pelvic mass Intravenous drug use Patrick’s sign or heel percussion sign Corticosteroid use Straight-leg or reverse straight-leg raising signs History of rapidly progressive neurologic deficit Rapidly progressive focal neurologic deficit Age > 70 years ALBP-Natural History/Treatment LBP – General Examination • 85-90% back to functional baseline in 12 weeks Abdomen-pulsatile mass in 50-75% with AAA • Treat symptoms Spine-palpate spinous processes; use – NSAIDs or acetaminophen for pain paraspinal muscles as a control for non- – Limited bed rest-2 days max; progressive ambulation specific pain – Muscle relaxants if back pain interferes with sleep Hips-Internal/external rotation with leg flexed – Muscle relaxants often not tolerable during a work day Pelvis and Rectum-rare, but don’t forget – Opioids are not a first choice! – Reassurance 2
Back Pain John W. Engstrom, MD December 15, 2011 Initial Approach to Acute Back or Examination Signs Neck Pain Signs that reproduce usual pain symptoms Patrick’s Sign - Hip or buttock pain elicited by Acute LBP 1 internal rotation of the hip with flexion of the leg at the knee Risks for Serious Source? Straight-leg raising – Traction on L5 or S1 roots or sciatic nerve (all posterior to hip) Yes No Reverse straight-leg raising – Traction on L2- Consider infection, tumor, fracture Symptomatic Rx x 3 months No Diagnostic Tests L4 roots or femoral nerve (all ant to hip) 1 Pain < 3 months duration Lumbosacral Radiculopathy - Algorithm 2 -ALBP Suspected Serious Etiology Neurologic Findings Risk factors present Root Motor Reflex Sensory Pain Distribution L4 Quads (knee ext) Knee Medial calf Medial calf Fracture Cancer Infection Rapidly progressive Leg adduct neurologic deficit L5 EHL/EDB/Peronei None Lateral calf, Posterolateral thigh; ESR, CBC, consider consultation, (foot eversion) dorsal foot Lat calf, dorsal foot Plain X-ray/CT Immediate consultation imaging, other lab S1 FDL (toe flexors) Ankle Sole foot Posterior thigh/calf Sole foot 3
Back Pain John W. Engstrom, MD December 15, 2011 Exam for L/S Radiculopathy-Motor L/S Radiculopathy-Sensory • Use smallest bulk muscle avail-most sensitive • Decreased sensation (negative sensory symptoms) • L4 - If quad weak, check leg adductors (obturator nerve) indicates a decrease in sensory function; • L5 -Dorsiflex toes (EDB)/great toe (EHL) • Paresthesias/pain (positive sensory symptoms) -Evert foot (peronei); dorsiflex foot-TA reflect alive nerve cells firing inappropriately • S1 -Toe Flexors-tibial nerve, sciatic nerve • Elicit either a decrease in quantity or quality of • Overcome flexion of toes with fingers-do not screen with sensation (decrease = loss of sensory axons) big toe or foot plantar flexion • Compare light touch from side-to-side • Sensation scale (0 to 10; 0=None, 10 = normal) L/S Radiculopathy-Reflexes L/S Radiculopathy-Sensory • Symmetry of the reflex is more important than • L4 -Medial calf absolute value (3+ throughout vs. right 3/left 2) • L5 -Lateral calf or dorsal foot • Limbs in analagous positions to compare sides • S1- Sole foot • If you can’t get a reflex, add stretch to the tendon or reinforcement • Sens loss from root/nerve injury occurs in a patch • L4-sitting or supine, knees bent if supine • Circumferential loss below the knees suggests spinal cord/brain lesion or polyneuropathy • L5-No associated reliable reflex • S1-strike Achilles or ball of dorsiflexed foot 4
Back Pain John W. Engstrom, MD December 15, 2011 Lumbar Radiculopathy-Anatomic Diagnosis • Paracentral disk herniation (root in lateral recess) or lateral disk herniation (root in neural foramen) • Bony foraminal stenosis • Tumor, infection, fracture • Scarring from prior injury • Anatomy helps determine etiology of a lumbar radiculopathy and consideration for surgery Natural History of Acute Acute Disk Herniation and Nerve Root Injury: Disk-Related Radiculopathy Compression or Inflammation? Usually Not Compression • Weber (1983)- If deficit and pain tolerable while waiting, - Mobile nerve roots spontaneous recovery common - Nerve roots move during lumbar puncture • Saal (1989)-Focal motor deficits improve with rehab; - Gelatinous nucleus pulposus does not compress pain improves over time-not as fast as with surgery - Favorable response to steroids • Bottom Line: If patient can function with the pain, then the long term outcome is about the same with and Evidence for Inflammation: Extrusion of nucleus without surgery pulposis inflammation demyelination 5
Back Pain John W. Engstrom, MD December 15, 2011 Pros of Spine Imaging Radiculopathy is not a Radiologic Diagnosis • May find specific and treatable cause for symptoms • MR Imaging did not replace the neurologist; • Outstanding anatomic definition instead, the imaging findings doubled our work • Non-invasive • “Is the anatomic change clinically significant?” • MRI preferred for anatomy of soft tissues • Imaging establishes anatomic plausibility • CT is helpful for detection of fractures • Disk abutment to nerve roots often asymptomatic • CT myelography can define the extent to which • Does the history, exam, and ancillary testing (as abnormalities seen on MRI are bony (e.g.- measures of nerve root function) support the foraminal narrowing from bone vs disk) helpful anatomic abnormality Role of Exam and EMG studies Cons of Spine Imaging • Neurologic exam is a qualitative measure of how the nervous system functions (physiology) • Expensive in the U.S. • MRI assesses anatomy of the nervous system – $143 for spine MRI in Taiwan in 2010! – Radiology a profit center vs. a cost center • EMG gives a semi-quantitative measure of nerve • Non-specific findings that do not explain the tissue function (physiology) patient’s symptoms are very common • When the anatomy and physiology point to the – May lead to unnecessary additional testing same cause, the probability of a correct diagnosis – May alarm patients and clinicians unnecessarily increases dramatically – Set patient expectations when testing ordered 6
Back Pain John W. Engstrom, MD December 15, 2011 Disk Herniation: Surgical Radiculopathy Diagnostic Stool and Indications the 4 legs: Hx, Exam, Radiol, EMG • History suggests a nerve root injury -Cauda equina syndrome (CES) • Exam shows focal abnormalities suggesting nerve root injury -Spinal cord compression (C/T-spine) • Radiology (MRI) shows anatomic nerve root -Progressive motor weakness by exam injury or compression • EMG, when necessary, establishes nerve root Severe Radicular Pain - Controversial injury and excludes peripheral nerve injury CES Symptoms and Signs CES Diagnosis and Management • Patient describes perineal or perianal numbness • Common etiologies-Herniated disk, tumor, abscess, traumatic displacement of spine, • New nocturia or bowel/bladder incontinence • Almost never due to chronic spondylotic spinal stenosis • Unable to feel or reduced feeling for toilet paper after urination or bowel movement • Consensus opinion-earlier surgery (within 1-2 days) better than later-partial syndrome better than complete • Weakness and numbness in the legs in the distribution of multiple bilateral nerve roots • Send to ER for lumbar spine MRI or CT • Acute, subacute, chronic • Request emergent spine surgery consultation 7
Recommend
More recommend