Cathra Halabi, MD February 14, 2020 Patient Presentation A 42-year-old man with a history of migraine experienced severe headache, anxiety, and difficulty concentrating. Two months ago, he was involved in a mid-air collision with another athlete during a recreational basketball game. There was no blunt head impact. He felt stunned for several moments, then required assistance while walking to the sideline due to imbalance. He did not play for the rest of the game and was driven home. Over the next 1-2 days, he developed a throbbing headache with nausea and photosensitivity. He presented to his local urgent care clinic and was advised to rest until symptom remission. Despite excessive sleep, he felt fatigued with cognitive fog. He abstained from basketball and any other physical exertion due to symptom exacerbation. He took 1 week off of work as his company’s executive though he worked from home, then returned to a typical schedule. Usual activities in the office exacerbated the headaches, requiring frequent breaks and longer days. He could not focus or multitask though his colleagues did not note significant change. He felt uncharacteristically irritable and emotionally labile which further intensified his distress. He was delivering a routine presentation for his company board, as he had done on a quarterly basis for 10 years, when he suffered a first anxiety attack. He was advised by his board to take additional time off. He again presented to his local urgent care clinic. Subsequent brain MRI without gadolinium was normal. He was referred to a neurologist for persistent headaches. His general examination was normal. On neurological examination, he was embarrassed by tearfulness and subjectively felt unsteady with Romberg and tandem gait maneuvers. In addition, exam maneuvers requiring eye movements prompted discomfort and nausea. He asked if he would ever be able to return to work. He asked if he was developing dementia. A diagnosis was provided and a plan was implemented. References 1. Blennow K et al. Nat Rev Dis Primers. 2:16084, 2016. 2. Giza CC et al. Neurology. 80:2250, 2013. 3. Brody DL. Oxford Press, 2019. 4. Gardner RC, Yaffe K. Mol Cell Neurosci. 66:80, 2015.
Cathra Halabi, MD February 14, 2020 Case Discussion The patient likely sustained a concussion during the mid-air collision with his fellow teammate. In addition to blunt head trauma (such as from falls or other community accidents), whiplash, body-checking, and blast injuries from a variety of mechanisms can generate forces that are transmissible to and through the brain, disrupting neurological function. Signs and symptoms may be apparent immediately or may emerge over 1-2 days. A proportion of patients will experience prolonged recovery beyond commonly quoted timeframes of 1 week to 3 months. The terms concussion and mild traumatic brain injury (mTBI) are often used interchangeably but concussion is considered to be the mildest form of mTBI. Concussion/mTBI may cause a range of debilitating symptoms and functional impairment. The term “persistent post-concussive symptoms” is preferred over “post-concussion syndrome” as the latter may actually reflect alternative diagnoses including exacerbated premorbid medical conditions (such as migraine) and may also include maladaptive perspectives toward recovery. Concussion/mTBI is currently a purely clinical diagnosis. Heterogeneity in clinical manifestations reflect complex pathophysiologic mechanisms and patient-level features including age at time of injury and comorbid conditions or vulnerabilities. In concussion specifically, current clinical neuroimaging modalities yield normal results. Concussion/mTBI is a treatable condition. A systematic, domain-based approach assists the clinician in maintaining organized diagnostic and therapeutic strategies. Individual diagnoses within domains should be considered where possible for targeted treatment (e.g., post-traumatic migraine, exacerbated or de novo anxiety, insomnia). Judicious use of diagnostic tools should be tailored to the patient. Tools include neuroimaging, neuropsychological testing, and serum neuroendocrine studies in appropriate cases. An active recovery approach is favored over prolonged rest. Active recovery approaches include escalating exposures to usual activities and escalating “doses” of subthreshold or threshold aerobic exercise. These strategies should be implemented with guidance from interdisciplinary colleagues such as physical or occupational therapists, since symptom provocation may prevent an individual patient from adhering to treatment plans. Concussion/mTBI has increasingly been linked to elevated risk for developing neurodegenerative disease. There are numerous patient-level factors that affect this risk. Many individuals with neurodegenerative conditions have never sustained a concussion/mTBI, and many individuals with history of concussion/mTBI do not develop neurodegenerative disease. However, it is important to recognize refractory or
progressive neurobehavioral symptoms despite optimal management strategies for prompt referral to the appropriate specialist(s). References 1. Blennow K, Brody DL, Kochanek PM, et al: Traumatic brain injuries. Nat Rev Dis Primers. 2:16084, 2016. 2. Harmon KG, Clugston JR, Dec K, et al: American Medical Society for Sports Medicine Position Statement on Concussion in Sport. Clin J Sport Med. 29:87, 2019. 3. Giza CC, Kutcher JS, Ashwal S, et al: Summary of evidence-based guideline update: Evaluation and management of concussion in sports: Report of the guideline development subcommittee of the American Academy of Neurology. Neurology. 80:2250, 2013. 4. Guideline for Concussion/Mild Traumatic Brain Injury & Persistent Symptoms. Third Edition, 2018. https://braininjuryguidelines.org/concussion/fileadmin/media/adult-concussion- guidelines-3rd-edition.pdf 5. Scholten J, Vasterling JJ, Grimes JB. Traumatic brain injury clinical practice guidelines and best practices from the VA state of the art conference. Brain Injury. 31: 1246, 2017. 6. Gardner RC, Yaffe K. Epidemiology of mild traumatic brain injury and neurodegenerative disease. Mol Cell Neurosci. 66:80, 2015.
2/14/2020 Financial Disclosures • None Challenging Case Cathra Halabi, MD Assistant Clinical Professor of Neurology Founder & Director, Neurorecovery Clinic Neurovascular Division, Department of Neurology Weill Institute for Neurosciences 1 2 Case Presentation: Chief Complaint Case Presentation: HPI Day 0: • The patient sustained a mid-air collision with another athlete during recreational basketball game. No blunt head impact. A 42-year-old man with a history of • He felt stunned for several moments, then required assistance while walking to the sideline due to imbalance . migraine experienced severe headache, anxiety, and difficulty concentrating. Day 0-2: • The patient developed headache , nausea, photosensitivity . • He presented to his local urgent care clinic and was advised to rest until symptom remission. 3 4 1
2/14/2020 Case Presentation: HPI, continued Case Presentation: HPI, continued Day 0-7: Day 35: • The patient had excessive sleep, fatigue, cognitive fog . • He again presented to local clinic. Imaging was ordered. • There was symptom exacerbation with physical, cognitive, or emotional exertion. Day 39: • Subsequent brain MRI without gadolinium was normal. Day 0-14: • He was referred to a neurologist for persistent headaches. • He could not focus or multitask. He felt uncharacteristically irritable and emotionally labile. Day 56: First neurology evaluation. • He had a first ever panic attack during routine, longstanding activities. 5 6 Case Presentation: Additional History Case Presentation : Review of Systems Allergies: None. Review of Systems: Medications : None. Past Medical History: Migraine. It’s complicated. Social History: Executive, avid recreational athlete, no tobacco products, rare Stay tuned. alcohol use, no recreational drug use. Family History: • Migraine (mother) • Possible undiagnosed anxiety disorder (brother) • Unspecified learning disability (brother) 7 8 2
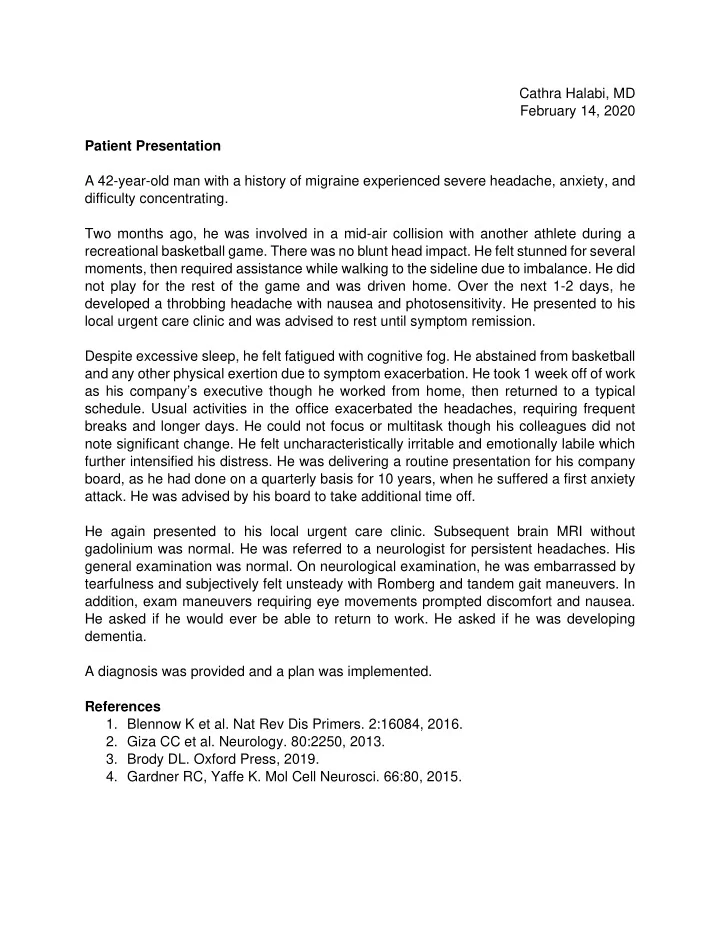
2/14/2020 Case Presentation: Examination What is the diagnosis? 53% • Vital Signs: Normal. A. Concussion 38% B. Post-concussive syndrome • General Examination: Normal. C. Persistent post-concussive symptoms D. Anxiety 7% • Neurological Examination: Technically normal. 2% – MS: Tearful. Concussion Anxiety Post-concussive syndrome Persistent post-concussiv... – CN: Nausea with eye movements. – SENS: The patient sustained a concussion during the mid-air Discomfort and unsteadiness with Romberg. – GAIT: Discomfort and unsteadiness with tandem gait. collision due to transferred force despite absence of head impact. He is experiencing persistent post- concussive symptoms (C) , of which anxiety is one. 9 10 Definitions: Concussion/mTBI Definitions: Concussion/mTBI Ontario AAN Sports Brain Trauma Neurotrauma VA/DoD CPG CDC/ACEP Concussion ACRM Foundation Foundation Guidelines mTBI involves disruption of brain function due to some external non- penetrating force that is transmitted to the brain. Ontario AAN Sports Brain Trauma Neurotrauma VA/DoD CPG CDC/ACEP Concussion ACRM Foundation +/- LOC, but if present the duration must be <30 min. Foundation Guidelines 2018 2016 2016/2008 2014 2013 1993 (GCS 13-15) Peri-trauma amnesia must be <24 hours. There may be AMS and/or physical symptoms immediately after the index event, sometimes with emergence of impairments within 1-2 days. 13 14 3
Recommend
More recommend