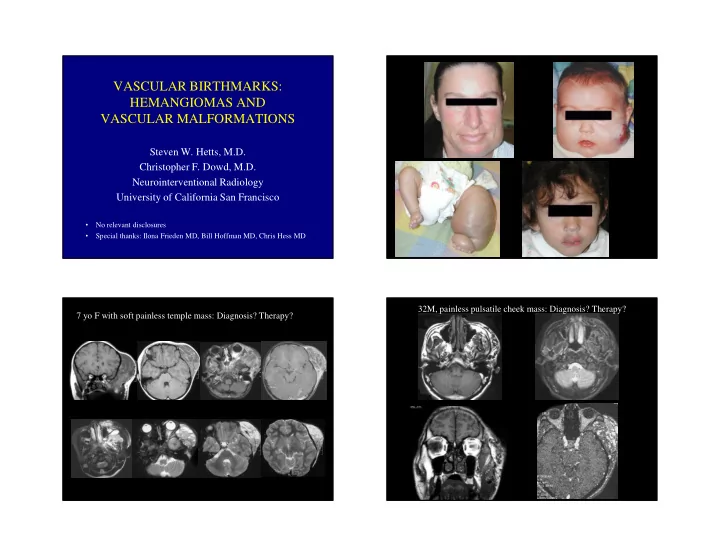
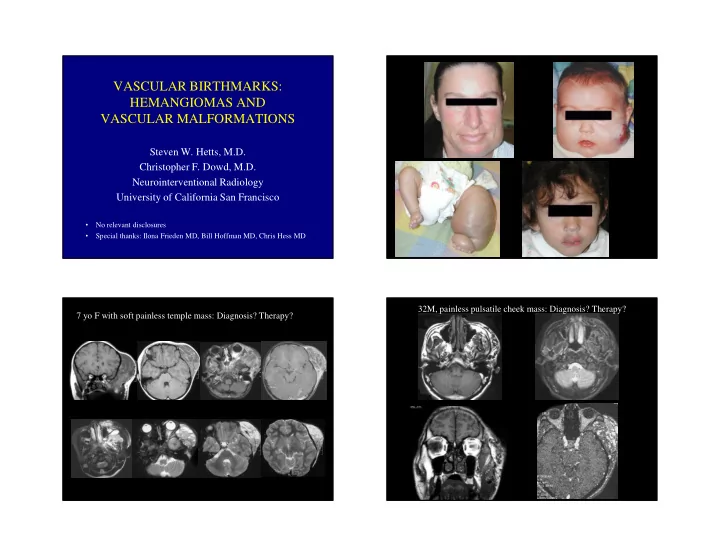
VASCULAR BIRTHMARKS: HEMANGIOMAS AND VASCULAR MALFORMATIONS Steven W. Hetts, M.D. Christopher F. Dowd, M.D. Neurointerventional Radiology University of California San Francisco • No relevant disclosures • Special thanks: Ilona Frieden MD, Bill Hoffman MD, Chris Hess MD 32M, painless pulsatile cheek mass: Diagnosis? Therapy? 7 yo F with soft painless temple mass: Diagnosis? Therapy? 1
Common Misconceptions (Dowd) Vascular Birthmark: What is it? • All vascular birthmarks are not “ hemangiomas ” ! Confusing Terminology • All vascular malformations are not “ AVMs ” ! • Strawberry hemangioma • Cavernous hemangioma • 50% of patients referred to the UCSF Vascular • AVM Anomalies Clinic carry an incorrect diagnosis! • Cystic hygroma • Angioma • Port wine stain • Naevus flammeus • Eponymous syndromes Vascular Birthmark: Classification * Vascular Birthmark: Classification Clinical and Cellular Differences Vascular Tumor Vascular Malformation Hemangioma (Infantile) Vascular Malformation • Infantile Hemangioma • Arterial (AVM) • Tumor of blood vessels • Malformed blood vessels • Tumors producing KMP • Venous • Not present at term birth • Present at birth “low flow” – KHE - Kaposiform • Lymphatic • Proliferation/involution • Commensurate growth Hemangioendothelioma • Capillary – Tufted Angioma • F/M: 3/1 • F/M: 1/1 • (Combination) • Congenital Hemangioma • ↑ endothelial turnover • nl endothelial turnover – RICH • ↑ FGF • nl FGF – NICH • GLUT 1 staining • No GLUT 1 staining (*Mulliken and Glowacki, 1982) 2
Hemangioma (Infantile) Diagnosis of Vascular Birthmark • Benign tumor of blood vessel origin • Endothelial cell proliferation ( ↑ bFGF) • More important: • GLUT1: immunohistochemical stain – age of patient • Most common tumor of infancy (~10%) – physical examination • F/M : 3/1 – history (esp. birth/childhood/recent activity) • Share phenotype markers of placenta • Less important: • Clinical: classically appear at age ~2 wks – imaging – Proliferative phase: rapid growth to age 10-12 mo. – Involuting phase: slower involution -> fibrofatty scar • Common mimic: venous malformation -> Go look at patient and ask a few questions! • Focal (70%) vs. Segmental 3m 6d 6w Infantile Hemangioma: Imaging • well-circumscribed • T1: intermediate signal • T2: high signal • “ salt and pepper ” pattern of • enhancement: homogeneous 6m-steroids 19m vessels within tumor • [angio: vascular tumor blush, normal size feeding arteries, no A-V shunt] 3
3moM, infantile hemangioma Hemangioma: Therapy • No therapy: preferred because hemangiomas involute! • Medical therapy – Propranolol (2008) – steroids (systemic or intralesional) • Surgery – early, when vital structures compromised – late, to treat residual fibrofatty scar • Embolization: – Not necessary preoperatively – [Often used to Rx Kasabach-Merritt Syndrome] 2moM, KHE, KMP, platelets=5000 Rx: platelets, α INF, prednisone,Vincristine, embolization (repeated) Kasabach-Merritt Syndrome • Severe thrombocytopenia (platelet trapping) • Formerly thought to arise in aggressive variant of Infantile Hemangiomas • Now known to arise in: – Kaposiform Hemangioendothelioma (KHE) • Clinical: “ angry ” red-purple vascular tumor – Tufted Angioma post-embo • Imaging: appear similar to infantile hemangioma with less discrete borders pre-embo • Rx: embo, prednisone, Sirolimus, VCR, surg, ( α INF) mid-embo 4
Congenital Hemangiomas RICH vs NICH vs IH: Clinical Behavior RICH: Rapidly-Involuting Congenital Hemangioma (limb, near joint, “soufflé”) NICH: Non-Involuting Congenital Hemangioma (flat, pallid, “red-white-blue”) • Fully grown in utero • Present at birth • F/M : 1/1 • No GLUT1 staining from Nozaki et al, Radiographics 33:175-195, 2013 RICH, newborn NICH, 7 yo F Vascular Birthmark: Classification * Vascular Tumor Vascular Malformation • Infantile Hemangioma • Arterial (AVM) • Tumors producing KMP • Venous at birth “low flow” – KHE - Kaposiform • Lymphatic Hemangioendothelioma • Capillary – Tufted Angioma • (Combination) • Congenital Hemangioma – RICH – NICH (*Mulliken and Glowacki, 1982) 3mo p/ excision 5
Arteriovenous Malformation (AVM) AVM: Imaging • flow voids • Vascular malformation characterized by a nidus of vessels • May have “soft tissue” lacking the normal capillary bed, causing high-flow element (Type I vs II) arteriovenous shunting. • best-seen on gradient echo • F/M : 1/1 • involved ST may be swollen • Growth commensurate; also may be triggered by trauma, • may involve bone surgery, hormonal effects (puberty, pregnancy). ?Role of • partition images helpful angiogenesis factors? • MRA not helpful [Dowd] • Clinical: pulsatile mass with thrill/bruit; pain, swelling, • angio: A-V shunt with bleeding (may be life-threatening); high-output CHF nidus, enlarged feeding • Difficult to eradicate fully arteries and draining veins 32M, facial AVM AVM: Therapy • No therapy • Embolization (agent, route) – palliative – preoperative – curative • Surgery (you ’ d better get it all!) 6
29F, popliteal AVM Rx: ETOH embolization 24M, “neurofibromatosis”, increasing arm pain, “please biopsy” Pre-embo Embo Embo Post-embo 7
51F, CHF, huge left thorax/shoulder AVM L int. mam. pre- LV L T5 costocerv. tr. L int. mam. post- L T10 intercostal->spinal art.! LW Venous Malformation Venous Malformation: Pathology • Vascular malformation characterized by dilated veins, limited • Large serpiginous channels mural smooth muscle (allows gradual expansion) • Outdated name: “ cavernous hemangioma ” • Single-layer endothelial • Non-proliferating: no endothelial turnover, no ↑ bFGF lining • Very little smooth muscle • F/M : 1/1 • Clinical: dilated venous channels, usu. boggy/compressible, no thrill, enlarge w/ gravity-dependence or Valsalva, firmer w/ thrombosis • Spongiform (“cave-like”) vs. Phlebectatic (“tubular”) phenotypes • Commensurate growth • Large/IM VMs -> low-grade consumptive coagulopathy (“LIC”) Mulliken and Young 1988 8
Venous Malformation: Imaging Venous Malformation: Therapy • discrete/scattered soft tx lsn. • T1: intermediate signal • T2: high signal • No therapy • enhancement: homogeneous • ASA • no flow voids • uni/multilocular • Compressive stocking • can involve muscle/bone • Laser • + phleboliths (CT, plain) • angio: normal art. phase, • Sclerotherapy may have venous puddling • Surgery • direct px: irregular venous pouches 39F, venous malformation, sclerotherapy Sclerosing Agents: venous malformation • Sotradecol (sodium tetradecyl sulfate 3%) • Ethanol (~pure) • Bleomycin • Sodium morrhuate • Ethanolamine oleate Mix with contrast for visualization U/S and fluoro guidance Avitene slurry to close puncture site(s) 9
pre-scleroRx immed. post Rx post-scleroRx (3wk) Capillary Malformation • Vascular malformation characterized by ectatic vessels within the upper dermis • Aka: “ port-wine stain ” , “ naevus flammeus ” • Non-proliferating: no endothelial turnover, no ↑ bFGF • Trigeminal (V1) lesions assoc. w/ Sturge-Weber Syndrome • F/M : 1/1 • Clinical: sharply-demarcated flat pink-red stain; grows proportionately; no involution; hue deepens with crying, warmth, fever; color darkens w/age (pink->red->purple); texture more nodular w/age. • Usually no imaging in isolated cases DB Capillary Malformation Capillary Malformation: Therapy Thin-walled capillaries in upper dermis (Mulliken and Young 1988) • No treatment • Laser therapy to remove color (temporary) 10
Lymphatic Malformation: Imaging Lymphatic Malformation • macro- vs. micro-cystic • multiple cysts • Vascular malformation characterized by malformed • T1: low (water) signal, lymphatic cavities lined by flattened endothelium • Aka: “ cystic hygroma ” , “ lymphangioma ” unless prior hemorrhage, Rx • Non-proliferating: no endothelial turnover, no ↑ bFGF • T2: high (water) signal • fluid-fluid layers typical • F/M : 1/1 • enhancement: rim only • Microcysic vs. Macrocystic • Clinical: Neck/face/axilla common; diverse morphology • angio: normal (enlarged limb, nodular vesicles, translucent cysts) • direct px: well-defined • Commensurate growth cysts, +/- intercommunicate • Enlargement with infection (bacterial/viral), hemorrhage 7 yo F with macrocystic lymphatic malformation 6wkM, combined macro- and microcystic lymphatic malformation upper leg (macro- and micro-) lower leg (micro-) 11
Recommend
More recommend