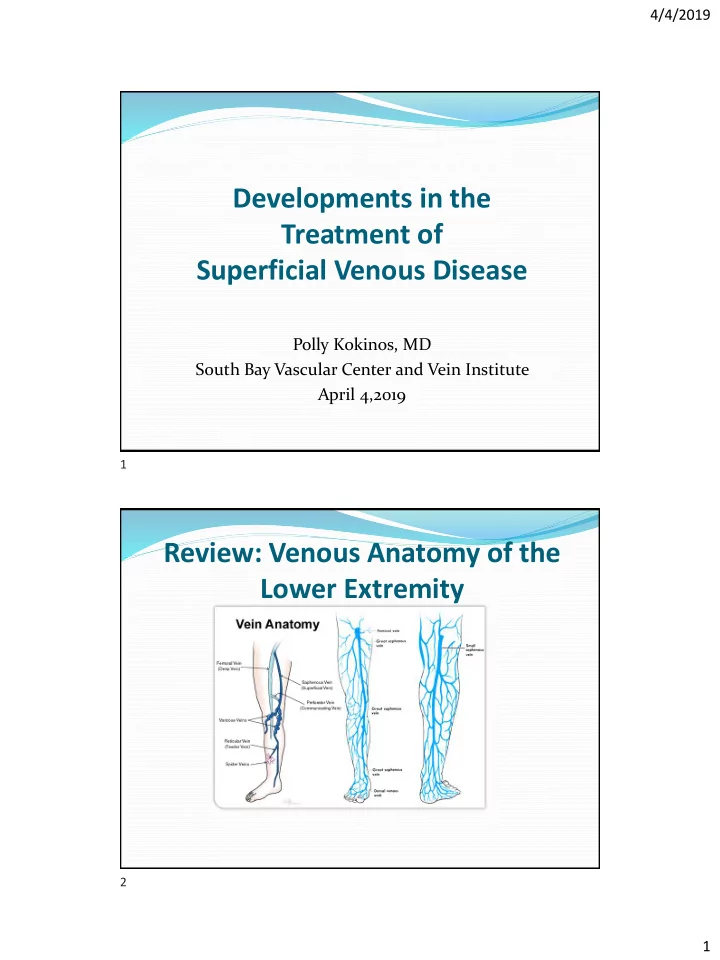
4/4/2019 Developments in the Treatment of Superficial Venous Disease Polly Kokinos, MD South Bay Vascular Center and Vein Institute April 4,2019 1 Review: Venous Anatomy of the Lower Extremity 2 1
4/4/2019 Manifestations and Mechanisms of Venous Insufficiency 3 Treatment Patterns and Outcomes in Patients with Varicose Veins Retrospective review of claims in 2008-2010 of database with 45 million claims Eligibility: Age over 18, One diagnosis came during time with “varicose veins”(ICD9 454) Had health coverage for at least one year before and two years after the time period above Eligible to be included in study: 150K claims Results: 90.8% Female, Mean age 53 years Treatment used: 100K managed conservatively (70%) 23 K had thermal endovenous treatment 4800 had sclerotherapy 4800 had surgery 11K had multiple modalities During the 2 year follow-up, 54% of patients treated with interventional treatment had another treatment for varicose veins, however this did not adjust for laterality (1/3 patients had bilateral disease), or for “staged” treatment of GSV/SSV, varicosities, or perforators. Most of the additional treatments occurred within the first 60 days. Am Health Drug Benefits. 2016 Nov; 9(8): 455 – 465 4 2
4/4/2019 Superficial Venous Insufficiency: Treatments COMPRESSION THERAPY IS THE CORNERSTONE OF THERAPY High ligation and stripping: rarely done today Thermal Method: Endovenous ablation using radiofrequency/laser: FDA approved since 2005 Non-thermal methods: MOCA( mechanico-chemical ablation): Clarivein Sclerotherapy: Varithena Glueing of vein: VenaSeal 5 EVRA Trial: Does treating Superficial Venous Insufficiency help ulcer healing? 450 patients in the UK Randomized to early ablation vs. Compression +/- delayed ablation Outcomes: time to healing healing percentage at 24 weeks recurrence rate ulcer-free interval QoL Gohel MS, et al, NEJM 2018; 378:2105-2114 6 3
4/4/2019 EVRA Trial Results: Median time to healing: 56 days vs. 82 days (p=0.001) 24-week healing 85.6% vs 76.3% Ulcer recurrence 11.4% vs 16.5% Ulcer-free interval 306 days vs 278 days (p=0.002) Gohel MS, et al, NEJM 2018; 378:2105-2114 7 Options for vein treatment 2019 Thermal with tumescent: Radiofrequency Ablation( Closure Fast) Laser Ablation (EVLT, ELVes, VeinSeal) Nonthermal Nontumescent: Mechanical Occlusion chemically assisted ablation (Clarivein) Cyanoacrylate Closure (Venaseal) Polidocanol endovenous microfoam (Varithena) Nonthermal Tumescent: Inversion Stripping with Tumescence 8 4
4/4/2019 Considerations in the treatment of superficial venous insufficiency and varicose veins Vein diameter Vein length (especially for recurrent reflux or accessory veins) Tortuosity Vein location (suprafascial vs intrafascial) Vein location (above vs below the knee) Concerns regarding neighboring structures (ie. nerves) Presence of perforators Disease state (ulcers, lipodermatosclerosis, swelling) 9 10 5
4/4/2019 Problems with RF/Laser: Intra-operative discomfort of patient Length of procedure Thermal injury to surrounding structures , especially below the knee Need for tumescent Problems if vein too superficial or tortuous Development of reflux in accessory branches Need for compression postop 11 Long term durability of treatment Hamman, et al: Meta-analysis of 3 RCT and follow-up studies of 10 RCTs: >5 yr follow-up on treatment of GSVs Surgery vs EVLA vs USG-guided sclerotherapy 5 year occlusion rates with laser or RF both about 96.5% 12 6
4/4/2019 Clarivein( Merrit Medical) Mechanicochemical ablation (MOCA)-mechanical agitation of the vessel endothelia by rotating catheter tip combined with injection of a liquid sclerosant FDA approved in 2014 Medicare reimbursement in 2017 (codes 36473/4) 13 Clarivein Advantages: Disadvantages: No tumescent Need for compression Single entry site Difficult if tortuous vein Minimal intraop pain Insurance coverage issues No bruising Recannalization No nerve injury Throw away a whole power motor unit each time 14 7
4/4/2019 Clarivein results Phlebology. 2017 Dec;32(10):649-657. Mechanochemical endovenous ablation of saphenous veins using the ClariVein: A systematic review Review of 10 unique cohorts including 1521 veins Pooled short-term (6 months) success 92% Mid-term success: 2 years: 91% 3 years 87% Major complication rate 0.2% (DVT, nerve injury) 15 Venaseal (Medtronic) Website describes as “The only non -thermal, Non-tumescent, non-sclerosant Procedure” to close the vein Uses cyanoacrylate “superglue” type of adhesive to seal the vein FDA approval: 2015 Medicare coverage: codes 36482 and 36483 in 2018 16 8
4/4/2019 Venaseal (Cyanoacrylate) 17 VeClose Study 2017 242 patients with symptomatic GSV reflux At 3 years 92% had complete closure of GSV vs 92% with Closure Fast (no difference) Statistical improvement in QOL and VSS scores seen in both groups 18 9
4/4/2019 Venaseal Disadvantages: Advantages: Phlebitis rate up to 16% No tumescent Equally painful to RF Single needlestick during procedure No need for compression Difficult to advance the hose post-op stiff Venaseal catheter in No nerve injury tortuous veins, Excellent long term closure postthrombotic veins rate Can feel glue if GSV is superficial (permanent) Allergic reactions rare but require surgical excision of glue 19 Varithena (BTG) Polidocanol injectable foam FDA approved: 2013 Medicare approval 2018: CPT codes 36465/6 20 10
4/4/2019 Varithena Foam Composition • Oxygen:CO2 ratio of 65:35 with low (<0.8%) nitrogen content • Polidocanol liquid to gas ratio of approximately 1:7 by volume • Median bubble diameter of 100 µm and no bubbles greater than 500 µm 21 21 Varithena Clinical Trials • VARITHENA was evaluated in two randomized, blinded, multicenter clinical trials designed to assess the efficacy and safety of VARITHENA compared with placebo in the treatment of GSV or major accessory vein reflux disease. • VANISH- 1 and VANISH-2 Studies showed statistically significant improvement in symptoms and appearance of varicose vein disease • Downplay duplex “responders” as 1 year results showed 73% success. 22 22 11
4/4/2019 Santangelo, KT. Treating C6 Venous Disease Requires Tandem Effort. evtoday.com January 2017. 23 Varithena Advantages: Disadvantages: Can treat tortuous GSV and Multiple needle sticks varicosities Canister needs to be used No tumescent over a short time to treat multiple patients Fast procedure Need to wear compression for Comparable in net cost to RF 2 weeks Little to no intraop/postop Outcomes >1 year unclear pain Medicare will only reimburse for GSV not SSV 24 12
4/4/2019 Theraclion’s Echopulse HIFU (High-Intensity Focused Ultrasound) technology focuses high- energy ultrasound to deliver a large amount of acoustic energy to a targeted area, quickly heating localised areas of tissue. The energy of the ultrasound is concentrated in a small area. The energy released quickly raises the temperature in this area (to 80-95°C). This produces therapeutic effects through coagulation and then necrosis of the tissue in the targeted area This has been used to treat thyroid nodules and breast fibroadenomas and is now in clinical trials to treat varicose veins. May be most helpful in treating recurrences, tortuous veins, “stumps” 25 Superficial Venous Treatments All quite safe , outpatient procedures with good short- term outcomes All improve symptomatology of heaviness, aching, swelling, itching Only thermal methods have long-term follow-up and success rates at 15 years of up to 88% by duplex ultrasound. There was no clinical recurrence in the originally treated veins, however “de novo” reflux was found in 51.6% of patients in veins that were originally competent. Eur J Vasc Endovasc Surg. 2017 Sep;54(3):357-362 26 13
4/4/2019 Pharmacotherapy for Chronic Venous insufficiency MPFF: Micronized Purified Flavonoid Fraction Diosmin + Hesperidin Most investigated venoactive medication: Daflon 500 NOT APPROVED IN THE US Mechanism: inhibits noradrenaline degradation, leukocyte adhesion and activiation, TNF, VEGF Side effects: N/V in up to 7% Cost: $15-30/month 27 MPFF RELIEF trial: European trial with >5000 pts in 23 countries: Significant improvement in leg aching, heaviness, edema, and QoL A meta-analysis of 5 prospective, randomized trials in 723 patients demonstrated a 32% improvement in venous ulcer HEALING with its use (p=0.03) Coleridge-Smith. Eur J Vasc Endovasc Surg. 2005;30:198-208 28 14
4/4/2019 Diosmiplex (Vasculera) Only MPPF that is FDA approved for use in USA Classified as a “Medical Food” Addresses the Biochemical Pathway to Avoid The Progression to Chronic Venous Disease (CVD) Take once a day Side Effects: Mild, GI upset, Headache Must get through special pharmacy-- $50/month 29 Society Recommendations 30 15
Recommend
More recommend