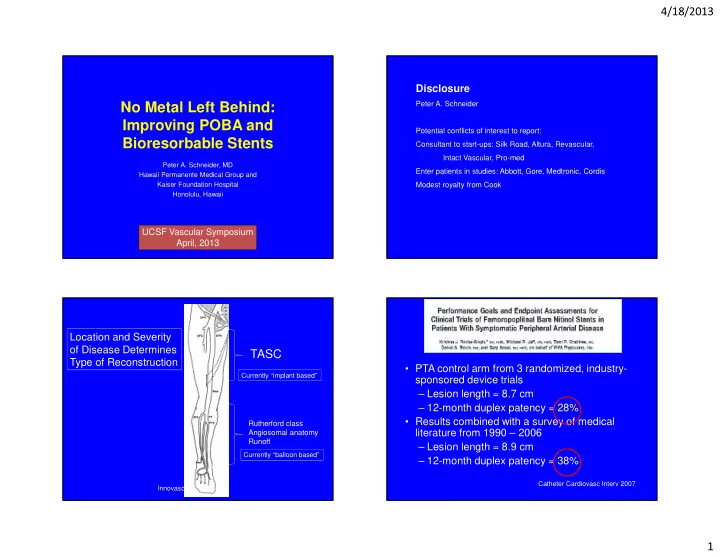
4/18/2013 Disclosure Peter A. Schneider No Metal Left Behind: Improving POBA and Potential conflicts of interest to report: Bioresorbable Stents Consultant to start-ups: Silk Road, Altura, Revascular, Intact Vascular, Pro-med Peter A. Schneider, MD Enter patients in studies: Abbott, Gore, Medtronic, Cordis Hawaii Permanente Medical Group and Kaiser Foundation Hospital Modest royalty from Cook Honolulu, Hawaii UCSF Vascular Symposium April, 2013 Location and Severity of Disease Determines TASC Type of Reconstruction • PTA control arm from 3 randomized, industry- Currently “implant based” sponsored device trials – Lesion length = 8.7 cm – 12-month duplex patency = 28% • Results combined with a survey of medical Rutherford class literature from 1990 – 2006 Angiosomal anatomy Runoff – Lesion length = 8.9 cm Currently “balloon based” – 12-month duplex patency = 38% Catheter Cardiovasc Interv 2007 Innovasc 1
4/18/2013 Problems with balloon angioplasty How Does Balloon Angioplasty Work? Achilles heal of balloon angioplasty=dissection • Equal pressure in all directions around the circumference of the irregular lumen. • Pressure increases until it overwhelms the lesion through compression and plaque fracture. • When the lesion gives way, the pressure propagates along the artery and there is usually uncontrolled damage. Anterior tibial artery dissection after long segment recanalization SFA dissections Above knee popliteal artery dissection at re-entry site Recanalizing Atherosclerotic Vessels • Balloon Angioplasty – – Minimally invasive – Technique “dissects” plaque from wall allowing adventitia to expand to maximum diameter – New larger lumen accommodates pre-existing plaque and increased cross-section for blood flow – Problems: • Plaque is not “molded” but dissected and fractured >40% immediate failure of PTA in uncontrolled (random) manner requiring bailout stents • Plaque often “falls into” lumen � obstruction • Irregularity of “injury” and plaque conformation can initiate restenosis � reaction to injury 8 2
4/18/2013 SFA Treatment Femoral-popliteal Disease Stent Results TASC C and D Trial Patency Lesion 12 months Length Fast 68% 4.4 cm Resilient 80% 6.2 cm TASC Durability 72% 9.3 cm A/B Astron 65% 9.9 cm C lesions: Surgery preferred D lesions: Surgery treatment of choice Vienna 68% 10.9 cm unless high risk 35-50% stent bailout rate in current SFA trials SFA Treatment SFA Treatment Our Challenge Patency at Patency at 139 limbs 12 months 24 months TASC C stent 83% 80% Poor results in more TASC D stent 54% 28% complex lesions. Above knee 81% 75% PTFE fem-pop Surowiec et al. JVS, 2005 Dosluoglu et al. J Vasc Surg 2008;48:1166 3
4/18/2013 Is it possible: The poor results of long lesions are due as much to stent length as they are to lesion length? Primary Patency No. of 12 24 36 patients months months months TASC A/B 46/82 79% 67% 57% TASC D: Diminished patency TASC C/D 38/35 53% 36% 19% at 12 and 24 months. 210 patients DeRubertis et al. J Vasc Surg 2007 Dearing et al J Vasc Surg 2009;50:542. Baril et al. J Vasc Surg 2010 SFA Treatment Failed SFA Intervention Conformational Forces After primary stent, TASC C and D lesions are more likely to fail with occlusion rather than stenosis, lose run-off vessels, and extend the length of contiguous diseased arterial segments than their TASC A and B counterparts. Dramatic changes in configuration with movement. J Vasc Surg 2011; 53: 658-67 Klein et al.Catheter Cardiovasc Interv 2009;74:799 4
4/18/2013 Long segment SFA recanalization Recanalizing Atherosclerotic Vessels • Stents – Effective apposition of dissected plaque to expanded lumen wall – Problems • Large amount of foreign body • Rigidity of stent / fracture / micro- trauma • Restenosis • Poor options for reintervention Lower Extremity Stents Our Challenge Too Much Scaffolding • Too much metal to artery interaction Factors Associated with Stent Failure • Too much outward force • Stent overlap • Chronic outward force • Tissue apposition rather than scaffolding • Stent material PTA technique • Strut thickness • Stent length Focal support-Spot stenting, Tack • Design/Fracture Balloon angioplasty Stents No one volunteers Bioabsorbables Cha et al. Invest Radiol 2003;38:95. for a full metal jacket! Joner et al. J Am Coll Cardiol 2006;48:193. Finn et al. Circulation 2007;115:2435. Lau et al. J Invasive Cardiol 2004;16:411. Sigwart et al. N Engl J Med 1087;316:701. We need a new paradigm Bertrand et al. J Am Coll Cardiol 1998;32: 562. Verheye et al. Arterioscler Thromb Vasc Biol 2000;20:1168. Nelken et al. Surg Clin N Am 2004;84:1203. 5
4/18/2013 No Metal Left Behind: Improving POBA and Bioresorbable Stents Bioresorbable Vascular Scaffold Improve Balloon Angioplasty Technique • Use a balloon that covers the entire length of the lesion. • Increase pressure gradually so that it is only as high as it needs to be to dilate the lesion. • Leave balloon inflated for 2-3 minutes. • Repeat if necessary. CAUTION: Investigational use only. Not available for sale in or outside the U.S. Bioresorbable Stent Bioresorbable Stent Bioabsorable Stent Technology Overview Rationale: Mechanical support at the treatment site is needed transiently. • Product(s) / Technology overview: • Provide acceptable lumen after treatment, then resorb naturally • Polymer (PLLA) vs metal alloy into the body, leaving the vessel in its native state. (magnesium) • No implant left behind • Challenges: degradation rate, control of – No permanent implant – restore natural vascular response to physiological stimuli and potentially late expansive remodeling radial force, diameter sizing, brittleness, – No stimulus for chronic inflammation cost – Future re-intervention is facilitated – Compatible with non-invasive diagnostic imaging 6
4/18/2013 1 st Gen Porcine Coronary Safety Study: Post-procedure Representative Photomicrographs (2x) Porcine Coronary Artery Model E D BVS Pre-procedure C 1 month 3 months 1 year 2 years 3 years 6 months B A CYPHER 1 month 3 months 6 months 1 year 2 years 3 years B E A C D Representative photomicrographs 2X. Igaki-Tamai bioabsorbable stent in the SFA Igaki-Tamai bioabsorbable stent in the SFA Bioresorbable Scaffolds in the Peripheral Vasculature Bioresorbable Scaffolds in the Peripheral Vasculature Study Device Lesions n Outcome IGAKI Kurz 100 PERSEUS SFA 45 50% restenosis @ 6-mos. prim. Patency ass. prim. Patency 80 BE Poly-l-lactic acid sec. Patency Percent 60 BEST BTK infrapopliteal 20 90% clinical patency @ 3-mos. 40 AMS INSIGHT infrapopliteal 37 68% restenosis @ 6-mos. 20 BE Magnesium alloy 0 0 6 12 18 24 30 Tamai H, Igaki K, Kyo E, Kosuga K, Kawashima A, Matsui S, et al. Circ. 2000; 102(4):399-404. Waksman R. Cardiovascular Revascularization Therapeutics. Washington, D.C., 2007. Month Erbel R, Di Mario C, Bartunek J, Bonnier J, de Bruyne B, Eberli FR, et al. Lancet 2007; 369:1869-1875. Bosiers M, Peeters P, D ’ Archambeau O, et al. AMS INSIGHT - Absorbable metals stent implantation for treatment of below-the-knee critical limb Peeters P, Bosiers M, Verbist J, Deloose K, Heublein B. J. Endovasc. Ther. 2005; 12:1-5. ischemia: 6-month analysis. Cardiovasc. Intervent. Radiol. 2009. Schmidt A. Bioabsorbable stents: The Igaki-Tamai Stent. 2010. www.CRTonline.com. 7
4/18/2013 AMS INSIGHT – 6-mos. patency results AMS INSIGHT – 6-mos. patency results New Studies of Lower Extremity Bioabsorbable Stent • ESPIRIT I – SFA and iliac, 30 patients, December 2011 – Bioabsorbable Drug Eluting Vascular Scaffolds – Everolimus, same polymer as ABSORB – New scaffold design, larger diameter, longer length • ABSORB BTK in CLI – CLI, infrapopliteal, September 2011 – ABSORB device, CE mark for coronary artery disease Bosiers M, Peeters P, D ’ Archambeau O, Hendriks J, Pilger E, Duber C, Zeller T, Gussmann A, Lohle PNM, Minar E, Scheinert D, Hausegger K, Schulte K-L, Verbist J, Deloose K, Lammer J. AMS INSIGHT - Absorbable metals stent implantation for treatment of below-the-knee critical limb ischemia: 6-month analysis. Cardiovasc. Intervent. Radiol. 2009. Outward Force Tack: Key Components Commercially available stent Supporting Frame High outward force Self expanding Always changing with artery diameter Nitinol, supports Inner Circle of 6 Anchor Fixation: Anchor Fixation Therapeutic components component: 6 pair of anchors Short length tack down focal (6.0mm), effective irregularities Tack implant: less metal, less friction Pressure delivered at Focal Points Hinged design prevents Diameter (mm) Radiopaque watermelon seeding Markers: 6 RO Substantially lower outward force than commercially available stents during delivery markers aid in Same low outward force over a broad range of diameters visualization 8
4/18/2013 Tack: Above the Knee Tack: IVUS Dissection Flap Seen Using Post Treatment Intravascular Ultrasound Tack Permits Tissue Apposition Above-the-knee 1 yr angio Post-PTA Completion Arteriogram SFA stenosis dissection After Tack follow-up Goal is tissue apposition with positive remodeling After Tack 33 Popliteal artery occlusion One-year angio Pre-treatment angio Post-PTA dissection Post-Tack angio 9
4/18/2013 After wire loop subintimal recalization and balloon angioplasty Re-entry site Tack placement at dissection sites Entry site 10
Recommend
More recommend