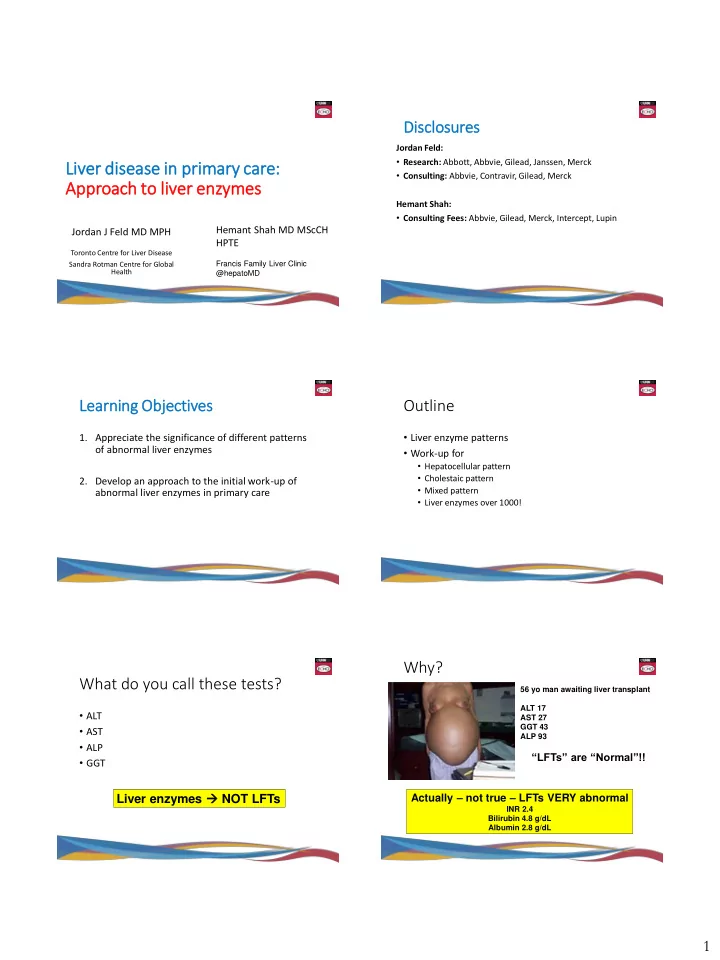
Dis isclosures Jordan Feld: • Research: Abbott, Abbvie, Gilead, Janssen, Merck Liv Liver dise diseas ase in in pr prim imary car are: • Consulting: Abbvie, Contravir, Gilead, Merck App Approach to o live liver en enzymes Hemant Shah: • Consulting Fees: Abbvie, Gilead, Merck, Intercept, Lupin Hemant Shah MD MScCH Jordan J Feld MD MPH HPTE Toronto Centre for Liver Disease Sandra Rotman Centre for Global Francis Family Liver Clinic Health @hepatoMD Learn Le arning Obje bjectives Outline • Liver enzyme patterns 1. Appreciate the significance of different patterns of abnormal liver enzymes • Work-up for • Hepatocellular pattern • Cholestaic pattern 2. Develop an approach to the initial work-up of • Mixed pattern abnormal liver enzymes in primary care • Liver enzymes over 1000! Why? What do you call these tests? 56 yo man awaiting liver transplant ALT 17 • ALT AST 27 GGT 43 • AST ALP 93 • ALP “LFTs” are “Normal”!! • GGT Liver enzymes NOT LFTs Actually – not true – LFTs VERY abnormal INR 2.4 Bilirubin 4.8 g/dL Albumin 2.8 g/dL 1
Liver tests/enzymes ≠ LFTs What do the liver enzymes mean? • Liver Functions • Ongoing injury • Synthesis: • Protein – Albumin, Clotting factors (INR) • Hepatocellular injury • Glucose – gluconeogenesis (only impaired very late) • ALT (SGPT) – L for Liver specific (small amount muscle) • Metabolism: • AST (SGOT) – lots of other sources (RBC, muscle, heart) • Bilirubin conjugation • Ammonia breakdown (encephalopathy) • Normal for both lower than the labs! • Drug/toxin breakdown • Men – ALT 30 • (Portal Hypertension) • Women – ALT 19 • Ascites • Cholestatic/infiltrative injury or obstruction • Varices • Encephalopathy • ALP (alkaline phosphatase) • GGT Liver function tests : INR, albumin, bilirubin (direct) Hepatocellular Pattern Categorization (ALT/AST) • Most useful relative to upper limit of normal • Organization is key • Hepatocellular pattern (ALT/ULN >> ALP/ULN) • Infectious • Cholestatic/infiltrative pattern (opposite) • Toxic • Mixed (ALT/ULN ≈ ALP/ULN) This should be the focus • Metabolic • Helps with narrowing a broad differential • Genetic • Height & duration of elevation also important • Autoimmune • Check trend ie historical labs Probably leave this stuff for us to do • Other Infectious Toxin • Medications, medications, medications Screen EVERYONE! • HBV (HBsAg, anti-HBc, anti-HBs) Common enough • Almost any drug can do it to screen even if • HCV (anti-HCV Ab) • Take a good history may have stopped the drug ALT normal (ask about drugs in past 3 months) • Antibiotics (Amox/Clav!!, minocycline, nitrofurantoin) Screen Selectively • Don’t forget herbals, OTC and recreational drugs – • HAV – very high ALT (>1000, exposure hx) – IgM need to ask • CMV/EBV – immunosuppressed, ALP elevated 2
Alcohol – how much is too much? Metabolic – fatty liver • History is everything • AST>ALT (2:1) (+GGT) • ALT> AST (+ GGT) • CAGE questionnaire • • Trust your patients (mostly) Metabolic risk factors • • If ALT>500 not alcohol DM, HTN, lipids alone • Weight gain or loss • Still screen for HCV, Men: 1-2 per day HBV & ETOH – not Women: 1 per day mutually exclusive! • More to come… Avoid binge drinking Avoid daily drinking Genetic Autoimmune?? • Hemochromatosis • Diagnosis is not straightforward • Not rare in Caucasians (think Vikings – northern Europe) • Fe Sat > 50%, Ferritin • Variable presentation from asymptomatic liver test • But both can be up in ETOH or Fatty liver disease abnormalities to fulminant liver failure • Again…not mutually exclusive! • Useful diagnosis because it has a bad prognosis and • More likely if also DM, arthritis, bronzing of the skin… etc it’s treatable! • Start with IgG if high, follow with ANA, SMA (and • Wilson Disease LKM if children) and biopsy (or just refer!) • Screen all if < 30 and maybe all up to age 50 • Ceruloplasmin • Bad to miss this – deadly disease that is treatable A few ‘general’ rules So bottom line – ALT/AST • Etiology Search • ALT>AST – most liver diseases • History – meds, alcohol & other drugs • Viral hepatitis • HBV, HCV for everyone, (HAV, other viruses in context) • NAFLD/NASH • Fe Sat/ferritin for everyone • Most drug induced liver injury • (ceruloplasmin) • (IgG – if persistent) • AST>ALT • Severity assessment • Alcohol – >2:1 ratio • CBC – low platelets suggest cirrhosis or acute alcohol • Ischemia (low flow or congestion) • Bilirubin, INR, Albumin (if persistent) • Wilson disease (hemolysis – 4:1) • Ultrasound (if persistent) • Cirrhosis!! (AST>ALT but <2:1) 3
What about high ALP? Cholestatic • First prove it’s from the liver GGT (usually up), ALP isoenzymes • Rule out obstruction US usually adequate • GGT is pretty useless on its own – VERY non-specific • If painless jaundice need to see pancreas (CT or MRCP) (almost any liver disease) and inducible (by meds) • Cholestatic • If no obstruction (this is where we come in…): • Extra-hepatic obstruction (stone/tumor) • Large Ducts: Primary/Secondary Sclerosing Cholangitis • Intrahepatic duct disease (stones, IgG4) MRCP • Cholestasis (poor bile flow) – e.g. alcohol!! • Small Ducts : Primary Biliary Cholangitis, vanishing bile duct syndrome, portal biliopathy (PV thrombosis) biopsy • Infiltrative • Granulomatous • Drugs (or alcohol) history +/- biopsy • Mass / tumor High ALP – Work-up Granulomatous/Infiltrative History Labs/Radiology • Symptoms – may be absent • GGT – confirm liver (ie not • Granulomatous (biopsy) • Itch bone, placenta etc) • Sarcoid • Jaundice (dark urine – • Imaging – US • TB/Fungal useful for timing) • Pain, Fever (stones) • If high suspicion, CT/MR even • Schistosomiasis – even years after leaving endemic area • Constitutional symptoms if US negative • DRUGS + Herbals • Etiology: • Infiltrative (imaging +/- biopsy) • Risk factors for TB, HCC • Anti-mitochondrial Ab (PBC) • Lymphoma • History of IBD (PSC), past • Immunoglobulins (IgG, IgM) stones, surgery (chole), • Mass lesion (HCC, mets, abscess, hydatid cyst) • Biopsy bone disease Mixed Picture A good list to remember – ALT>1000 • Similar approach to hepatocellular (AST/ALT) 1. Virus 2. Toxin • A few common ones: 3. Vascular • Meds – antibiotics! 4. Stone • Alcohol – acute alcoholic hepatitis • Stones – AST/ALT up first followed by ALP (+/- Bili) 5. Autoimmune hepatitis • Sepsis • Viruses – CMV/EBV (not HBV, HCV) Not alcohol (unless alcohol plus) • Rarer conditions (overlap syndromes etc) 4
Viral Infection (ALT>1000) Toxin (ALT>1000) • Hepatitis A to E • A – HAV IgM – only order if ALT very high &/or exposure • Medications, medications, medications • B – flare or acute infection • Take a good history may have stopped the drug • C – rare unless acute (if high suspicion, HCV RNA) • D – super-infection with HBV or flare (ask about drugs in past 3 months) • E – think Hep A (travel history) • Acetaminophen classic • CMV/EBV • Many others • Rare to be >1000, usually cholestatic too (ALP up) • Don’t forget herbals, OTC and recreational drugs – • HSV need to ask • Important – if you think of it, start the acyclovir! • Rare – VZV, SARS, influenza, adenovirus Vascular (ALT>1000) Stone (ALT>1000) • Forward flow – Shock Liver • ALT and AST go up BEFORE ALP and Bilirubin • Usually underlying cardiac disease • Typically associated with pain +/- fever (others may • Rapid increase and rapid normalization be asymptomatic) • Mild affect on liver function (INR may go up transiently) • Prompt normalization with passing of the stone • Congestion • Acute Budd-Chiari • Even severe heart failure (not very common) Liver Disease Catches You By Autoimmune Hepatitis Surprise… (ALT>1000) • Not all that common but you have to think of it • Diagnostic tests: • Quantitative immunoglobulins IgG • ANA • Smooth Muscle Antibody • Liver Kidney Microsomal (Type II – children) • Liver biopsy 5
Recommend
More recommend