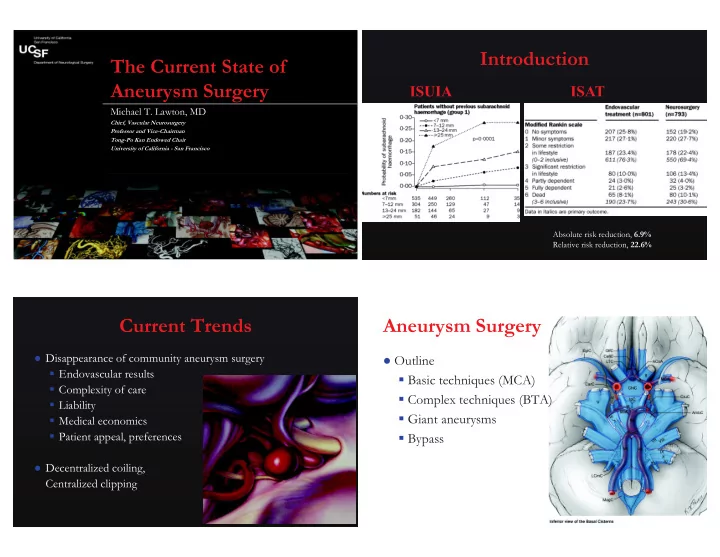
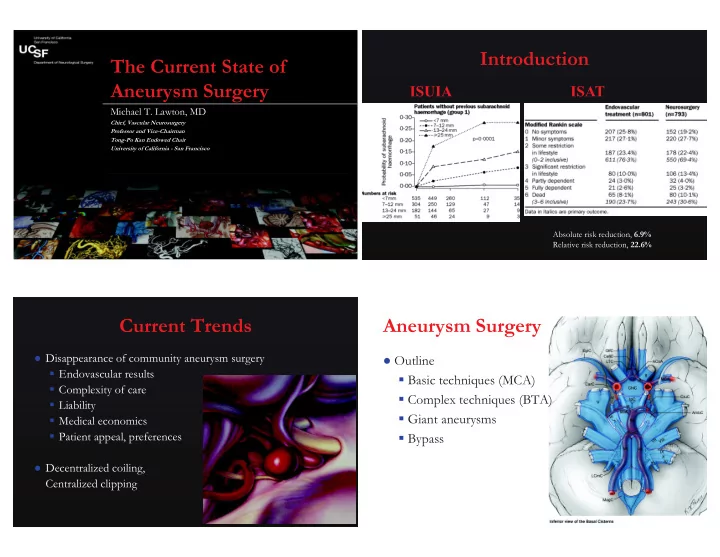
Introduction The Current State of Aneurysm Surgery Michael T. Lawton, MD Chief, Vascular Neurosurgery Professor and Vice-Chairman Tong-Po Kan Endowed Chair University of California - San Francisco Absolute risk reduction, 6.9% Relative risk reduction, 22.6% Current Trends Aneurysm Surgery Disappearance of community aneurysm surgery Outline § Endovascular results § Basic techniques (MCA) § Complexity of care § Complex techniques (BTA) § Liability § Giant aneurysms § Medical economics § Patient appeal, preferences § Bypass Decentralized coiling, Centralized clipping
MCA Aneurysms UCSF Experience Consecutive series, single surgeon “Clip First” Policy: § Favorable surgical anatomy Review period (years) 14 § Endovascular limitations Total aneurysms 3000 § Simple exposure Total patients 2301 § Multiple surgical options MCA aneurysms 805 § Minimally invasive, retractorless MCA aneurysm patients 701 § Low therapeutic risk Percentage 25% § Good outcomes Most common aneurysm Sylvian Split Sylvian Veins
Fissures MCA Aneurysm Dissection
MCA Aneurysm Clipping Clipping Techniques Endovascular Therapy for MCA Aneurysms � ✁ ✂ ✄ ✞ ✟ ☎ ✆ ✝ ✠ ✞ ✞ ✞ ✌ ✍ ✞ ✟ ✎ ✞ ✡ ☛ ✡ ☞ ☎ ✡ ✝ ☎ ✆ ✝ ✆ ✏ ✆ ✑
Aneurysm Projection
Contralateral MCA Clipping Aneurysm Surgery Outline § Basic techniques (MCA) § Complex techniques (BTA) § Giant aneurysms § Bypass
ISAT Current Practice Eligible patients 9559 Charing Cross Hospital, London “All posterior circulation aneurysms, if Excluded patients 7416 Included patients 2143 technically feasible, were coiled” Aneurysm unsuitable for Anterior circulation 2085 Mayo Clinic, USA clipping or coiling Posterior circulation 58 (2.7%) Uncertainty about best tx (lack “Endovascular treatment is definitely superior § Basilar apex 26 of equipoise) to surgical clip ligation of basilar bifurcation § PICA 31 aneurysms” ✒ ✔ ✗ ✢ ✦ ✦ ★ ✦ ✖ ✖ ✖ ✖ ✖ ✓ ✕ ✕ ✕ ✓ ✘ ✙ ✕ ✚ ✕ ✛ ✙ ✜ ✜ ✚ ✓ ✣ ✓ ✤ ✜ ✥ ✓ ✥ ✧ ✥ ✧ ✘ ✕ ✓ ✚ ✕ ✚ ✜ ✘ ✥ ✩ ✙ ✤ ✤ Posterior Circulation Aneurysms Cisterns Technically difficult, high morbidity Endovascular option is appealing Absence of definitive data What should neurosurgeons be doing? § Stop clipping § Limit aneurysm surgeons § Selected aneurysms
Triangles Temporal Lobe Basilar Aneurysm Dissection Basilar Aneurysm Dissection
✵ ✯ ✰ ✴ ✳ ✭ ✲ ✰ ✮ ✱ ✮ ✯ ✰ ✮ ✭ ✬ ✪ ✫ ✶ ✺ ✻ ✷ ✾ ✸ ✽ ✹ ✻ ✼ ✹ ✺ ✻ ✹ ✷ ✸ ✁ ✶
Transcavernous Approach Transcavernous Approach Indications § Low-riding aneurysm § No proximal control § Too tight Technique § Anterior clinoidectomy § Posterior clinoidectomy § Unroof cavernous sinus Anterior Clinoidectomy Anterior Clinoidectomy
Anterior Clinoidectomy Anterior Clinoidectomy Posterior Clinoidectomy
Transcavernous Approach UCSF Experience Basilar Apex Aneurysms Consecutive series, single surgeon Aneurysm surgeons should not abandon basilar aneurysms Review period (years) 14 Best therapy for basilar aneurysms is unclear Total aneurysms 3000 Endovascular therapy is eroding case volume, Total patients 2301 neurosurgical manpower, and technical proficiency Basilar apex aneurysms 317 Surgery preferred for aneurysms with broad necks, large and giant size, abnormal branches, thrombus Percentage 10% Most difficult aneurysm
Aneurysm Surgery Endovascular Therapy Outline The problem with coiling giant aneurysms: § Basic techniques (MCA) § Incomplete aneurysm obliteration § Coil compaction/extrusion § Complex techniques (BTA) § Recurrence, rehemorrhage, retreatment § Giant aneurysms § Bypass � ✁ ✂ ✿ ✺ ❀ ✺ ❂ ✷ ❄ ✻ ✶ ❁ ❃ ✻ ✶ ❅ Endovascular Results Endovascular Therapy Total patients 38 Giant aneurysms 39 Complete occlusion 36% Need for stent 66% Sessions/aneurysm 1.9 Cumulative Morbidity 12 32% Cumulative Mortality 6 16% Follow-up (months) 25 Late Morbidity 10 26% Late Mortality 11 29% ❪ ✢ ✦ ✦ ❫ ✦ ✔ ✦ ✦ ✦ ✖ ✖ ✕ ✥ ✚ ✤ ✓ ✙ ✥ ✤ ✛ ✕ ✚ ✕ ✚ ✜ ✘ ✥ ✩ ✙ ✤ ✤ ✚ ✓ ✕ ✧ ✥ ✓ ✚ ✧ ✤ ✜ ✕ ✤ ✜ ✥ ✜ ❴ ✘ ✥ ✚ ✛ ✦ ★ ★ ✔ ✦ ❜ ✔ ★ ✦ ❆ ❈ ● ■ ▼ ❖ ● ❙ ❯ ❳ ❨ ❩ ❬ ❬ ❭ ✖ ✖ ✖ ✖ ❇ ❉ ❊ ❋ ❏ ❑ ▲ ❊ ◆ P ◗ ❏ ❘ ❇ ❏ ❉ ❱ ❊ ◗ ❉ ❱ ❏ ❲ ❉ ▲ ✤ ✘ ✥ ❵ ✜ ✕ ✚ ✧ ✜ ✥ ✜ ✥ ✜ ✕ ✙ ✜ ✚ ✤ ✥ ✜ ✣ ✕ ✜ ✜ ✥ ✤ ✜ ✣ ❝ ✓ ✤ ✘ ✥ ✜ ✕ ✚ ✥ ✜ ✕ ✣ ✤ ✚ ✛ ✧ ✓ ✘ ✥ ✤ ✜ ❍ ❍ ❍ ❍ ❚ ❛ ❛ ❛
UCSF Experience UCSF Experience Consecutive series, single surgeon Anterior Circulation Posterior Circulation Cavernous 19 ❞ Review period (years) 14 Supraclinoid ICA 18 Basilar Bifurcation 14 ❞ ❞ Total aneurysms 3000 Ophthalmic 15 SCA 2 ❞ ❞ Total patients 2301 Superior Hypophyseal 5 PCA 7 ❞ ❞ Posterior Communicating 5 Basilar Trunk 9 Giant aneurysms ❞ 168 ❞ MCA 23 PICA 4 ❞ ❞ Giant aneurysm patients 167 Anterior Communicating 13 Vertebral Artery 5 ❞ ❞ Percentage 5.6% Pericallosal 2 ❞ Giant aneurysms remain a surgical disease Total 100 Total 41 ❞ ❞ Pre-Op Direct Clipping Post-Op
Direct Clipping Post-Op Pre-Op Tandem Angle Fenestrated Clipping
Fenestration Tube Post-Op Pre-Op
Clip Reconstruction UCSF Experience Direct Aneurysm Occlusion § Neck clipping 64 45% § Neck clipping + bypass 2 1% Indirect Aneurysm Occlusion ✼ ✺ ❀ ❣ ❀ ✺ ✹ ✻ ❡ ❃ ❢ ✾ ✾ ❤ ❅ ✻ ✶ § Parent artery clipping 20 14% § Parent artery clipping + bypass 29 21% § Endovascular occlusion + bypass 23 16% Other 3 2%
Patient Outcomes Giant Aneurysms Neurologically improved or unchanged 106 75% Coiling is ineffectual, due to high rates of incomplete Surgical Mortality 18 13% obliteration, recurrence, and retreatment Permanent neurological morbidity 16 11% Flow diversion is unproven, but may offer a better endovascular option than coiling, particular in posterior Complications circulation § Surgical 8 6% Conventional clipping is preferred, often inadequate § Medical 11 8% Complete Aneurysm occlusion 108 77% Hypothermic circulatory arrest is rarely indicated Recurrence/retreatment 2 1.4% Bypass used frequent, enabling reconstruction or indirect Late rehemorrhage 0 0% aneurysm occlusion Aneurysm Surgery Bypass Surgery Outline Same old techniques § Basic techniques (MCA) More advanced applications § Complex techniques (BTA) Technical evolution § Giant aneurysms ( not technological evolution) § Bypass Pushing the envelope
Arterial Reconstruction (IC-IC) Evolution of Bypass Surgery 1 st Generation STA-MCA Bypass Technique Total MCA ACA PICA Basilar 2 nd Generation EC-IC Bypass In Situ Bypass 16 3 3 9 1 3 rd Generation IC-IC Bypass Reimplantation 12 1 1 9 1 Reanastomosis 20 9 1 10 0 Graft Reconstruction 17 4 3 1 9 Hypothesis: Total 65 17 8 29 11 § IC-IC bypass = EC-IC bypasses § Move to intracranial reconstruction Bypasses for Aneurysms, 138 PICA IC-IC Bypass Technique Anastomosis In Situ Bypass Side-to-Side ❞ Reanastomosis End-to-End ❞ Reimplantation End-to-Side ❞ Intracranial Bypass Graft, 2x ❞ Sites § Sylvian fissure § Interhemispheric fissure § Carotid, crural cisterns § Cisterna magna
PICA-PICA Bypass PICA Reanastomosis PICA Reanastomosis
Triangles PICA Reimplantation PICA Reimplantation
MCA MCA Aneurysm MCA Reanastomosis MCA Reanastomosis
Excision - Reanastomosis ACA Pericallosal Reimplantation
Pericallosal Reimplantation Pericallosal Reimplantation Basilar Apex PCA Dissecting Aneurysm Presentation Endoscopic resection New aneurysm
SCA-PCA In Situ Bypass SCA-PCA In Situ Bypass UCSF Experience Bypass Old-fashioned microsurgery can create elegant Consecutive series, single surgeon bypasses Review period (years) 14 Data support intracranial bypass Total aneurysms 3000 Suture, meticulous technique will advance us Total patients 2301 from EC-IC to IC-IC bypasses Bypasses 291 ELANA, staplers, will not facilitate IC-IC bypasses Bypasses for aneurysms 121 Evolution depends on mastering arterial Percentage of aneurysms 4% anastomosis in all its variations and expending extra effort
Current Trends Vascular Volume 3500 Total = 3195 Endovascular Surgical Aneurysm 3195 600 AVM 3000 Patient demand ! " 527 Cav Mal 316 Bypass 2500 Case volume ! " Neurosurgeons ! " 2000 Centralization " ! 1500 Selectivity " ! 1000 Expertise ! " Complexity - ! 500 ✐ ✔ ✔ 0 ✚ ✜ ✘ ✥ ✩ ✙ ✤ ✤ ✘ ✥ ✛ ✜ ✓ ✚ ✤ ✕ ✥ ✜ ✚ ✜ ✜ ✜ 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 UCSF Center for Stroke & Cerebrovascular Diseases 877/BRAIN – 1 – 1
Recommend
More recommend