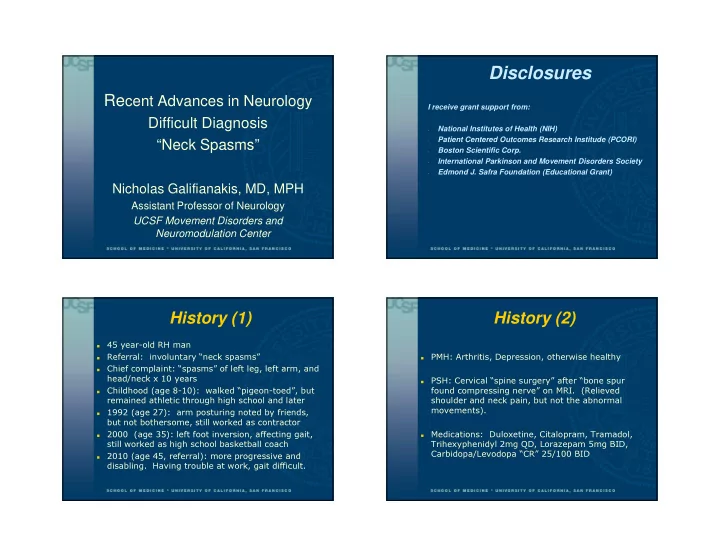
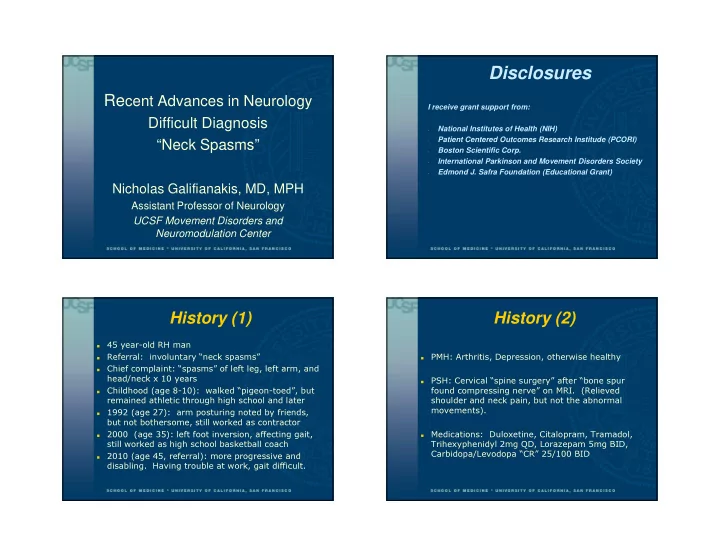
2/10/2017 Disclosures Re cent Advances in Neurology I receive grant support from: Difficult Diagnosis National Institutes of Health (NIH) - Patient Centered Outcomes Research Institude (PCORI) “Neck Spasms” - Boston Scientific Corp. - International Parkinson and Movement Disorders Society - Edmond J. Safra Foundation (Educational Grant) - Nicholas Galifianakis, MD, MPH Assistant Professor of Neurology UCSF Movement Disorders and Neuromodulation Center History (1) History (2) 45 year-old RH man � Referral: involuntary “neck spasms” PMH: Arthritis, Depression, otherwise healthy � � Chief complaint: “spasms” of left leg, left arm, and � head/neck x 10 years PSH: Cervical “spine surgery” after “bone spur � Childhood (age 8-10): walked “pigeon-toed”, but found compressing nerve” on MRI. (Relieved � remained athletic through high school and later shoulder and neck pain, but not the abnormal movements). 1992 (age 27): arm posturing noted by friends, � but not bothersome, still worked as contractor 2000 (age 35): left foot inversion, affecting gait, Medications: Duloxetine, Citalopram, Tramadol, � � still worked as high school basketball coach Trihexyphenidyl 2mg QD, Lorazepam 5mg BID, Carbidopa/Levodopa “CR” 25/100 BID 2010 (age 45, referral): more progressive and � disabling. Having trouble at work, gait difficult. 1
2/10/2017 History (3) Examination (1) ROS: (+)Gait disturbance, occasional falls. General examination was normal. � � No cognitive, behavioral, autonomic complaints. No � sensory complaints (except painful muscle spasms. On neurologic examination: � No weakness, no change in speech/swallowing). � Mental status was normal. Memory, language, attention, naming, and visuospatial function were normal. SH: Married with 5 adopted children. College � � Cranial nerve examination was normal, with graduate, now working as substitute teacher, normal voice and facial expression. basketball coach. No substance use/exposure. � Sensation and coordination were normal. � DTRs brisk throughout, including crossed adductors, FH: younger brother (age 41) recently mentioned � but no Babinski sign. stiffness and abnormal movements on one side. English/German ancestry. Examination (2) Examination (3) Movement Disorders Examination: � � Tone was minimally increased in the neck, left arm and leg (only brought out with distraction). � No tremor at rest, postures, or actions. � Rapid repetitive movements (finger taps, hand movements, heel stomps) � Possible mild bradykinesia - somewhat difficult to interpret whether just a consequence of abnormal movement 2
2/10/2017 Question #1 Dystonia The predominant phenomenology of abnormal Movement disorder � movements seen in this examination is most consistent characterized by with: sustained/intermittent Chorea A. muscular contractions Dyskinesia causing abnormal B. 86% repetitive movements, Parkinsonism C. postures, or both Dystonia D. Typically patterned, � twisting, and may be tremulous Often initiated or worsened 9% � 4% Dystonia Consensus Update 1% by voluntary action, a/w (Jinnah, Delong, Hallett. overflow muscle activation a a Movement Disorders. 2013) a m e s i n i r e s o n n i o h t i o s C k s y s n D y i D k r a P “New” Dystonia “New” Dystonia Classification Classification Axis 1 – Clinical features Axis 2 – Etiology � � � Age of Onset (infancy, thru late adult) � Inherited � DYT genes � Body distribution (focal, segmental, generalized) � Familial Parkinsonism: YOPD/Juvenile PD � Other: Wilson’s disease, Familial BG calcifications, HD, SCA, NBIA/PKAN, Ataxia-Teleangiectasia, � Temporal pattern (static, progressive course) Neuroacanthocytosis, Lesch-Nyhan � Acquired � Isolated or Combined w/other movement disorder � Nonfamilial Parkinsonism: PD, MSA, CBD, PSP… (e.g. parkinsonism, myoclonus, etc..) � Tardive syndromes (DRBA exposure), toxic � Other: Brain injury, ischemic, metabolic … � Our Case: Axis 1: Childhood onset, generalized, progressive, isolated vs combined dystonia. � Idiopathic 3
2/10/2017 Prior Work-up/Mgmt Prior Work-up/Mgmt Metabolic labs, Thyroid labs, vitamin E level, Levodopa responsive? � � ceruloplasmin, and anti-GAD antibodies all normal. � Do symptoms worsen right before next dose, or if you miss a dose?” � “Not sure” MRI Brain normal � � Is there a particular time of day when you are at your MRI cervical spine showed a “bone spur � worst? compressing a nerve” � “Yes, in the morning…” � “Wake up with legs very stiff, and bent over” (*) Levodopa 25/100 BID “helped”, but not clear � � “Straighten up” after morning meds. whether trihexyphenidyl, tramadol, lorazepam Differential Diagnosis (Axis Differential Dx 2 – Etiology) Our Case: Axis 1: Childhood onset, generalized, Familial dystonia (DYT genes) � progressive, isolated vs combined... DYT1 most common: � � Most commonly presents in childhood, legs Inherited Dystonia (“Primary”) � Usually becomes generalized over course of � childhood/adolescence Other DYTs: a diverse group, some a/w � Acquired Dystonia (“Secondary”) � Parkinsonism, Ataxia, rarely dopamine responsive � DYT3 (Lubag) Dopamine-responsive Dystonia (DRD) � � DYT5 (Segawa = DRD) Young-onset Parkinson’s Disease (YOPD) � Other acquired (brain injury, tardive, ischemic, etc…) 4
2/10/2017 Differential Dx: DRD Differential Dx: YOPD Dopamine-Responsive Dystonia (DRD) Young onset Parkinson’s disease (YOPD) � Group of familial disorders with mutations in the Symptom onset <40 years old � � enzymatic pathway of dopamine synthesis Parkin, PINK1, LRRK2 most common genes found � DYT5: GTP Cyclohydrolase (GCH1), (Segawa in this group (but still don’t account for majority) � Syndrome), Tyrosine Hydroxylase (TH) Onset in Childhood � More tremor, more dystonic cramps/posturing � Diurnal pattern of sensitivity (best in a.m.) � Slower progression � Very responsive to low-dose Levodopa � Earlier dyskinesia � Not neurodegenerative � Better response to meds and DBS � Negative genetic tests do NOT exclude DRD � Question #2 Question #3 All of the following would be helpful in distinguishing Which of the following is the most likely diagnosis at this Dopamine-Responsive Dystonia (DRD) and other dystonias time? from Neurodegenerative Parkinsonism (PD) EXCEPT: Dystonic Cerebral Palsy A. Young Onset Parkinson’s disease Response to Levodopa (e.g. On/off testing) A. B. 51% Dopamine transporter (DAT) Scan Dopamine-Responsive Dystonia B. 78% C. (Segawa) Response to Botulinum toxin injection C. Genetic testing (DRD + Familial PD panels) DYT-3 Dystonia (Lubag) D. D. 25% 21% 3% 9% 9% 5% Dystonic Cerebral Palsy DYT-3 Dystonia (Lubag) Young Onset Parkinson’s ... Dopamine-Responsive Dy... . . . . . e . . . . . . t a ( ( . m F a p r + e u o t n D d r i o l R o p u D v t e s o ( n g L a B o n r o i t t t t e e s n e e s s t n i n o m o c t i p a p e s p s e o e n e R D R G 5
2/10/2017 Diagnosis PARK2 (Parkin) YOPD Genetic testing: DRD and PD panels revealed … Found in 1998, several Japanese families (REF) � � DYT1, DYT5 (GCH1, TH), PINK1 (PARK6), 6p27, deletions in 1+ exons � � LRRK2 (PARK8) = Negative Parkin (PARK2) (+) � #1 cause of YOPD/EOPD (onset < 40, mean 27) � � Predicted disease-associated mutations: #1 cause (and majority) of AR PD � � Homozygous Deletion of Exon 4 � Deletion in Exon 1 Diurnal fluctuations, improvement after sleep � � Potential adjacent disease-associated mutations Initially mild, slow progression, rare ANS/Cog. � (deletions in exons 2, 3, 5) � Very responsive to Levodopa � Leg dystonia very common (>90%) Diagnosis: Parkin (PARK2)(+) YOPD � � Pathology: Absence of Lewy Bodies � Case: Clinical Course Summary: DRD vs YOPD Botulinum toxin: “90%” relief of pain/laterocollis: Similarities: both prominent dystonia early (esp. in � � Left Splenius, Levator Scap, SCM, Trapz (200 units) legs), very responsive to Levodopa, better w/sleep Dramatic response to levodopa, however, � developed “motor complications” wearing off Differences: � Q2hrs, bothersome dyskinesia � DRD almost always clear onset in childhood 2012 Disability: eval for DBS, minimal non-motor � � YOPD: parkinsonism on exam (but difficult early once depression treated, MOCA 29/30. when mild rigidity/brady, and confounding dystonia). Goals: Improve fluctuations, dyskinesia, Off sx � 2013 bilateral GPi-DBS � YOPD frequently misdiagnosed as ET or Dystonia � 2016 continues to do extremely well � � Not expected in younger population � Postural component of tremor � Long period of time when Dystonia predominant sx 6
2/10/2017 THANK YOU. 7
Recommend
More recommend