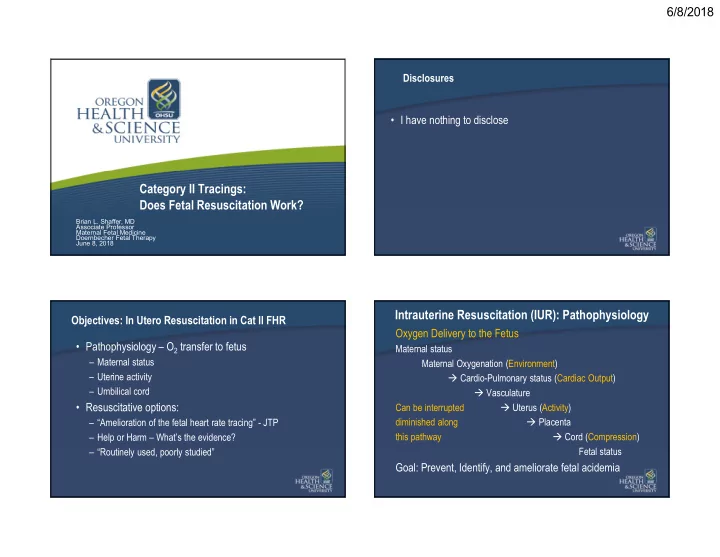
6/8/2018 Disclosures • I have nothing to disclose Category II Tracings: Does Fetal Resuscitation Work? Brian L. Shaffer, MD Associate Professor Maternal Fetal Medicine Doernbecher Fetal Therapy June 8, 2018 Intrauterine Resuscitation (IUR): Pathophysiology Objectives: In Utero Resuscitation in Cat II FHR Oxygen Delivery to the Fetus • Pathophysiology – O 2 transfer to fetus Maternal status – Maternal status Maternal Oxygenation (Environment) – Uterine activity Cardio-Pulmonary status (Cardiac Output) – Umbilical cord Vasculature • Resuscitative options: Can be interrupted Uterus (Activity) diminished along Placenta – “Amelioration of the fetal heart rate tracing” - JTP this pathway Cord (Compression) – Help or Harm – What’s the evidence? Fetal status – “Routinely used, poorly studied” Goal: Prevent, Identify, and ameliorate fetal acidemia 1
6/8/2018 IUR - Pathophysiology (cont.) IUR - Pathophysiology (cont.) • Hypoxemia Anaerobic metabolism Lactate ↓ pH • Category II – not predictive of fetal-acid base status – Requires evaluation, continued surveillance and re-evaluation • FHR monitoring: indicate risk of acidemia – Common - 2h prior to delivery: ~40% of FHR is cat II – Cat I – very low risk – Moderate variability & accelerations – Absence of acidemia – Cat III – very high risk – More “abnormal” findings higher the probability of acidemia • Immediate IUR and if not successful…. • Minimal variability, Decelerations, Tachycardia, etc… • Expeditious delivery • ~30% of fetuses demonstrate a “nonreassuring” pattern in labor • Very uncommon <1% of all FHR – Nonreassuring ≠ acid base values – With the limitations of FHR – • What can we do about it? – IUR! IUR – Goals and Actions IUR – Goals and Actions Goals “Resuscitation” Goals “Resuscitation” Deliver O 2 Lateral decubitus, IV fluid bolus Alleviate cord Lateral decubitus, Amnioinfusion (stage I) Compression Alter pushing (every 2 nd /3 rd ) To Fetus Reduce/Stop uterotonics, Alter pushing Administer O 2 (Maternal) Treat maternal Lateral decubitus, IV fluids Hypotension Meds: ephedrine, phenylephrine ↓ Uterine Lateral decubitus, IV fluid bolus, Activity Reduce/Stop Uterotonics, Tocolytic • Must consider clinical context – parity, stage, chorio, etc. • Characteristics of FHR, pattern evolution (~60 min)* • Cascade of actions – position, IV fluids... *Parer JT 2006 J Mat Fetal Neo Med 2
6/8/2018 IUR: Lateral decubitus position IUR: Lateral decubitus position • Lateral decubitus (Left or Right) • Most common intervention – Supine position Aortocaval compression • May alleviate compression with uterine wall/fetal parts • Decreases venous return & increases afterload • Prevents supine hypotension episode • Reduction of CO – up to 30% – May maximize maternal CO – May use wedge • Left more commonly utilized • Lateral position & Fetal O 2 status – Both R&L may modify uterine blood flow and assist in – Lateral position compared with supine resolution of late decelerations • Normal FHR, small number of subjects • First response to a “nonreassuring” pattern • Increased fetal O 2 by fetal pulse ox (fetal SpO 2 ) • Left and right similar increased in SpO 2 • Fetal SpO2 was lowest - supine hypotensive episode Carbonne 1996 Obstet Gynecol; Simpson KR Am J Obstet Gynecol 2005 Carbonne 1996 Obstet Gynecol; Simpson KR Am J Obstet Gynecol 2005 IUR: IV Fluid Bolus IUR: IV fluid bolus – Fetal oxygenation Sp0 2 Hypovolemia/Hypotension ↓ Uterine blood flow ↓Fetal O 2 • IVF and fetal oxygen saturation (Sp0 2 ) – IOL, oxytocin, epidural, n=56, normal FHR • IV fluid bolus – 500-1000cc NS/LR – 500 vs. 1000cc LR • Do not utilize glucose containing IVF – Increase fetal oxygen saturation (Sp0 2 ) • 1000cc increase in fetal SpO 2 - 5.2% – Increased fetal lactate, decreased pH • 500cc increase in fetal SpO 2 - 3.7% – Increased risk for fetal hyperglycemia neo hypoglycemia – Improved fetal SpO 2 in normotensive, well hydrated patients hyperinsulinsim, jaundice, TTN • Fetal pulse oxygenation? • Caution: Pre-eclampsia, Magnesium Pulmonary edema Simpson KR Obstet Gynecol 2005 Simpson KR Obstet Gynecol 2005 3
6/8/2018 IUR: IV Fluid Bolus Audience Poll 35 yo G2P1001 at 40 5/7 wks IOL for rapid labor Neuraxial anesthesia/Supine position (both!) Hypo- and SVE of 6/80/0, oxytocin at 3mu/min FHR 150s volemia/Hypotension ↓ Uterine blood flow ↓Fetal O 2 85% min-mod variability, intermittent late and severe Action: Lateral position, IVF bolus variable decelerations. Toco:q1-2 • If not corrected – Ephedrine, phenylephrine A. None, with some moderate variability the fetus is 9% – Ephedrine – mixed α and β agonist 4% 2% 0% unlikely to be acidemic, AROM and glove up • Epinephrine (α only) can constrict uterine blood flow B. Position change, Fluid bolus, O 2 CD if not resolved – Associated with marked FHR variability • Data - Few studies C. If B doesn’t work, AROM and Amnioinfusion • May reduce hypotension, but most benefit illustrated with high dose D. Oxytocin off, position change, IVF, Tocolytic if – No longer utilized in contemporary anesthesia E. No resolution 10 min • No clear benefit to FHR, hypotension – epidural, spinal Hofmeyr Cochrane Review 2010 IUR: Uterine activity IUR: Uterine activity • Contraction - Intermittent interruption of O 2 /CO 2 transfer • Contraction - Intermittent interruption of O 2 /CO 2 transfer – Tetany/Tachysystole ↓ Intervillous flow ↓Fetal O 2 – Tetany/Tachysystole ↓ Intervillous flow ↓Fetal O 2 Anaerobic metabolism Anaerobic metabolism Acidemia Acidemia • Reduction in UCs • Reduction in UCs improved perfusion improved perfusion • Action: Uterotonics • Action: Uterotonics • Limitation – pulse Ox Simpson KR Am J Obstet Gynecol 2008 Simpson KR Am J Obstet Gynecol 2008 4
6/8/2018 IUR: Excessive Uterine activity Audience Poll 35 yo G2P1001 at 40 5/7 wks IOL for rapid labor and Tachysystole - >5 UCs in 10 min (30 minutes) SVE of 6/80/0, oxytocin at 3mu/min FHR 150s min-mod • Spontaneous variability, int late and severe variable decelerations. • Induction/Augmentation: (misoprostol, Oxytocin, etc.) Toco:q1-2 Which Tocolytic? 76% • Anesthesia – Intrathecal opioids/Response A. A IV terbutaline ACTION B. B IV nitroglycerine • Reduce/Stop Uterotonics C. C IV Magnesium • Tocolytic 21% D. D SQ terbutaline – Terbutaline SQ or IV 1% 1% 0% E. E Atosiban – Nitroglycerine – Magnesium IUR: Excessive Uterine activity IUR: Excessive Uterine activity Terbutaline v Nitroglycerine (IV) Terbutaline/Beta agonists vs. No medication • Amelioration of nonreassuring FHR tracing, n=110 • Abnormal FHR, fetal scalp pH, randomized – NRFHT • Decels: Prolonged, late or severe variables; • Neonate – decrease rate of acidemia • Tachycardia + min variability • Maternal – transient maternal tachycardia – Success = complete resolution (10 min) Terbutaline (0.25mg SQ) vs. Magnesium (4gm bolus IV) Terbutaline: • Awaiting CD for FHR abnormalities – Fewer median UCs (2.9 vs. 4 UCs/10 min) – Resolution of tachysystole (1.8 vs. 18.9%) • Terbutaline reduced uterine activity (MVU) • Similar rates of successful resuscitation (72 vs. 64%, NS) • Magnesium no significantly reduced uterine activity • Maternal MAP decreased with Nitroglycerine – More neonates with CUA pH <7.2 • No differences in Ob Outcomes Kulier R Cochrane review 2009 Pullen KM AJOG 2007 5
6/8/2018 Audience Poll IUR: Suspected umbilical cord compression 29 yo G1 at 39 5/7 weeks with SOOC and SVE of 5/80/-1 FHR • Umbilical cord compression – recurrent severe 150s mod variability and recurrent severe variables. variable decelerations despite position change Toco: q2-3 • Concept: alleviate cord compression via infusion of A. A: None, with mod variability - fetus is unlikely NS/LR into the uterus with IUPC acidemic 53% • Beware of iatrogenic poly – ensure fluid egress B. B: Position change, Fluid bolus – “Fix” those variables 26% 16% C. C: Position change, Fluid bolus and O 2 4% D. D: If B doesn’t work, AROM and Amnioinfusion 0% E. E: Cesarean: too remote from delivery Hofmeyr GJ, Cochrane Review 2012 IUR: Suspected umbilical cord compression IUR: Stage II Alternate Pushing • 19 trials, n=>1000 • Consider interruption of pushing fetus to recover • Reductions in: • Decrease frequency and length of each effort – FHR decelerations (RR 0.53) – 3-4 efforts for 6-8 seconds – CD for NRFHT (RR 0.62) & Endometritis (RR 0.45) • Effort with every other UC or every third – Apgar <7 at 5 min (RR 0.47) • Some advocate laboring down – cat II? – Meconium below cords (RR 0.53) • Few adequate well designed trials to provide clear • Maternal risks recommendations – Appears to be generally safe, No increased risk in VBAC – “Street Smarts” Hofmeyr GJ, Cochrane Review 2012 6
Recommend
More recommend