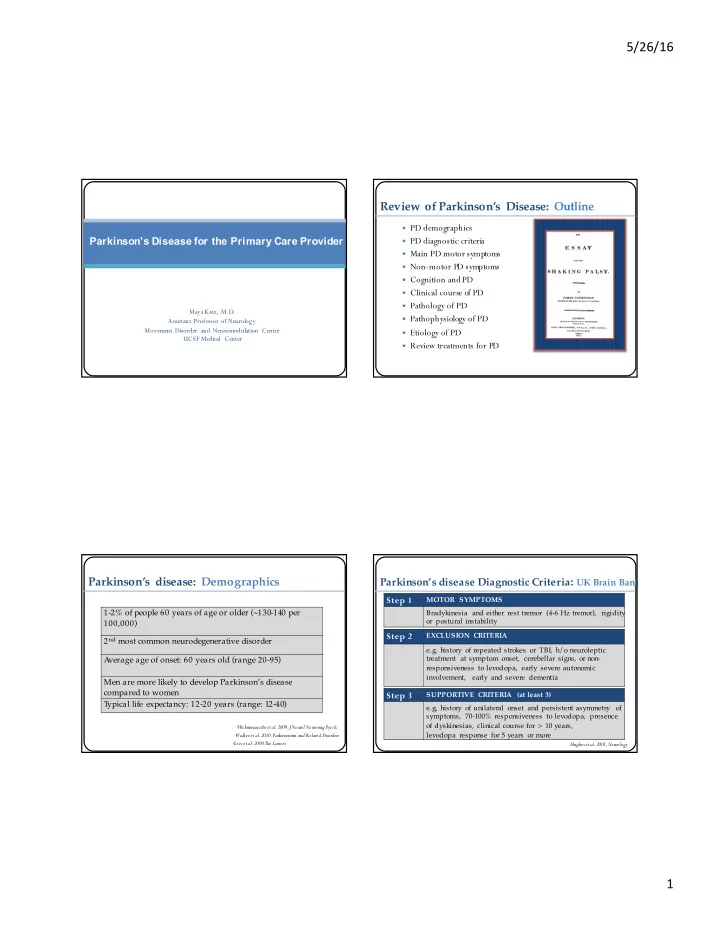
5/26/16 Review of Parkinson’s Disease: Outline PD demographics Parkinson’s Disease for the Primary Care Provider PD diagnostic criteria Main PD motor symptoms Non-motor PD symptoms Cognition and PD Clinical course of PD Pathology of PD Maya Katz, M.D . Pathophysiology of PD Assistant Professor of Neurology Movement Disorder and Neuromodulation Center Etiology of PD UCSF Medical Center Review treatments for PD Parkinson’s disease: Demographics Parkinson’s disease Diagnostic Criteria : UK Brain Bank Step 1 MOTOR SYMPTOMS 1-2% of people 60 years of age or older (~130-140 per Bradykinesia and either rest tremor (4-6 Hz tremor), rigidity or postural instability 100,000) Step 2 EXCLUSION CRITERIA 2 nd most common neurodegenerative disorder e.g. history of repeated strokes or TBI, h/o neuroleptic treatment at symptom onset, cerebellar signs, or non- A verage age of onset: 60 years old (range 20-95) responsiveness to levodopa, early severe autonomic involvement, early and severe dementia Men are more likely to develop Parkinson’s disease compared to women Step 3 SUPPORTIVE CRITERIA (at least 3) T ypical life expectancy: 12-20 years (range: 12-40) e.g, history of unilateral onset and persistent asymmetry of symptoms, 70-100% responsiveness to levodopa, presence of dyskinesias, clinical course for > 10 years, 1 Wickremaracthi et al. 2009. J Neurol Neurosurg Psych; levodopa response for 5 years or more Walker et al. 2010. Parkinsonism and Related Disorders 2 Lees et al. 2009. The Lancet Hughes et al. 2001, Neurology 1
5/26/16 Parkinson’s disease: Group A: characteristic of PD NINDS Diagnostic Criteria Cardinal motor symptoms: Tremor Resting tremor (4-6 Hz) Bradykinesia Possible Parkinson’s dise ase Rigidity At least 2 features inGroup A, w ith on e of them being either tremor or Asymmetric onset bradykinesia, no features in group B Group B: present, and sustained response to suggestive of alternative diagnosis dopaminergic therapy Onset of the following sympt oms < 3 Probable Parkinson’s disease years after PD onset: postural instability At least 3 of 4 feat ures in group A freezing present, no features in group B hallucinations for > 3 years, and sustained response to dementia dopaminergic therapy Supranuclear gaze palsy (other t han restriction of upgaze or slowed saccades) Definite Parkinson’s dise ase Severe dysautonomia All criteria met for Possible PD, plus Other condition known to cause histopathologic confirmation of parkinsonism diagnosis at autopsy Gelb et al. 1999, Archives Neurol Cardinal motor symptoms: Bradykinesia Cardinal motor symptoms: Gait Impairment 2
5/26/16 PD non-motor symptoms: Categories Motor symptoms are Just the tip of the iceberg… Psychiatric Autonomic Fatigue Orthostasis Depression Constipation Anxiety Urinary urgency Apathy ED Psychosis Sleep Cognitive RBD Executive dysfunction Impaired attention Poor sleep maintenance Impaired visuo-spatial Sensory function Loss of smell Relative preservation of anterograde memory Loss of taste Mild cognitive impairment Pain Dementia Barrone et al. 2009, Mov Disord Langston, 2006, Ann Neurol PD non-motor symptoms: Prevalence Cognitive deficits: Prevalence and clinical course PD-MCI: • Normal primarily nonamnestic single Most PD patients report an ↓ domain impairment average of 8 non-motor symptoms ~30% meet criteria for • Non-motor symptoms are often: PD-MCI within 3 years after PD-MCI more difficult to treat diagnosis ↓ impair quality of life more than motor symptoms ~50% meet criteria for • PD-MCI after 5 years PD Dementia (PDD) Barrone et al. 2009, Mov Disord Litvan et al., 2011, Mov Disord; Litvan et al., 2012, Mov Disord; Marraset al. 2013, Mov Disord 3
5/26/16 PD pathology: Parkinson’s disease: Clinical course substantia nigra pars compacta degeneration Stage 1: ~2 years Stage 3: ~2 years Unilateral involvement Mild to moderate bilateral involvement, Postural instability , Stage 2: ~7 years Mild bilateral Still independent involvement Stage 4: ~2 years Severe disability , Stage 5: ~2 years Needs an assistive device Wheelchair bound or bedridden to walk or stand Can only ambulate with another person assisting Zhao et al. 2010, Mov D isord Scarret al., 2013, Front. Cell. Neurosci.; Jenner 2002, Neurology PD pathology: Lewy body PD pathology: prion like disease 4
5/26/16 PD pathology: Braak Staging PD imaging: DaTSCAN DaTSCANs detect presnaptic dopaminergic § neuronal loss using SPECT imaging Measures Ioflupane ( 123 I), which is a DA T § ligand that binds to presynaptic dopamine transporters in the striatum de la Feunte-Fernandez 2012. Neurolog y Braak et al., 2004, Cell Tissue Research Piggott 1998; Fang and Martin, 2015, Parkinsonism and Related Disorders PD pathophysiology: Rate Model PD pathophysiology: Brain Arrhythmia The basal ganglia has two major intrinsic pathways: Phase amplitude coupling Increased bursting of neuronal activity Direct and Indirect Increased synchronization in neuronal activity • The direct pathway facilitates movement. Increased oscillatory • The indirect pathway inhibits movement activity • Striatal dopamine excites the direct pathway (increasing movement), and suppresses the indirect pathway (increasing movement) de Hemptinne et al. 2013, PNAS 5
5/26/16 PD etiology: Multifactorial PD Treatments: Role of exercise • Complex interplay between genetics (ingredients) • environment (recipe) • Oguh et al. 2014, Parkinsonism and Related Disorders Shu et al. 2014, PLOS T anner et al. 2011, Envi Health Perspectives Yang et al. 2014, PLOS Abbott et al. 2015, Neurology Sharp and Hewitt, 2014, Neurosci Biobehav Rev PD Treatment : Medications PD Treatments: Role of cognitive training Carbidopa/Levodopa: Mechanism of Action Paris et al. 2011, Movement Disorders Cannas et al. 2010, NeuropsychiatrDis T reat; Jenner, 2002, Neurology 6
5/26/16 PD Treatment : Medications PD Treatment : Medications Carbidopa/Levodopa: Carbidopa/Levodopa: Effects Formulations Sinemet IR The most effective and generally well-tolerated medicine for PD Parcopa Short half-life (~90 minutes), may need to be taken frequently as PD progresses Sinemet CR Should be taken 30-60 minutes before or after a protein-rich meal Main side effects: nausea, lightheadedness, hallucinations, and dyskinesias Rytary Cenci 2015, Frontiers in Neurology PD Treatment : Medications PD Treatment : Medications Carbidopa/Levodopa Extenders: Carbidopa/Levodopa Extenders: Mechanism of Action Effects 1 HOUR INCREASED ON-TIME Rasagaline (Azilect) • Rasagaline (Azilect) Side effects: drug interactions 1 HOUR INCREASED ON-TIME • Selegiline (Eldepryl) Selegiline (Eldepryl) Side effects: drug interactions, HTN, insomnia, delirium • Entacapone (Comtan) 1 HOUR INCREASED ON-TIME Entacapone (Comtan) Side effects: diarrhea, orange urine • Tolcapone (Tasmar) 2-3 HOURS INCREASED ON-TIME Tolcapone (Tasmar) Side effects: Liver failure Najib 2001, Clinical Therapeutics, Youdim 2006, Nature Rev Najib 2001, Clinical Therapeutics 7
5/26/16 PD Treatment : Medications PD Treatment : Medications Dopamine Agonist: Dopamine Agonist: Mechanism of Action Effects Compared to carbidopa/levodopa Lasts longer, half-life: ~6 hours Lower risk of causing dyskinesias • Pramipexole (Mirapex) More mild benefit • Ropinirole (Requip) Main side effects: sleep attacks, ICDs, sedation, confusion, hallucinations, cognitive deficits, dry mouth, lightheadedness • Rotigotine (Neupro) Usually not prescribed to people over 70 years of age Jenner, 2002, Neurology Jenner, 2002, Neurology PD Treatment : Motor Fluctuations PD Treatment: Motor Fluctuations & Dyskinesias OFF MEDICATIONS ON MEDICATIONS Cenci, 2014, Frontiers Neurology 8
5/26/16 PD Treatments: Dyskinesias PD Treatments: Risk of dyskinesias § The risk of dyskinesias is inversely proportional to the L-dopa dose Dose of Percentage developing dyskinesia after 1 year of L-dopa levodopa Placebo 3% 150 mg/day 3% 300 mg/day 2% 600 mg/day 15% § The risk of dyskinesias is inversely proportional to the age of PD onset Age of PD onset Percentage developing dyskinesia after 5 years of L-dopa 40-49 70% 50-59 42% 60-69 33% 70-79 24% Ku and Glass, 2010, Movement Disorders; PSG Study Group, NEJM, 2004 PD Treatment : Medications PD Treatments: Levodopa sparing therapy Levodopa sparing therapy: Dopamine agonists Zonisamide Effects Mild-moderate reduction in parkinsonism Dopamine agonists Side effects: ICD, sleep attacks, hallucinations, cognitive deficits Reduces tremor, mild benefit Trihexyphenidyl (Artane) MAO-B inhibitor Side effects: nephrolithiasis, somnolence, Zonisamide ataxia, confusion, cognitive deficits (Selegiline or Rasagaline) Amantadine Reduces tremor and dystonia T rihexyphenidyl Side effects: sedation, delirium, hallucinations, increased risk of dementia, dry mouth, constipation Najib 2001, Clinical Therapeutics 9
Recommend
More recommend