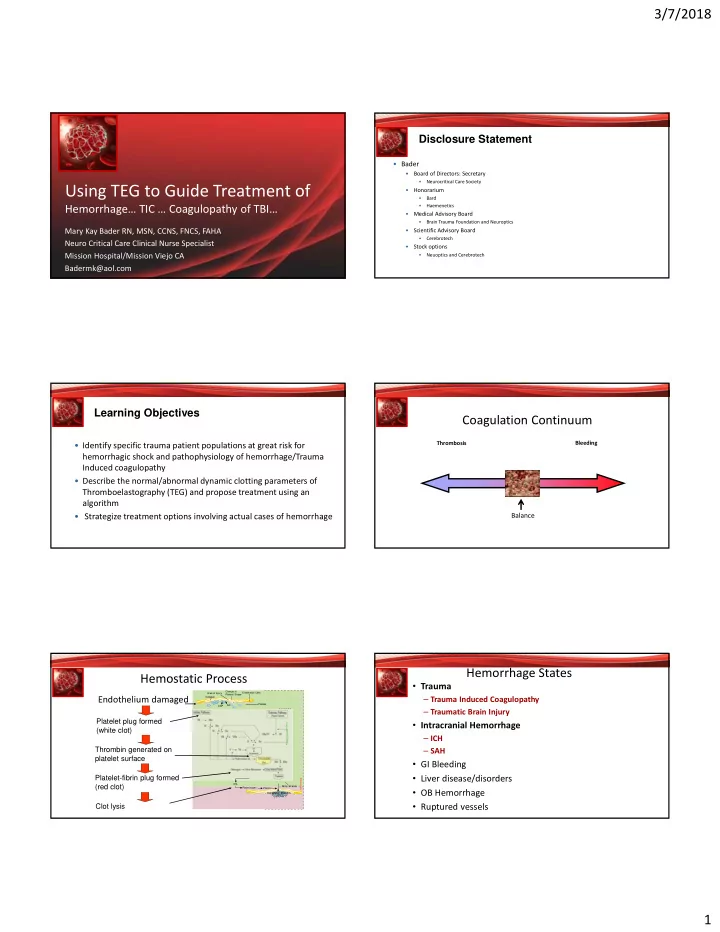
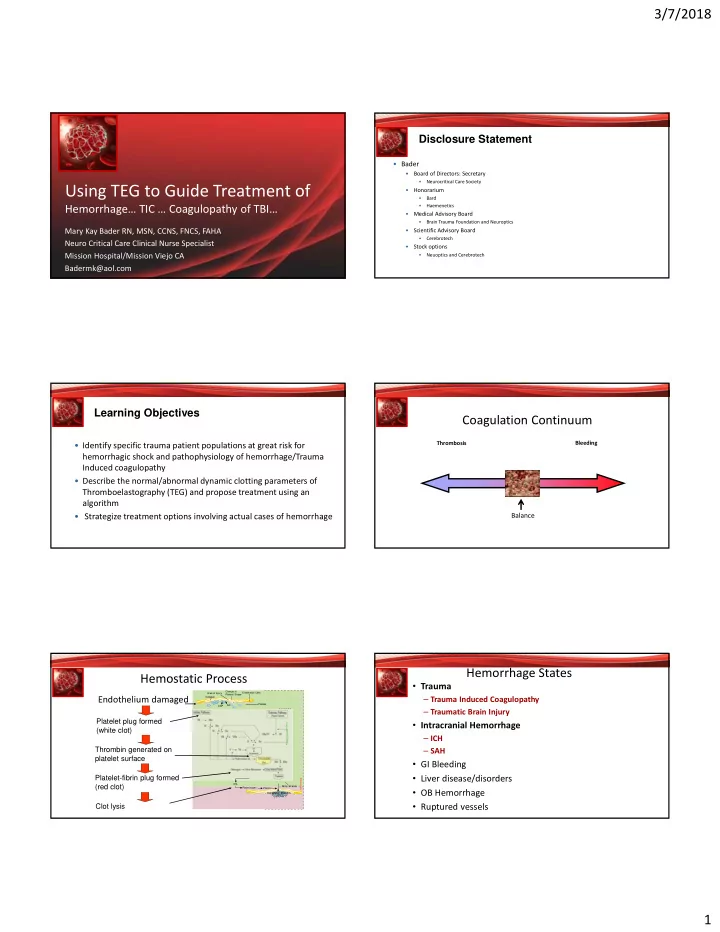
3/7/2018 Disclosure Statement • Bader • Board of Directors: Secretary • Neurocritical Care Society Using TEG to Guide Treatment of • Honorarium • Bard • Haemenetics Hemorrhage… TIC … Coagulopathy of TBI… • Medical Advisory Board • Brain Trauma Foundation and Neuroptics Mary Kay Bader RN, MSN, CCNS, FNCS, FAHA • Scientific Advisory Board • Cerebrotech Neuro Critical Care Clinical Nurse Specialist • Stock options Mission Hospital/Mission Viejo CA • Neuoptics and Cerebrotech Badermk@aol.com Learning Objectives Coagulation Continuum Thrombosis Bleeding • Identify specific trauma patient populations at great risk for hemorrhagic shock and pathophysiology of hemorrhage/Trauma Induced coagulopathy • Describe the normal/abnormal dynamic clotting parameters of Thromboelastography (TEG) and propose treatment using an algorithm • Strategize treatment options involving actual cases of hemorrhage Balance Hemorrhage States Hemostatic Process • Trauma Change in Endothelial Cells Area of Injury Platelet Shape Endothelium damaged Collagen – Trauma Induced Coagulopathy Platelet AA ADP – Traumatic Brain Injury XII XIIa Platelet plug formed • Intracranial Hemorrhage Coagulation Cascade XI XIa (white clot) IX VII a/TF VII – ICH X + Thrombin generated on – SAH Ca 2+ V V platelet surface • GI Bleeding Pr om bin (II) Thr XIII XIIIa Platelet-fibrin plug formed • Liver disease/disorders Fibrinolysis tPA (red clot) Fibrin Strands Plasminogen Plasmin • OB Hemorrhage Degradation Products Clot lysis • Ruptured vessels 1
3/7/2018 The Coagulopathy of Trauma Trauma Injury, Hemorrhage, & TBI Numerous Theories • Trauma/Injury is the 2 nd leading cause of death globally Hypoxia derived from hemorrhagic Intrinsic and – 40% of mortality associated with injury due to uncontrollable hemorrhage shock & tissue Acquired Factors that potentiate TIC injury are • 1/3 of severely injured trauma patients sustain Trauma Induced synergistic in driving TIC and coagulopathy (TIC) activation of protein C – Poorly understood mechanisms – Several theories • Coagulopathy of TBI (CTBI) is a component of TIC – Multiple theories contribute to early platelet dysfunction – Correlation between severity of TBI and platelet dysfunction Coagulopathy of TBI (CTBI) Coagulopathy of TBI (CTBI) • Multiple Factors – • Presence of CTBI ranges 10 ‐ 97% in ROL due to many factors Multiple Theories – TF release by the – Heterogeneity of patients, types of lab tests, timing of tests, and lack brain of clear defined consensus to define CTBI tissue/platelet degradation – Associated with poor outcomes – Disseminated – Blunt TBI: coagulopathy increases mortality (50% vs 17.3% ) intravascular coagulation (DIC) compared to no coagulopathy – Activation of – Factors increase risk include GCS<8, ISS>16, hypotension on admit, Protein C cerebral edema, SAH, shift – Hyperfibrinolysis Exhausted Platelet Dysfunction Coagulopathy of TBI (CTBI) • BBB disruption releasing TF (Castellino et al 2014) – Qualitatively different form that found in most tissues (unexposed to • Platelets & Platelet Activating Factor Theories soluble clotting factors –unsaturated by factor VII) – TBI may result in platelet hyperactivity – Liberation of free TF into circulation, provokes TF binding to VIIa on a – Platelet activating factor (PAF) induces massive scale aggregation and contributes to hypoxia ‐ induced • Results in stimulation of thrombin production in the initiation phase • Flood of TF –generated thrombin results in platelet exhaustive syndrome breakdown of the BBB • Large numbers of circulating platelets exist in a refractory state – Tissue Factor normally not exposed to circulating – Leads to Platelet inhibition at the ADP receptor site (Davis et al 2013) blood volume…in TBI brain tissue (rich in TF) & – Platelets incapable of stimulation and cannot form a stable thrombus through usual pathways platelets (breakdown) release TF in response to – Platelet count usually normal (Davis et al 2013) the injury and other cellular dynamics • No evidence of fibrinolysis (Davis et al 2013) 2
3/7/2018 Rats c TBI – TEGPM Platelet Dysfunction as an Early Marker for CTBI Human TBI 70 Pts TEGPM done Rats: ADP inhibition within 15 min Humans: ADP inhibition 93% in TBI Massive Transfusion Protocol • Fluid resuscitation – Crystalloid resuscitation done judiciously to avoid dilutional coagulopathy and tissue edema – 1:1:1 goal ratios for blood products • Normothermia Maintenance – Warmed fluids and Bair Hugger • Transfusion Related Medications – TXA – Calcium Chloride – Reversal agents for anticoagulant, antiplatelet therapy • Ongoing Assessment of Lab values – Point ‐ of ‐ care testing (Chem 8, PT/INR, Lactate) – ABG, CBC, PT/INR/PTT/FIB – TEG Endpoints of Resuscitation • – Ratio ‐ driven massive transfusion – Goal ‐ directed transfusion • TEG End Points of Resuscitation Measuring Hemostasis & TEG 3
3/7/2018 Measuring TIC and CTBI Assessing Coagulopathy after TBI Value of Viscoelastic Analysis • Viscoelastical Hemostatic Assays (VHAs) tests that reflect the new understanding of hemostasis – Initiation – Amplification –Propagation – TEG and ROTEM • VHAs assess properties of coagulation in whole blood – Can differentiate between low fibrinogen and reduced platelet function as the cause of impaired clot strength as well as systemic hyperfibrinolysis – Clinical value of VHA is corroborated by > 30 clinical studies on patients with massive hemorrhage— • Demonstrates Superiority over conventional coagulation tests Hemostasis Monitoring: TEG Technology: TEG Hemostasis System How It Works • Cup oscillates • Whole blood test • Pin is attached to a torsion • Measures hemostasis wire Clot initiation through clot lysis • Clot binds pin to cup Net effect of components • TEG system • Degree of pin movement is a function of clot kinetics Laboratory based • Magnitude of pin motion is a Point of care function of the mechanical Remote, can be networked properties of the clot Flexible to institution needs • System generates a hemostasis profile From initial formation to lysis Thrombin Formation (Clotting Time) Thrombin Formation Abnormalities The R Parameter: Identified • Reaction time The R Parameter: Elongated R • • Possible causes of The time from the start of the test, when the pin is imbalance: stationary, to the time of Slow enzymatic Initial fibrin initial fibrin formation, reaction formation when fibrin creates a • Possible etiologies: connection between the Factor deficiency/ surface of the cup and the surface of the pin, dysfunction • Residual heparin Expression of enzymatic reaction- Anticoagulants the ability to Intrinsic, Warfarin extrinsic, generate thrombin common Novel AC and fibrin pathways • Pin is • Pin is Common treatments: Normal range 5-10 stationary engaged Pin is Pin is minutes FFP stationary engaged Protamine Cup oscillates, Pin starts to pin remains oscillate with PCC stationary cup 4
3/7/2018 Fibrinogen Fibrinogen Abnormalities The α (Angle) Parameter: Low The α (Angle) Parameter: Identified A low angle suggests a slow rate of fibrin formation, which could lead to bleeding. • • Possible causes of imbalance : Fibrin Rate of increase in pin increases Slow rate of fibrin oscillation amplitude formation as fibrin is generated • Possible etiologies: and cross-links are Fibrin Low fibrinogen levels or formed increases function Conversion of Fibrinogen Insufficient rate/amount fibrin Baseline Baseline of thrombin generation Interactions among fibrinogen, fibrin, and Platelet platelets deficiency/dysfunction The faster the rate of fibrin • Pin is Common treatments: generation, the greater the engaged FFP increase in pin oscillation Pin is amplitude, and the larger Cryoprecipitate engaged the angle. The common treatments for a low angle depend on the cause and the degree of Normal α (Angle) is bleeding. An isolated low angle with normal R and MA values is indicative of low 53 ‐ 72 degrees fibrinogen levels, a condition commonly treated with FFP or cryoprecipitate. Fibrinogen Abnormalities Fibrinogen Abnormalities The α (Angle) Parameter: High The α (Angle) Parameter: Low alpha Angle Fibrin increases • Possible causes of imbalance: Fast rate of fibrin formation • Possible etiologies: Platelet Baseline hypercoagulability Fast rate of thrombin generation Pin is engaged Since a high angle is the result of an imbalance in other phases of the hemostatic Pt admit with cirrhosis of liver, liver failure, septic shock…. process, there is no specific common treatment for it. Possibilities for reducing the angle are anticoagulation and platelet inhibition. Platelet Function Fibrinogen Abnormalities • Maximum amplitude The MA Parameter: Defined • The α (Angle) Parameter: High Clot strength = 80% platelets + 20% Maximum amplitude (MA) of pin oscillation fibrinogen • Patient is • Binds plts together • the stronger the clot, given way the greater the to much amplitude of pin oscillation. Amplitude of fibrinogen • pin oscillation Platelet function in the OR influences thrombin generation and fibrin formation relationship between R, α , and MA Normal MA=50 ‐ 70 mm 5
Recommend
More recommend