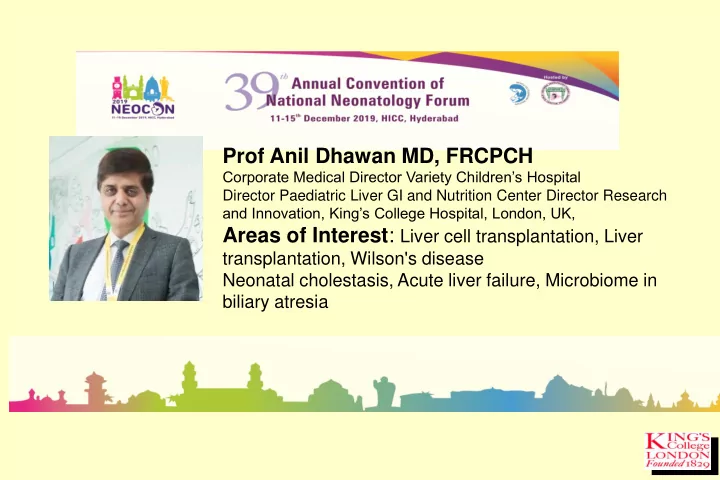
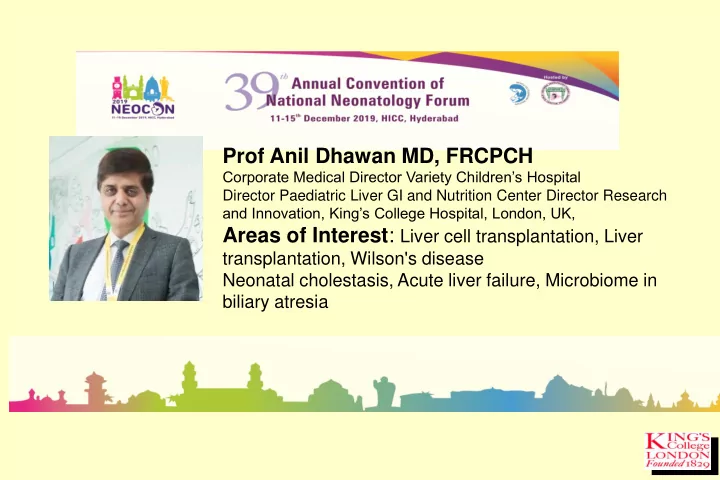
Prof Anil Dhawan MD, FRCPCH Corporate Medical Director Variety Children’s Hospital Director Paediatric Liver GI and Nutrition Center Director Research and Innovation, King’s College Hospital, London, UK, Areas of Interest : Liver cell transplantation, Liver transplantation, Wilson's disease Neonatal cholestasis, Acute liver failure, Microbiome in biliary atresia
Neonatal Cholestasis Case based discussions Profesor Anil Dhawan MD, FRCPCH Medical Director Paediatrics Director Pediatric Liver GI and Nutrition Centre Variety Children’s Hospital King’s College Hospital London
Neonatal Cholestasis ~ 1:2700 live births
Neonatal Hepatitis 1992-2005 N=1625 PFIC 5%
Diagnostic Dilemmas Exclude ALF as presentation (INR >2 unresponsive to Vit K) Exclude Biliary atresia Identify treatable conditions Recogonise and avoid complications Genetic /inherited conditions- PFIC syndromes
Charlie Born one week before term by Caesarian section because of maternal UTI No problems during pregnancy No immediate neonatal problems
At 6 days of age: refuses to feed irritable vomits floppy
GP Local Hospital AST 10150 IU/l Bilirubin 150 m mol/l (100 conjugated) GGT 56 IU/l Albumin 33 g/l Alkaline Phosphatase 313 IU/l Hb 11.9 g/l WBC 3.3x10 9 /l, Platelets 80x10 9 /l INR 2.3
Local Hospital D : sepsis/?meningitis + DIC Treated with antibiotics for 3 weeks No improvement
Liver failure ? cause King’s
Differential Diagnosis Galactosaemia Tyrosinaemia Neonatal Herpes Infection Neonatal Haemochromatosis Haemophagocytic Lymphohistiocytosis
Differential Diagnosis Galactosaemia ? Tyrosinaemia Neonatal Herpes Infection Neonatal Haemochromatosis Haemophagocytic Lymphohistiocytosis
Galactosaemia Commonly presents with sepsis Early treatment essential D : galactose 1 phosphate uridyl transferase in red cells
Differential Diagnosis Galactosaemia Tyrosinaemia ? Neonatal Herpes Infection Neonatal Haemochromatosis Haemophagocytic Lymphohistiocytosis
Tyrosinaemia Prolonged INR, but mildly elevated AST and no jaundice D : Succinyl acetone in urine Rx: NTBC, if no response, OLT
Differential Diagnosis Galactosaemia Tyrosinaemia Neonatal Herpes Infection ? Neonatal Haemochromatosis Haemophagocytic Lymphohistiocytosis
Neonatal Herpes Infection Presents during first week of life No skin lesions Maternal history can be negative Caesarian section not always protective Transaminases very high Early treatment with aciclovir essential
Differential Diagnosis Galactosaemia Tyrosinaemia Neonatal Herpes Infection Neonatal Haemochromatosis ? Haemophagocytic Lymphohistiocytosis
Neonatal Haemochromatosis Liver failure of neonatal presentation Abnormal LFTs, severe coagulopathy, high serum ferritin Hepatic and extra-hepatic non-RES iron deposition MRI shows extra-hepatic iron overload
Neonatal Haemochromatosis Treatment Anti-oxidant cocktail Liver transplant
Differential Diagnosis Galactosaemia Tyrosinaemia Neonatal Herpes Infection Neonatal Haemochromatosis Haemophagocytic Lymphohistiocytosis ?
Haemophagocytic lymphohistiocytosis (HLH) inherited acquired different entities?
HLH severe pancytopaenia & coagulopathy liver dysfunction high triglicerides low fibrinogen (with or without DIC) high uric acid haemophagocytosis (bone marrow, liver, spleen, CSF, ascites, skin, lymphonodes etc)
HLH steroids, i.t. metotrexate, i.v. immunoglobulin etoposide ( anti histiocytes ) anti thymocyte globulin/cyclosporin A ( anti T cells ) bone marrow transplant
HLH lethal without chemotherapy & bone marrow transplant
Diagnosis in Charlie Neonatal Herpes Infection No response to aciclovir (started too late?) Successful OLT at 6 weeks
Cholestasis case 1 Persisting Jaundice 6 weeks Pale stool Bilirubin 134/108,GGT 297 ALT102 INR 3.5 babies with biliary atresia look normal!!
Take home message Please check and correct INR with Vit K in all children with Cholestasis
Cholestasis Case 2 6 week old boy Referral for conjugated hyperbilirubinaemia & local US scan suggestive of biliary atresia Background: – Born at 36+1, SVD, BW 2.8kg, discharged home same day – Antenatal history: Anti-D during pregnancy for previous Rh incompatibility – Jaundice day 4 of life requiring 3 days of phototherapy Family history: – Parents are second cousins (born in Iraq, 5 years ago moved to UK) – 3 elder siblings – alive & well – No FHx of liver or blood disorders Persisting jaundice -> referred to prolonged jaundice clinic
Investigations at local hospital TFT, G6PD, CMV, FBC, urine MC&S – all normal Date Total Conj. bilirubi bilirubi US scan: abnormally n n 16/1 183 29 small shrunken thick- 31/1 125 38 3/2 110 48 walled GB with mild splenomegaly. Appearances suggestive of biliary atresia.
Review at KCH ( 6 weeks old) HPC: Growing well. Breastfed with formula top-ups. Weight 4.42kg (19 th centile) O/e: pale stools, soft 2cm liver & 2cm spleen palpable. Management: – Started on Vitamin K & E, & Abidec – Changed to Heparon Junior with BF top-ups
Bloods from initial review (6 weeks old) US scan – Hb 86 g/L Albumin 39 g/L – Liver parenchyma Retic. count 104 10^9/L Bilirubin 111 umol/L Platelets 196 10^9/L homogeneous Conj. Bili 42 umol/L LDH 349 IU/L ALP 597 IU/L – Normal gallbladder Haptoglobin <0.1 g/L AST 74 IU/L Potassium 5.8 mmol/L – No duct dilatation GGT 17 IU/L Urea 3.2 mmol/L ALT 113 IU/L Creatinine 15 umol/L – Normal vessels INR 1.17 Ratio TSH 4.4 mIU/L Lactate 1.9 mmol/L – Spleen is enlarged Free thyroxine 14.6 pmol/L Glucose 5.8 mmol/L O Rh positive DAT negative (length 7.6 cm) Cortisol 475 nmol/L G6PD normal
Liver biopsy Portal fibrosis Cholestasis, ductal bile plugs, but no ductular reaction Severe macrovesicular steatosis
Investigations (3m old) Bilirubin 144 umol/L A1AT PIM Conj. Bili 109 umol/L Gal-1-Put Normal ALT 1670 IU/L LAL-D Negative AST 1090 IU/L CDG Negative GGT 20 IU/L Urine organic acids Normal Albumin 39 g/L Plasma amino acids Normal INR 1.33 Very long chain fatty Normal acids Thyroid function Normal AFP 2171123 (kIU/L) Ferritin 4151 ug/L - Cholestasis gene panel - Urinary bile acids
Molecular genetics (4.5m): 12466 combined parents UBA_03-08-17_014 38 (4.256) Cm (4:70) 1: Parents of 85ES- 771 2.85e3 100 607 623 % 760 489 595 523 624 420 446 225 591 759 477 491 700 320 421 524 653 671 710 783 401 202 300 338348 564 379 279 236 791 0 m/z 200 250 300 350 400 450 500 550 600 650 700 750 800 UBA_03-08-17_014 38 (4.275) Cm (3:68) 2: Parents of 97ES- 725 3.26e3 100 511 250 511 511 527 658 % 565 481 415 657 658 423 445 561 600 736 265269297 384 619 659 531 714 337 379 620 311 697 786 779 234 0 m/z 200 250 300 350 400 450 500 550 600 650 700 750 800 UBA_03-08-17_014 29 (3.627) Cm (4:63) 3: Parents of 80ES- 494 6.58e3 100 494 494 495 % 495 265 511 213 297 325 362 311 479 511 476 218 235 423 430 713 384 539 562 585 623 645 696 702 777 0 m/z 200 250 300 350 400 450 500 550 600 650 700 750 800 UBA_03-08-17_014 29 (3.646) Cm (2:71) 4: Parents of 74ES- 445 2.96e3 100 444 205 682 444 % 460 626 443 465 408 466 510 442 230 565 733 552 616 344 711 373 378 511 645 651 259 282 313 761 0 m/z 200 250 300 350 400 450 500 550 600 650 700 750 800 UBA_03-08-17_013 99 (3.630) Cm (4:443) Scan ES- 494 6.81e4 100 285 285 495 % 213 510 449 285 286 511 255 583 329 247 342 759 365 392 476 607 623 527 423 657 700 577 225 745 0 m/z 200 250 300 350 400 450 500 550 600 650 700 750 800
Ward admission 5m old Admitted to local hospital - acute bronchiolitis Decompensated liver disease Admitted to commence on cholic acid & chenodeoxycolic acid Assessed for transplant - listed on 1/6
Liver transplant Living related transplant from mother (left lateral segment) on 13/6 Explanted liver: Very cholestatic, fine nodularity, irregular surface, large droplets of fat, looks inflammatory. GGT immunostain absent, others expressed appropriately.
Treatment Fatal without treatment Cholic acid (5-15mg/kg) Chenodeoxycolic acid Ursodeoxycolic acid Liver transplantation
Cholestasis 3 6 wks old persisting jaundice Pigmented stool USS – Normal Bili 176/140, AST350, ALT 401, GGT 29 Liver Biopsy – Giant cell Hepatitis Mutational analysis – BSEP def. Tx at 3 years , suspicious nodule HCC
Molecular genetics Biochemistry
Hepatocytes Canalicular Membrane Canaliculus Junctional complexes
Actin Claudin s TJPs FIC1 MDR3 AL PC BA OA MRP2 BSE P
Hepatocyte Canaliculus ABCG5/8 Mixed micelles Phosphatidylcholine MDR3 BSEP Bile acids Conjugated bilirubin MRP2 FIC1 Amino Phospholipids
NGS for cholestasis at King’s • 3 PFIC genes • 7 bile acid synthesis defects • 2 tight junction defects • Neonatal sclerosing cholangitis • ARC • Dubin Johnson • Citrin deficiency • FXR
Recommend
More recommend