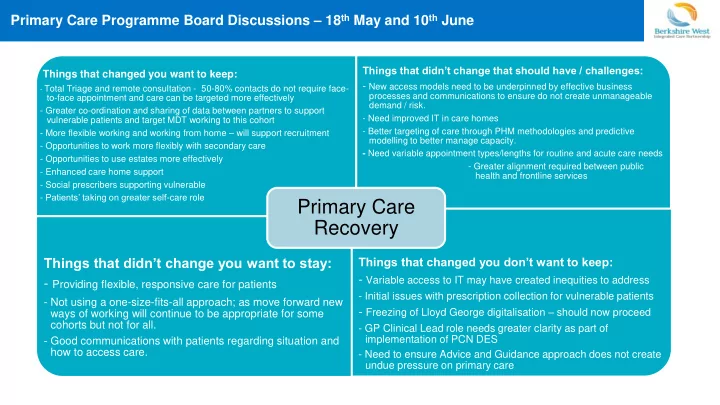
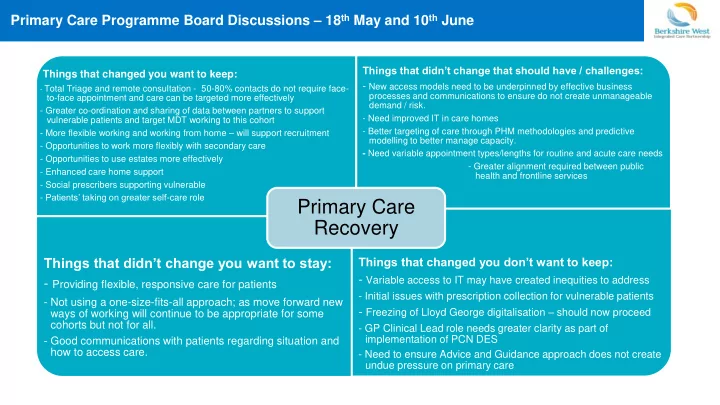
Primary Care Programme Board Discussions – 18 th May and 10 th June Things that didn’t change that should have / challenges: Things that changed you want to keep: - New access models need to be underpinned by effective business - Total Triage and remote consultation - 50-80% contacts do not require face- processes and communications to ensure do not create unmanageable to-face appointment and care can be targeted more effectively demand / risk. - Greater co-ordination and sharing of data between partners to support - Need improved IT in care homes vulnerable patients and target MDT working to this cohort - More flexible working and working from home – will support recruitment - Better targeting of care through PHM methodologies and predictive modelling to better manage capacity. - Opportunities to work more flexibly with secondary care - Need variable appointment types/lengths for routine and acute care needs - Opportunities to use estates more effectively - Greater alignment required between public - Enhanced care home support health and frontline services - Social prescribers supporting vulnerable - Patients’ taking on greater self -care role Primary Care Recovery Things that didn’t change you want to stay: Things that changed you don’t want to keep: - Variable access to IT may have created inequities to address - Providing flexible, responsive care for patients - Initial issues with prescription collection for vulnerable patients - Not using a one-size-fits-all approach; as move forward new - Freezing of Lloyd George digitalisation – should now proceed ways of working will continue to be appropriate for some cohorts but not for all. - GP Clinical Lead role needs greater clarity as part of implementation of PCN DES - Good communications with patients regarding situation and how to access care. - Need to ensure Advice and Guidance approach does not create undue pressure on primary care
Key changes to lock-in from practice survey (32 responses) Key changes to lock-in: Changes made: Total Triage >10 practices: Remote consultation • Total Triage Remote working by clinicians and teams • Remote consultation • Remote working >5 practices: • MS Teams meetings Other lock-in priorities: • EPS/Batch Prescribing Other changes: • Use of MS Teams for meetings • EPS usage • Split hot/cold working • Reduced bureaucracy • Working with hubs • Recruitment opportunities – reputational and increased flexibility • Reduced bureaucracy • Effective use of social prescribers • Virtual group clinics • Better use of estates • Redesign focus • Reduced focus on routine work and income 11 practices would not reverse any of the changes • Remote nursing home ward they have made however several noted importance of rounds now reinstating appropriate face-to-face care
Lock-in challenges from practice survey (32 responses) Challenges to sustaining change Potential CCG support: >10 practices: • Consistent supply of PPE • Changing patient expectations post-peak • Support patient communications • Social distancing / safely seeing patients / face coverings • Consider maintaining hub >5 practices: arrangements • Embedding new ways of working amongst clinicians • Clarify Nursing Homes clinical • Planning for increasing respiratory workload / need to see ‘hot’ patients in practice lead role as approach Winter - unknown Covid levels • • Share predictive modelling Flu • Addressing backlog in routine work / patient reluctance to attend around Covid-19 • Additional time required now to see patients face-to-face • Reinstate TIPs training • Effective selection of patients for face-to-face care, managing risk • Progress Lloyd George Other challenges: digitisation • Shielded/high risk staff and ‘Test and Trace’ • Reduce email traffic • Supporting staff working remotely, maintaining morale and avoiding burnout. • Maintain digital meetings Childcare remains a concern. • IT support / equipment • Continue to freeze QOF/ES • Training backlog/new training requirements returns • Time to focus on embedding change • Reduce email traffic • Backlog in PCN development/staffing • • Potential income shortfall IT equipment availability • Reinstatement of administrative tasks
Berkshire West Primary Care Recovery Pathway 1) Next phase operating model (key focus for next 3-4 months) • Core primary care delivery resumes with clear arrangements in place for managing increased prevalence of respiratory illness which may make it difficult to differentiate Covid and non-Covid presentations / potential increased complexity. Work with respiratory consultants and clinical leads to define ongoing role of both hubs and practices. • Practices operating with social distancing and clear business continuity arrangements in place. QOF/CES asks defined. • Predictive modelling used to determine capacity and assess escalation triggers (pilot work with Oxford University) • Escalation plan remains in place including ability to go live with home visiting service and expand hub capacity if required • Enhanced care home support remains in place – implementation of PCN DES requirements and further define clinical lead role • Full roll out of Advanced Advice and Guidance • Successful delivery of flu campaign 2) Lock in change • Time for Care/other training to embed business processes to underpin use of new technologies • Work with AHSN and Healthwatch to develop best practice model for video consultations and patient engagement strategy covering Total Triage and remote consultation • Greater use of GP Connect to support new pathways and collaborative working within PCNs • EPS 4 implementation • Further provision of IT equipment – laptops and care home IT infrastructure • Further embed PHM risk stratification approach to underpin partnership working to identify and support vulnerable patients • Social prescribers and others to continue to support self-care / patient activation 3) Drive further transformation • PCN OD work and ARRS recruitment back on track building on new ways of working. Implementation of all DES service specifications. • MDT care planning as core element of delivery – shared multi-morbidity care plan in place • Estates Strategy refreshed to reflect new ways of working / PCN models of care • Closer working with secondary care as part of outpatient transformation, improved referral practice
Recommend
More recommend