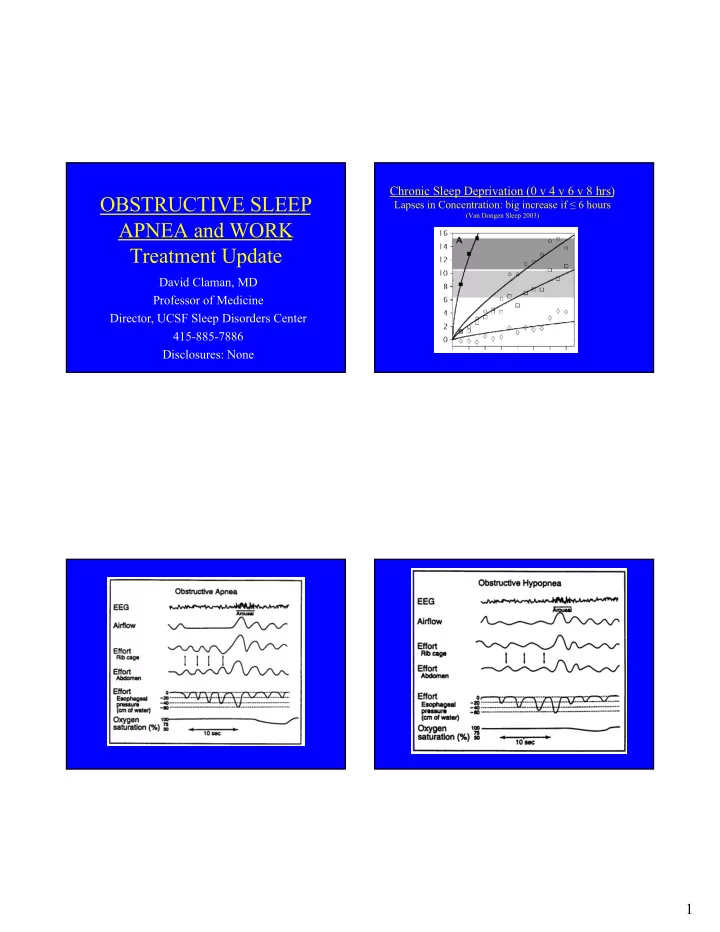
Chronic Sleep Deprivation (0 v 4 v 6 v 8 hrs) OBSTRUCTIVE SLEEP Lapses in Concentration: big increase if ≤ 6 hours (Van Dongen Sleep 2003) APNEA and WORK Treatment Update David Claman, MD Professor of Medicine Director, UCSF Sleep Disorders Center 415-885-7886 Disclosures: None 1
DEFINITIONS: CLINICAL PREDICTORS OF OSA u Apnea: complete cessation of airflow lasting 10 second or more • Screening questionnaires u Hypopnea: reduced airflow for 10 seconds or more, • Epworth Sleepiness Scale: range 0-24 for 8 questions associated with 4% oxygen desaturation – Normal score < 10 u 3% is AASM recommendation; 4% is Medicare definition – In OSA population, score correlates with AHI u Apnea-hypopnea Index (AHI): average number of apneas & – SLEEP 1991; 14(6):540-5 • Berlin 10 questions validated in primary care hypopneas per hour of sleep – Snoring, apnea, fatigue, sleepiness at wheel, Hypertension AHI < 5 is normal ● – Ann Intern Med. 1999 Oct 5;131(7):485-91 AHI 5-14 - Mild OSA ● • STOP-BANG used in Anesthesia AHI 15-29 - Moderate OSA ● – Snoring, Tired, Observed apnea, Pressure (HTN), BMI 35, Age 50, AHI >= 30 - Severe OSA ● Neck circumference 40 cm (15.75 inches), Gender (male) Wisconsin Sleep Cohort: prevalence of 2% women and 4% in men based on ● – Arch Otolaryngol Head Neck Surg. 2010 Oct: 136(10):1020-4 AHI > 5 and symptoms of daytime sleepiness; NEJM 1993; 328(17):1230-5. CLINICAL PREDICTORS OF EPWORTH SLEEPINESS SCALE https://www.slhn.org/docs/pdf/neuro-epworthsleepscale.pdf OSA Score < 10 is normal; 10-15 is situational sleepiness; 15 > excessive http://www.stopbang.ca/osa/screening.php • STOPBANG – 8 Questions • High risk: yes to 5-8 questions; Medium risk yes on 3-4;Low risk yes on 0-2 • Snoring • Tired (fatigue) • Observed Apnea • Pressure (Hypertension) • BMI >35 ( ≥ 30 is considered obese) • Age >50 • Neck size > 17 inches for men or >16 inches for women • Gender male 2
PREVALENCE OF SLEEP APNEA COMPARISON OF QUESTIONNAIRES GE Silva et al. J Clin Sleep Med. 2011; 7(5): 467–472 u 602 working subjects, age 30-60, studied by overnight polysomnography u Obstructive sleep apnea defined as both AHI > 5 and hypersomnolence u 9% of women had AHI >5; 22% c/o hypersomnolence; yields 2% prevalence u 24% of men had AHI >5; 15% c/o hypersomnolence; yields 4% prevalence T Young; NEJM 1993;328:1230-5 CPAP as Secondary Prevention of Cumulative Percentage of Cardiovascular Events in OSA New Fatal (A) & non-Fatal (B) • Randomized trial CPAP v usual care; n=2717 Cardiovascular Events • Age 61; 80% men; AHI 29; BMI 28 JM Marin et al. Lancet. 2005 Mar • Pre -existing CAD or cerebrovascular disease 16;365(9464):1046-53 • Mean f/u 3.7 years; CPAP use 3.3 hrs KEY POINTS: • No change in primary cardiovascular outcomes 1. Increased mortality seen if AHI>30 • CPAP did improve quality of life measures – McEvoy RD et al. NEJM 2016;375:919 -931 2. CPAP reduced this risk 3
OSA TREATMENT CPAP to Prevent Cardiovascular Events u Weight loss (10% weight loss reduces AHI 25%) u Avoid alcohol for 3+ hour before bed u Postural training (side sleeping since apnea worse on back) u Nasal patency (treat allergies) u CPAP (including autoCPAP; Bi-level less common) u Oral (dental) appliances u ENT surgery: u Tonsillectomy in kids u UPPP in adults <50% success u Hypoglossal nerve stimulator now FDA approved u Nasal expiratory resistor (Provent) u Nasal adhesive micro-valve resistor – delivers approx 5 cm pressure • McEvoy RD et al. NEJM 2016;375:919-931 WHY TREAT SLEEP APNEA? MANDIBULAR ADVANCEMENT DEVICES Advancement of mandible Enlarge airway behind tongue, but may also enlarge airway behind palate • Improve patient’s daytime alertness (big motivator!) • Reduce cardio- vascular risk – Still debated • Improve partner’s sleep 4
ORAL APPLIANCE THERAPY: WHEN TO USE ORAL APPLIANCES? ANTERIOR MANDIBULAR • Mild to moderate OSA (AHI <30) REPOSITIONING • Intolerant of CPAP • After failed UPPP • Significant overbite • Must have teeth! • Relative contraindications: – Severe OSA with severe oxygen desaturation – TMJ symptoms Ferguson;Chest 1996;109:1269-75 CPAP: Nasal Mask or Pillows CPAP – Site Non-specific 5
LONGTERM USE OF CPAP SURGICAL THERAPY Best compliance if AHI >30 & ESS >10 (primarily if non-compliant with CPAP) Nasal Surgery • Tonsillectomy: if 3-4++, can be 80-90% success • (common approach in kids) Uvulopalatopharyngoplasty (UPPP) reduces AHI by • 50% in 40-50% of patients • For snoring: laser or radiofrequency Mandibular advancement • – Genioglossus advancement with hyoid – Mandibular-maxillary osteotomy & advancement Hypoglossal Nerve Stimulator • Tracheotomy remains gold standard • McArdle N et al. AJRCCM 1999;159:1108-1114 Question 2 Question 1 • Which of the following is NOT part of • Based on sleep deprivation data, when do STOPBANG? shorter sleep hours cause more symptoms? – A. BMI • A. ≤ 8 hours – B. Alcohol • B. ≤ 7 hours – C. Hypertension • C. ≤ 6 hours • D. ≤ 4 hours – D. Observed apnea 6
Recommend
More recommend