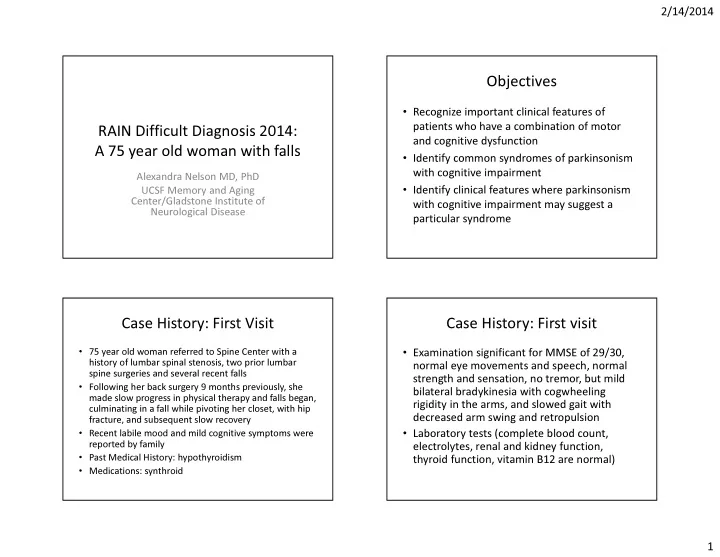
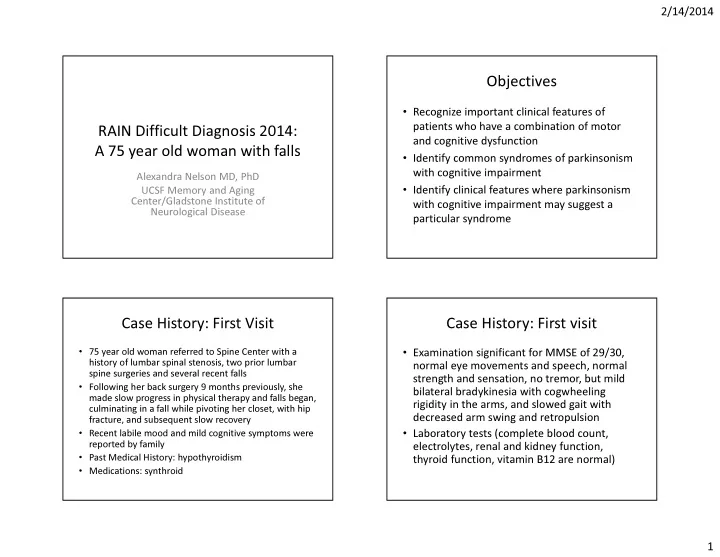
2/14/2014 Objectives • Recognize important clinical features of patients who have a combination of motor RAIN Difficult Diagnosis 2014: and cognitive dysfunction A 75 year old woman with falls • Identify common syndromes of parkinsonism with cognitive impairment Alexandra Nelson MD, PhD • Identify clinical features where parkinsonism UCSF Memory and Aging Center/Gladstone Institute of with cognitive impairment may suggest a Neurological Disease particular syndrome Case History: First Visit Case History: First visit • 75 year old woman referred to Spine Center with a • Examination significant for MMSE of 29/30, history of lumbar spinal stenosis, two prior lumbar normal eye movements and speech, normal spine surgeries and several recent falls strength and sensation, no tremor, but mild • Following her back surgery 9 months previously, she bilateral bradykinesia with cogwheeling made slow progress in physical therapy and falls began, rigidity in the arms, and slowed gait with culminating in a fall while pivoting her closet, with hip decreased arm swing and retropulsion fracture, and subsequent slow recovery • Recent labile mood and mild cognitive symptoms were • Laboratory tests (complete blood count, reported by family electrolytes, renal and kidney function, • Past Medical History: hypothyroidism thyroid function, vitamin B12 are normal) • Medications: synthroid 1
2/14/2014 Question 1: Which of the Following Imaging Diagnoses is Most Likely? 59% 1. Idiopathic Parkinson’s Disease 2. Complications of Spine Surgery 3. Progressive Supranuclear Palsy 22% 20% 4. Frontotemporal Dementia 5. Multiple Sclerosis 0% 0% . . . . . . . . . . . . . . u . r r s a l a n S e P r l o o c e c i p S t v h i a i m e s t c s l e p a i e p p l t t i r o o m g u l o t i n M d o r o I C P r F Imaging Parkinsonism + Cognitive Impairment • Parkinson’s Disease • Lewy Body Dementia • Progressive Supranuclear Palsy • Corticobasal Degeneration • Multiple System Atrophy • Vascular Disease • Frontotemporal Dementia – Parkinsonism • Alzheimer’s Disease +/- PD 2
2/14/2014 Case History: Second Visit Family History • Additional history obtained from family, including progressive gait disorder for 2-3 years, bulbar 89 progressive cognitive symptoms (disorganization, word finding problems), longstanding “sharp 90 65 56 80 tongue” but increased argumentativeness, irritability, obsessive criticism of family members • Motor impairment did not respond to levodopa 60 49 75 • Family history of ALS Motor Neuron Disease Cognitive/Behavioral Symptoms Question 2: Which of the Following Cognitive Evaluation Studies Would You Choose Next? • MMSE 27/30 66% • Verbal learning and memory: impaired but 1. Lumbar Puncture improved with cueing (CVLT 9 item) 2. PET Brain Imaging • Visuospatial memory: impaired (Figure drawing OK, but poor recall 3. Genetic Testing • Frontal/Executive: Working memory WNL. Set 21% 4. EMG switching/sequencing severely impaired 11% (Modified Trails Test) 2% • Language: Reading WNL. Phonemic and category verbal fluency impaired . . G . . . . . . M . g n r u a i E m t t s c e n I T u n P i c a i t r B r e a n b T e m E G P u L 3
2/14/2014 Behavioral Variant Frontotemporal FTD with Parkinsonism Dementia • Behavioral phenotype: loss of social graces, • Relatively common feature of FTD compulsive behaviors (eating, hoarding), • Akinetic-rigid subtype predominant irritability • Can manifest as corticobasal syndrome • Cognitive phenotype: frontal/executive (loss of ability to multitask, plan; poor processing speed, • Variable severity sequencing, verbal fluency) • Other FTD clinical phenotypes include aphasias (progressive nonfluent aphasia, semantic dementia), corticobasal syndrome, FTD-ALS • Can include parkinsonism in a subset of cases Genetic Correlates of bvFTD and/or Genetic Testing ALS • GRN (progranulin) – uncommon ALS • About 10 years previous, patient had participated in ALS research and none of the • MAPT ALS-related genes known at that time were • CHMP2B identified in her sample • FUS – rarely FTD • EMG had also been performed on 2 prior • C9ORF72 – FTD, ALS, and FTD-ALS occasions and was normal • SOD1 – uncommon FTD • Genetic Testing for C9ORF72 hexanucleotide • TARDBP – uncommon FTD expansion was positive 4
2/14/2014 C9ORF72 C9ORF72 Hexanucleotide Expansion • ALS: about 10% overall of cases have family • Originally identified in families with ALS history; of these large portion are associated and/or FTD with C9ORF72, though also TARDBP, FUS, • Non-coding region, hexanucleotide repeat SOD1 (>30 deemed pathologic) • ALS clinical spectrum in C9 similar to ALS • Autosomal dominant inheritance but may not overall, though more often other neurological be 100% penetrance, and variety of symptoms present (dementia, parkinsonism) phenotypes, even in the same family • NOT a common cause of idiopathic PD (3/1446 patients in one large study) C9ORF72 Hexanucleotide Expansion FTD with C9ORF72 • FTD: Patients have family history in approaching half of cases, but about 10-15% have clear autosomal dominant inheritance • Many familial FTD caused by C9ORF72; other genes include MAPT, GRN, CHMP2B, TARDBP, VCP, FUS • 3-4% of sporadic cases of FTD also associated with C9 • C9/FTD clinical features similar to FTD overall, but favors FTD-ALS, bvFTD, more commonly presenting with psychosis, rarely language • C9 Carriers can also have pure psychiatric disease Devenney et al, 2014 5
2/14/2014 FTD with C9ORF72 FTD with C9ORF72 Boeve et al, 2012 Boeve et al, 2012 bvFTD with C9ORF72 bvFTD - parkinsonism with C9ORF72 Akinetic/rigid, no rest tremor, none levodopa-responsive Boeve et al, 2012 Boeve et al, 2012 Also Sha et al, 2012 6
2/14/2014 Cognitive Features Imaging Features Impaired timed frontal/executive tasks • Heterogeneous; similar to FTD overall Preserved reading • Tends to be symmetric • Thalamic and cerebellar atrophy noted (connections to frontal cortex?) • Cortical and subcortical atrophy, ALS with C9>ALS without C9 • Dorsolateral PFC, insula common locations Boeve et al, 2012 Mahoney et al, 2012; Sha et al, 2012 Conclusions Pathological Features in SNc C9ORF72 Negative Case C9ORF72 Positive Case • Progressive parkinsonism + cognitive impairment can be caused by several atypical parkinsonian disorders, and this should also include FTD variants • Behavioral variant FTD, ALS, and FTD-ALS can are commonly accompanied by parkinsonism • C9ORF72 is the most common cause of inherited FTD, ALS, and FTD-ALS P62/ubiquitin cytoplasmic inclusions Cooper-Knock et al, 2013 Also Boeve et al, 2012 7
2/14/2014 Conclusions Acknowledgements • C9ORF72 is inherited in an autosomal dominant • Maggie Waung (UCSF Neurology) fashion, but can be present in sporadic cases • John Engstrom (UCSF Neurology) • C9ORF72 positive cases have typical onset in the • Jamie Fong (UCSF Memory and Aging Center, 50s, survival 5-10 years Genetic Counselor) • C9ORF72 clinical features: often psychosis (delusions), often parkinsonism; rare primary • Cindy Barton (UCSF Memory and Aging language variants Center, Geriatric Nurse Practitioner) • C9ORF72 has TDP-43 neuropathology, and includes substantia nigra pathology in both parkinsonian and nonparkinsonian cases 8
Recommend
More recommend