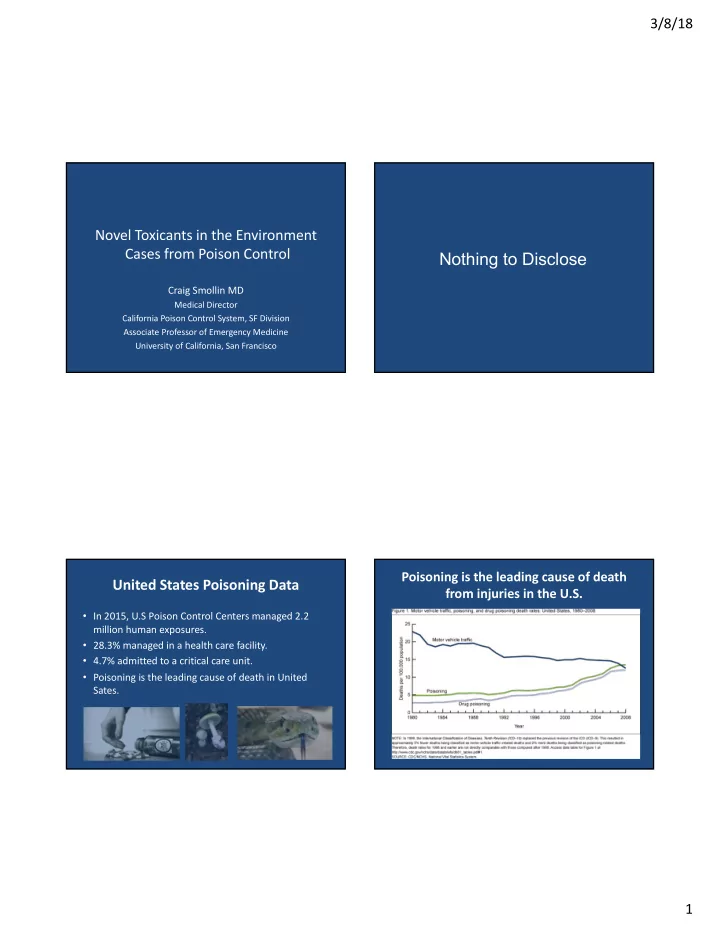
3/8/18 Novel Toxicants in the Environment Cases from Poison Control Nothing to Disclose Craig Smollin MD Medical Director California Poison Control System, SF Division Associate Professor of Emergency Medicine University of California, San Francisco Poisoning is the leading cause of death United States Poisoning Data from injuries in the U.S. • In 2015, U.S Poison Control Centers managed 2.2 million human exposures. • 28.3% managed in a health care facility. • 4.7% admitted to a critical care unit. • Poisoning is the leading cause of death in United Sates. 1
3/8/18 The California Poison Control System (CPCS) 55 Poison Control Centers The California Poison Control System (CPCS) • California Population ~40 million • Poison Control System Sacramento • Four Divisions • ~ 250,000 human exposures/year San Francisco Fresno San Diego 2
3/8/18 Case #1 – Leg pain and rash • A previously healthy 5 year-old male presents with intermittent bilateral lower extremity pain. • Pain wakes him from sleep and improves with massage. • Seen in clinic and diagnosed with “growing pains” Case #1 – Leg pain and rash Case #1 – Leg pain and rash • Pain worsens: • Pertinent Exam findings – Continuous “pins and needles” – Blood pressure 150/100 mmHg – Prefers to sit with knees drawn to chest – Mild diaphoresis – Associated with intermittent profuse sweating – Stomatitis – Rash on bilateral hands 3
3/8/18 Desquamation Erythema Stomatitis 4
3/8/18 Case #1 – Leg pain and rash Pink’s Disease • Laboratory tests: • Characteristics: – CBC, electrolytes, glucose, renal function normal – Pink palms and soles +/- desquamation – Urinalysis + protein – Red cheeks and nose – Serum catecholamines: – Loss of hair, teeth and nails • Norepinephrine 598 umol/mol (nl 0-80) – Salivation and marked diaphoresis • Epinephrine 61 umol/mol (nl 0-35) – Transient rashes • Dopamine 1041 umol/mol (nl 0-1130) – Painful extremities – Neuropsychiatric symptoms Case #1 – Leg pain and rash • Laboratory tests: – Spot urine mercury 26.7 mcg/L (nl <10 mcg/L) – 24 hour urine mercury 512 mcg/L (nl <50 mcg/L) 5
3/8/18 6
3/8/18 Case #2 Deadly Pesticide Case #2 Deadly Pesticide • A family of ten used an unknown pesticide • The father attempted to wash away the under their mobile home. pellets using a water hose. • Family members complained of an odor. • The following morning, 911 was called due to multiple family members will dyspnea and • Four days later, family members complained depressed level of consciousness. of abdominal pain and vomiting. • No carbon monoxide detected. • Seen in an Emergency Department and discharged with the “flu”. • One child in cardiac arrest. Multiple family members required transport to the hospital. 7
3/8/18 Aluminum Phosphide • AlP + 3 H 2 O à Al(OH) 3 + PH 3 (Phosphine gas) • Phosphine Gas: – Garlic or fishy odor – Highly toxic (lungs, brain, kidneys, heart, liver) – ACGIH TLVTWA = 0.3 ppm (0.42 mg/m 3 ) – IDLH = 50 ppm 8
3/8/18 Aluminum Phosphide Pesticides • Clinical Presentation: • Commonly reported to poison control centers. • Exposures occur through production, transportation – Cough dyspnea, headache, dizziness and vomiting and application. – ARDS • California with largest number of individuals – Acute renal failure employed in occupations using pesticides. – Hepatitis • Most commonly reported classes: – Seizures and coma – insecticides, herbicides, repellants, fumigants, fungicides. – Myocardial manifestations • Most common routes: – Inhaled and dermal. Case #3 An Unusual Opioid Case #3 An Unusual Opioid • A 36 year-old male brought to the emergency • 1.5 hrs later the patient developed recurrent department by EMS after ingesting symptoms with respiratory depression, and a hydrocodone/acetaminophen. decline in oxygen saturation to 90%. • Obtunded (grumbles/withdraws to pain). • Sxs improved after repeat dose of 6 mg naloxone. • Pin point pupils. • Respiratory rate is 8/min. • Improved after 2 mg of naloxone. 9
3/8/18 Onset, Duration of Effect, and Potency of Case #3 An Unusual Opioid Selected Opioids • 1.5 hrs later the patient developed recurrent Opioid Analgesic Onset of effect Duration of Potency (route) (min) effect (hrs) symptoms with respiratory depression, and a Morphine (IV) 5-10 3-6 1 decline in oxygen saturation to 90%. Oxycodone (PO) 10-15 4-6 0.5 Hydrocodone (PO) 30-60 4-6 0.33 • Sxs improved after repeat dose of 6 mg Hydromorphone (IV) 15 4-6 6.66 naloxone. Methadone (PO) 30-60 6-12 1 Fentanyl (IV) Immediate 0.5- 1 100 Buprenorphine (PO) 60 4-12 ? Meperidine (IV) 1-5 2-4 0.1 Naloxone (IV) 1-2 1-2 Case #3 An Unusual Opioid High Naloxone Requirements • Higher potency opioids may require larger • 1.5 hrs later the patient developed recurrent doses of naloxone symptoms with respiratory depression, and a decline in oxygen saturation to 90%. – Poklis A. Fentanyl: a review for clinical and analytical toxicologists. J Toxicol Clin Toxicol. 1995;33(5):439-47. • Sxs improved after repeat dose of 6 mg – Schumann H, Erickson T, Thompson TM, Zautcke JL, Denton JS. Fentanyl epidemic in Chicago, Illinois and surrounding Cook County. Clin Toxicol naloxone. (Phila). 2008;46(6):501-6. • Urine toxicology screen negative. 10
3/8/18 Urine Drug Screening: Opiates Case #3 An Unusual Opioid USUALLY NOT DETECTED USUALLY DETECTED • 1.5 hrs later the patient developed recurrent • Oxycodone 2 • Morphine symptoms with respiratory depression, and a • Methadone 2 • Heroin decline in oxygen saturation to 90%. • Fentanyl • Codeine • Sxs improved after repeat dose of 6 mg • Meperidine • Hydrocodone 1 • Buprenorphine 2 naloxone. • Hydromorphone 1 • Tramadol • Urine toxicology screen negative. • Acetaminophen level negative. 2 Specific assays available 1 Depending on the assay Laboratory Analysis: Fentanyl 3.5 mg Promethazine 2.3 mg Acetaminophen 39.2 mg 11
3/8/18 Novel Psychoactive Substances and Opioids What PPE for First Responders? • W18 • Furanylfentanyl • Acetylfentanyl • MT-45 • 3-methylfentanyl (TMF) • 4-methoxybutyrofentanyl What PPE for First Responders? What PPE for First Responders? 12
3/8/18 ACMT Position Statement on Workplace Exposure to Fentanyl • Risk of significant exposures to emergency responders is extremely low. • Incidental dermal contact unlikely to cause toxicity. • Nitrile gloves for routine handling. • In exceptional circumstances where there are drug particles or droplets suspended in air use N95 respirator • Worker should be trained to recognize opioid intoxication and to administer naloxone. Case #4 Feeling blue Case #4 Feeling blue • 57 year-old Chinese woman presents to the ED after • Physical Exam: eating previously frozen oven-cooked mudfish. – Dusky appearing skin without respiratory distress • She complains of headache, lightheadedness, – Vital Signs: P 84, RR 21, BP 120/80, O2 sat 85% shortness of breath and paresthesias of her – Lungs are clear bilateral extremities. • Husband ate same fish and had dizziness which resolved. 13
3/8/18 Case #4 Feeling blue Case #4 Feeling blue • Physical Exam: – Dusky appearing skin without respiratory distress – Vital Signs: P 84, RR 21, BP 120/80, O2 sat 85% – Lungs are clear bilateral • Placed on a non-rebreather oxygen mask – ABG: 7.41, pCO2 43, pO2 452, O2 sat 100% – CXR unremarkable Case #4 Feeling blue Case #4 • Physical Exam: • Treated with IV methylene blue (1 mg/kg) – Dusky appearing skin without respiratory distress • Skin discoloration and tachypnea improved within 1 hour. – Vital Signs: P 84, RR 21, BP 120/80, O2 sat 85% – Lungs are clear bilateral • Repeat MetHb level 1.3% at 3 hours. • Placed on a non-rebreather oxygen mask • Department of Public Health notified and – ABG: 7.41, pCO2 43, pO2 452, O2 sat 100% investigation revealed that frozen dried – CXR unremarkable mudfish imported from Thailand had high – MetHb level 40.2% levels of sodium nitrite. 14
3/8/18 Methemaglobinemia • Fe in Hgb oxidized Fe2+ à Fe 3+ • Reduced oxygen carrying capacity • Treatment – Methylene blue 1% – 1-2 mg/kg over 5 minutes – Symptoms generally improve over 1 hour – General rule treat when Methgb level > 20% Selected Drugs and Toxins Causing Methgb Amyl Nitrite “Poppers” Drugs Toxins Local anesthetics Aniline Dyes Chloroquin Benzene derivative Dapsone Paraquat Nitrites Phenazopyridine Primaquin Sulfamethoxazole 15
3/8/18 Poison Control System Summary 24/7 Hotline • The Poison Control System is an important public 1-800-222-1222 - Public health resource. • Involved in cases of significance to occupation and 1-800-411-8080 - Hospitals environmental health. • Case #1 à Mercury Exposure • Case #2 à Aluminum Phosphide Exposure Immediate consultation by • Case #3 à Fentanyl as an adulterant clinical pharmacists • Case #4 à MetHgb from nitrite exposure Back-up by MD toxicologists 16
Recommend
More recommend