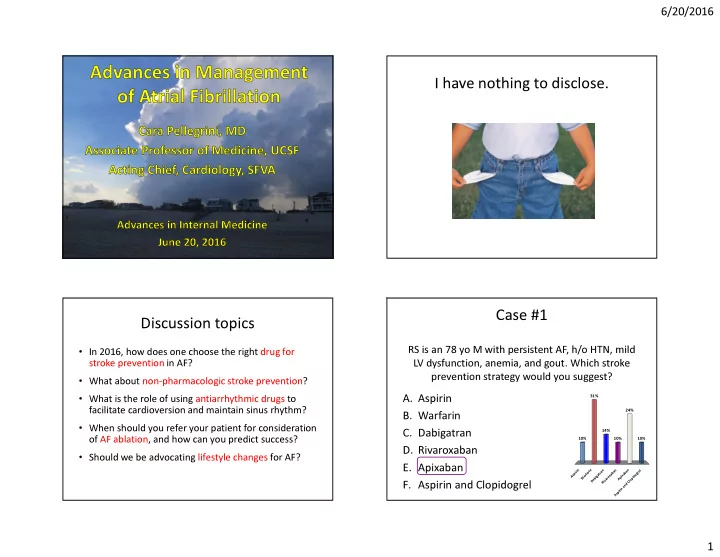
6/20/2016 I have nothing to disclose. Cara N. Pellegrini, MD Nothing to disclose Case #1 Discussion topics RS is an 78 yo M with persistent AF, h/o HTN, mild • In 2016, how does one choose the right drug for stroke prevention in AF? LV dysfunction, anemia, and gout. Which stroke prevention strategy would you suggest? • What about non-pharmacologic stroke prevention? 31% • What is the role of using antiarrhythmic drugs to A. Aspirin facilitate cardioversion and maintain sinus rhythm? 24% B. Warfarin • When should you refer your patient for consideration 14% C. Dabigatran of AF ablation, and how can you predict success? 10% 10% 10% D. Rivaroxaban • Should we be advocating lifestyle changes for AF? E. Apixaban Aspirin Warfarin Dabigatran Rivaroxaban Aspirin and Clopidogrel Apixaban F. Aspirin and Clopidogrel 1
6/20/2016 Annual Risk of Stroke or Systemic Embolism CHA 2 DS 2 -VASc Score 10-year follow-up rates among 73,538 of “real world” patients in Risk factor Score the Danish National Patient Congestive heart failure / LV dysfunction 1 Registry who have nonvalvular AF Hypertension 1 and were not treated with warfarin. Age ≥ 75 2 Diabetes mellitus 1 Stroke / TIA / thrombo-embolism 2 Vascular disease 1 Age 65-74 1 Female 1 CHA 2 DS 2 -VASc Score 4 Olesen JB and colleagues, BMJ 2011 Annual Risk (%/yr) of Major Bleeding HAS-BLED Score Major bleeding: bleeding requiring hospitaliza�on, causing ↓ hemoglobin > 2 g/L, Risk factor Score requiring transfusion. Uncontrolled hypertension 1 Significant renal dysfunction 1 Significant liver disease 1 Previous stroke 1 History of / predisposition to bleeding 1 Labile INRs 1 Age > 65 1 Antiplatelet / NSAID use 1 ≥ 8 alcoholic drinks / week 1 HAS-BLED Score 2 Olesen JB and colleagues, BMJ 2011 2
6/20/2016 Relative Risk of Stroke or Systemic Embolism Relative Risk of Major Bleeding Associated with Associated with Oral Anticoagulants and Oral Anticoagulants and Antiplatelet Drugs Antiplatelet Drugs LaHaye SA and colleagues, European Heart Journal 2012 LaHaye SA and colleagues, European Heart Journal 2012 Validation table for CHA 2 DS 2 VASc Treatment Recommendation (Lowest Attributable Net Risk) Score = 4, HAS-BLED score = 2 LaHaye SA and colleagues, European Heart Journal 2012 LaHaye SA and colleagues, European Heart Journal 2012 3
6/20/2016 Meta-Analysis of NOAC RCTs Meta-Analysis of NOAC RCTs Stroke or systemic embolism Secondary efficacy and safety outcomes Major bleeding Ruff CT and colleagues, The Lancet 2014 Ruff CT and colleagues, The Lancet 2014 Subgroup Subgroup Analysis Analysis Ruff CT and colleagues, The Lancet 2014 Ruff CT and colleagues, The Lancet 2014 4
6/20/2016 Recommendations for Resources Pharmacologic Stroke Prevention • Aspirin (low efficacy) • AF clinical decision aid: • Warfarin (low cost) – http://www.afib.ca/ • Dabigatran (lowest stroke risk) • Rivaroxaban (once daily dosing) • Edoxaban (once daily dosing, CrCl ≤ 95 ml/min) • Mobile app: • Apixaban (lowest net risk) – Afib CDA • Aspirin + Clopidogrel (modest efficacy, high bleeding – http://SPARCtool.com/ risk) • American College of Cardiology Interactions with medications, diet, patient preferences, – http://www.teamanticoag.com/ monitoring requirements, renal failure Phone/iPad app: Afib CDA Phone app: SPARCtool.com $4.99 *Not in your handout 5
6/20/2016 Case #2 Phone app: SPARCtool.com MF is an 80 yo M with PAF who has a h/o HTN, DM, a TIA, and PUD s/p GIB while on warfarin. How can his risk of subsequent thromboembolic event best be minimized? 61% A. Warfarin plus PPI B. Apixaban 27% C. Aspirin and clopidogrel 10% 2% D. Intervention on the left n I l P a e . atrial appendage P b r . g a . s a u x o t d f l p i e p p i A l n o e i l h r c a t f d n r n a o a W n n i o r i i t p n s e A v r e t n I Watchman Watchman Data • Self-expanding nitinol frame covered by fabric • Short-term anticoagulation recommended • 2 RCTs (1261 pts) + 2 registries (1145 pts) • Now FDA approved! • Non-inferior to warfarin (mostly) • Provider experience important – Complication rate: 7.7% -> 2.2% • 99% off warfarin within a year • NOAC comparisons not yet done Jain AK and colleagues, Heart 2011 6
6/20/2016 Meta-Analysis: Watchman vs. Warfarin Meta-Analysis: Watchman vs. Warfarin Decreased: Increased: Decreased: • Hemorrhagic strokes • Ischemic strokes • CV / unexplained death No difference in all stroke or systemic embolism Trend toward decrease in all-cause death Meta-Analysis: Watchman vs. Warfarin Meta-Analysis: Watchman vs. Warfarin Decreased: Increased: Decreased: Increased: • Nonprocedural bleeding • Procedural bleeding • Hemorrhagic strokes • Ischemic strokes • CV / unexplained death • Procedural bleeding No difference in major bleeding • Nonprocedural bleeding 7
6/20/2016 Amplatzer cardiac plug (ACP) LARIAT snare • Percutaneous ligation of LAA • Limited short-term results favorable • Painful • Nitinol only, barbs to increase stability • Complicated • High deployment success • Risky? • Low stroke/embolism rate • Available in the US • 16% peri-device leak at 6 mo f/u via 510(K) approval • No real trial data process • Not approved in US; approved in Europe Jain AK and colleagues, Heart 2011 Chatterjee S and colleagues, Ann Thorac Surg 2011 Urena M and colleagues, JACC 2013 Thoracoscopic stand-alone True anticoagulation alternative? left atrial appendectomy • 150 pt Watchman (ASAP) 60 pt Amplatzer study – Both non-randomized – Off anticoagulation – Lower than predicted stroke / embolism rates – 4% thrombus formation on Watchman (can occur late) • Well-established as • Non-appendage clot sites part of cardiac surgery • Very limited data on • Hybrid approach: low- stand-alone procedure dose NOAC + Watchman? • Surgery! Reddy VY and colleagues, JACC 2013 Wiebe J and colleagues, Catheter Cardiovasc Interv 2014 Ohtsuka T and colleagues, JACC 2013 Perk G and colleagues, Eur Heart J Cardiovasc Imaging 2011 8
6/20/2016 Case #3 Recommendation MJ has h/o HTN and PAF x 1 year. Now for the first time she has not converted spontaneously. • European Society of Cardiology: weak Which meds should she be given with CV? recommendation for those with high stroke 44% risk and contraindication to long-term A. Anticoagulant only anticoagulation B. Anticoagulant and AVN blocker 23% 18% 15% C. Anticoagulant, Flecainide, and • Not yet part of US guidelines AVN blocker • FDA: “suitable for warfarin” + “appropriate D. Anticoagulant and Amiodarone y . l . n . . e . . . o . . reason to seek a non-drug alternative” d o N t n i m i n V a A i a A u l c d e d g n a l n a F o a c t , n n t t i n n t a a a l A u u l u l g g g a a a o o o c c i c t t i i n n t n A A A Antiarrhythmic Treatment Prior to CV Pharmacologic cardioversion • Enhance ability to cardiovert • One week or less of AF – Dofetilide / Ibutilide • Avoid need for electrical cardioversion – Flecainide / Propafenone – No sedation – +/- Amiodarone – No scheduling • > 1 week of AF – Same need for anticoagulation – Dofetilide • Minimize risk of early recurrence – +/- Ibutilide, Amiodarone • Establish medication tolerability 9
6/20/2016 Meta-Analysis of Antiarrhythmic maintenance Efficacy of AADs >1 AF episode Placebo = 25% efficacy (95% CI: 15-34%) Long-term AAD Meds sinus possible use possible 52% with no AF Symptoms (95% CI: 47-57%) or poor average f/u = 1 yr rate control Calkins H and colleagues, Circ Arrhythm Electrophysiol 2009 Differential drug effectiveness Guideline Recommendations (SAFE-T – persistent AF pts) Time to AF recurrence after CV • Spontaneous conversion: ~ 25% (drugs) vs < 1% (placebo) • Failure of CV: ~ 25% (drugs) vs 33% (placebo) • Amiodarone 6x more effective than Sotalol • Both best placebo January CT and colleagues, JACC 2014 Singh BH and colleagues, NEJM 2005 10
6/20/2016 Case #4 My Recommendations GG is a 60 yo F with PAF and HTN who has episodes despite treatment with metoprolol. Why should she consider AF ablation? 33% A. Decrease AF symptomatic 28% 25% burden B. Minimize stroke risk 14% C. Decrease likelihood of developing HF D. Improve her survival Minimize stroke risk Decrease AF symptomat.. Improve her survival Decrease likelihood of d... January CT and colleagues, JACC 2014 Reasons for AF ablation AF ablation • Improvement of QOL Goal = Elimination of • ?Decreased stroke risk triggers and alteration of substrate • ?Decreased heart failure risk • ?Improved survival Calkins H and colleagues, Heart Rhythm 2012 11
6/20/2016 Meta-Analysis of AF Ablation Efficacy Outcomes - PAF 57% 71% 72% 77% AF ablation Medications ~60-75% efficacy 52% efficacy 5% complication rate 30% adverse events 26% Meta-analysis of RCTs only: 1 >1 1 >1 No No + + 77.8% efficacy 23.3% efficacy AAD AAD AAD AAD Repeat Bonanno C and colleagues, J Cardiovasc Med 2010 Calkins H and colleagues, Circ Arrhythm Electrophysiol 2009 Calkins H and colleagues, Circ Arrhythm Electrophysiol 2009 Persistent AF Abla�on ≠ Cure Single procedure success Multiple procedure success Weerasooriya and colleagues, JACC 2011 Verma A and colleagues, NEJM 2015 12
Recommend
More recommend