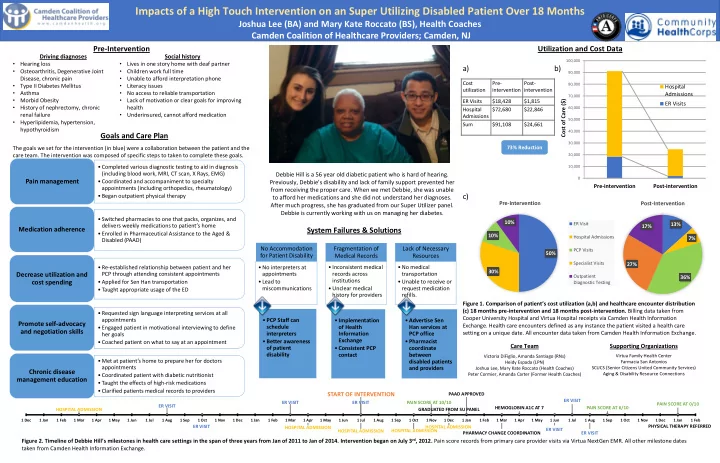
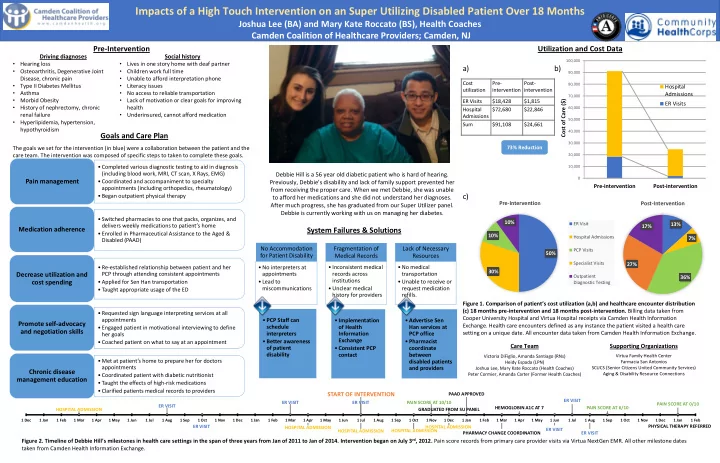
Impacts of a High Touch Intervention on an Super Utilizing Disabled Patient Over 18 Months Joshua Lee (BA) and Mary Kate Roccato (BS), Health Coaches Camden Coalition of Healthcare Providers; Camden, NJ Pre-Intervention Utilization and Cost Data Driving diagnoses Social history 100,000 • • Hearing loss Lives in one story home with deaf partner a) b) • • Osteoarthritis, Degenerative Joint Children work full time 90,000 • Disease, chronic pain Unable to afford interpretation phone Cost Pre- Post- • • 80,000 Type II Diabetes Mellitus Literacy issues Hospital utilization intervention intervention • • Asthma No access to reliable transportation Admissions 70,000 • • Morbid Obesity Lack of motivation or clear goals for improving ER Visits $18,428 $1,815 Cost of Care ($) ER Visits • History of nephrectomy, chronic health 60,000 Hospital $72,680 $22,846 • renal failure Underinsured, cannot afford medication Admissions 50,000 • Hyperlipidemia, hypertension, Sum $91,108 $24,661 hypothyroidism 40,000 Goals and Care Plan 30,000 73% Reduction The goals we set for the intervention (in blue) were a collaboration between the patient and the care team. The intervention was composed of specific steps to taken to complete these goals. 20,000 • Completed various diagnostic testing to aid in diagnosis 10,000 (including blood work, MRI, CT scan, X Rays, EMG) Debbie Hill is a 56 year old diabetic patient who is hard of hearing. 0 Pain management • Coordinated and accompaniment to specialty Previously, Debbie’s disability and lack of family support prevented her Pre-intervention Post-intervention appointments (including orthopedics, rheumatology) from receiving the proper care. When we met Debbie, she was unable c) • Began outpatient physical therapy to afford her medications and she did not understand her diagnoses. Pre-Interventio n Post-Intervention After much progress, she has graduated from our Super Utilizer panel. Debbie is currently working with us on managing her diabetes . • Switched pharmacies to one that packs, organizes, and 10% ER Visit 13% delivers weekly medications to patient’s home 17% Medication adherence System Failures & Solutions • Enrolled in Pharmaceutical Assistance to the Aged & 10% Hospital Admissions 7% Disabled (PAAD) No Accommodation Fragmentation of Lack of Necessary PCP Visits 50% for Patient Disability Medical Records Resources Specialist Visits 27% • Re-established relationship between patient and her • No interpreters at • Inconsistent medical • No medical 30% records across transportation Decrease utilization and PCP through attending consistent appointments appointments Outpatient 36% institutions • Applied for Sen Han transportation • Lead to • Unable to receive or cost spending Diagnostic Testing • Unclear medical request medication . miscommunications • Taught appropriate usage of the ED history for providers refills. Figure 1. Comparison of patient’s cost utilization ( a,b) and healthcare encounter distribution (c) 18 months pre-intervention and 18 months post-intervention. Billing data taken from • Requested sign language interpreting services at all Cooper University Hospital and Virtua Hospital receipts via Camden Health Information appointments • PCP Staff can • Implementation • Advertise Sen Promote self-advocacy Exchange. Health care encounters defined as any instance the patient visited a health care schedule of Health Han services at • Engaged patient in motivational interviewing to define and negotiation skills setting on a unique date. All encounter data taken from Camden Health Information Exchange. interpreters Information PCP office her goals Exchange • Better awareness • Pharmacist • Coached patient on what to say at an appointment Care Team Supporting Organizations of patient • Consistent PCP coordinate disability contact between Virtua Family Health Center Victoria DiFiglio, Amanda Santiago (RNs) • Met at patient’s home to prepare her for doctors disabled patients Farmacia San Antonios Heidy Espada (LPN) appointments and providers SCUCS (Senior Citizens United Community Services) Joshua Lee, Mary Kate Roccato (Health Coaches) Chronic disease Aging & Disability Resource Connections Peter Cormier, Amanda Carter (Former Health Coaches) • Coordinated patient with diabetic nutritionist management education • Taught the effects of high-risk medications • Clarified patients medical records to providers START OF INTERVENTION PAAD APPROVED ER VISIT ER VISIT ER VISIT PAIN SCORE AT 10/10 PAIN SCORE AT 0/10 ER VISIT HEMOGLOBIN A1C AT 7 PAIN SCORE AT 6/10 HOSPITAL ADMISSION GRADUATED FROM SU PANEL 1 Dec 1 Jan 1 Feb 1 Mar 1 Apr 1 May 1 Jun 1 Jul 1 Aug 1 Sep 1 Oct 1 Nov 1 Dec 1 Jan 1 Feb 1 Mar 1 Apr 1 May 1 Jun 1 Jul 1 Aug 1 Sep 1 Oct 1 Nov 1 Dec 1 Jan 1 Feb 1 Mar 1 Apr 1 May 1 Jun 1 Jul 1 Aug 1 Sep 1 Oct 1 Nov 1 Dec 1 Jan 1 Feb PHYSICAL THERAPY REFERRED ER VISIT HOSPITAL ADMISSION HOSPITAL ADMISSION ER VISIT HOSPITAL ADMISSION HOSPITAL ADMISSION PHARMACY CHANGE COORDINATION ER VISIT Figure 2 . Timeline of Debbie Hill’s milestones in health care settings in the span of three years from Jan of 2011 to Jan of 2014. In tervention began on July 3 rd , 2012. Pain score records from primary care provider visits via Virtua NextGen EMR. All other milestone dates taken from Camden Health Information Exchange.
“Erasing the Hotspot” Through Community Partnership Finding the Hotspot – Why Northgate II? Seeing that the initial interventions achieved Segments Represent People Segmentation: limited engagement of the highest utilizing “ the Hotspot within the Hotspot ” residents, we are now working to create a community-based care management model that comes alongside primary care to reach every hospitalized patient. Hospital Claims % Receipts Next Steps: Designing workflows around each segment, starting with the highest utilizers Ms. Suarez* is a 57 year old woman who lives Hospital Utilization history for Ms. Suarez • 64 residents (19% of Build- • 220 residents (66% of alone with assistance 6 ing) Building) Length of Stay (Days) from a visiting home The Camden Coalition of Healthcare Providers was able to pool the claims data from the 3 hospitals in 5 • Better linkage to primary • Preventative Health the city of Camden, NJ. Analysis of hospital-based healthcare costs revealed two striking findings. # of Residents 220 64 29 20 4 health aid. She goes to an care (especially for % of Building 66% 19% 9% 6% • Education First, it identified “superutilizers,” patients who consume a disproportionate amount of healthcare % of Receipts 8.2% 21.4% 9.2% 61.2% 3 adult day program every chronic conditions) resources. In Camden, the top 1% of patients account for 30% of the hospital-based medical costs. • Activities (Yoga, Exercise) 2 afternoon. Driving The second finding was that high-utilizing patients tend to be geographically clustered together in • Improved transportation • Coaching / Supporting 1 “hotspots” of medical cost. One of these hotspots was Northgate II, a 23-story high rise with 308 diagnoses for her While the in-building PCP practice served apartments for the elderly and disabled. 0 hospitalizations were Jan-11 Mar-11 May-11 Jul-11 Sep-11 Nov-11 Jan-12 Mar-12 May-12 Jul-12 Sep-12 Nov-12 Jan-13 Mar-13 May-13 Jul-13 Sep-13 Nov-13 Jan-14 proportionally more of the highest utilizing • 20 residents (6% of Build- • 29 residents (9% of build- COPD and stroke. She ing) ing) has difficulty speaking Inpt Obs ER residents, it engaged only about a third of the • Care Coordination • Better linkage to primary and residual left-sided First Interventions Timeline • Home visits post- care (especially for inpatient high utilizers. weakness from her chronic conditions) discharge System challenges identified: • Care coordination • Medical reconciliation Earlier efforts to improve the health of NGII residents and “erase • Education on use of ED • Scheduling In-building PCP Outside PCP Patients the hotspot” had not engaged this patient • Transportation to primary • Post-discharge planning Patients Polypharmacy with duplication of therapeutic class from different care (off-hours) • Health coaching providers • Redi-Clinic 4.6% Multiple barriers to medication adherence 13 7 13.5% 27 9.6% 2 3.8% 49 Final Steps: Current High Inpatient Utilizer Program goals: 17.5% Reduce preventable inpatient and emergency room utilization 14 Community Partner Investment and Development for 26.9% PCP follow-up within 7 days of hospital discharge Program Sustainability Improve the health of NGII residents and the cultivation of a healthy community Enhance capacity for Fairshare Housing to promote a sustainable, healthy community 191 Bend the cost curve & “eliminate the hotspot” 29 55.8% 68.2% HIE daily report Bedside visits 1st Home vis- Accompany Follow up visit in identifies any in the hospital it within 24- patient to 1st PCP 48 hours & hand- hospitalized – twice if pos- 48 hours of visit within 7 days off to NGII Social resident sible discharge of discharge Services Depart- 52 280 with ment medication reconciliation
Recommend
More recommend