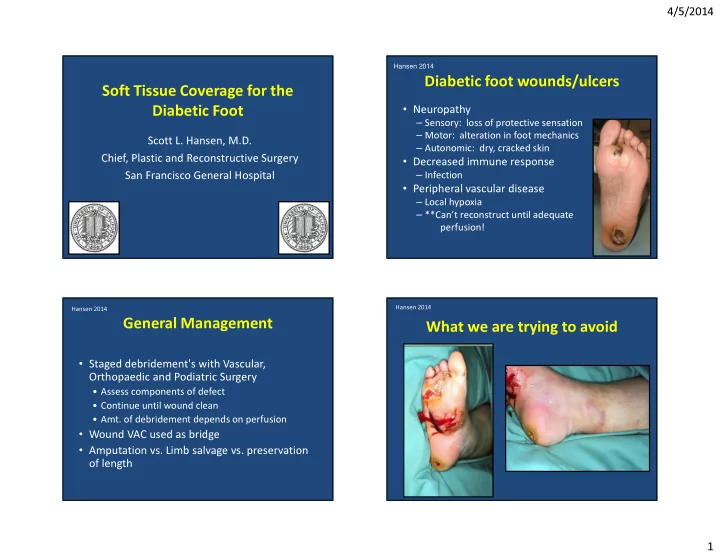
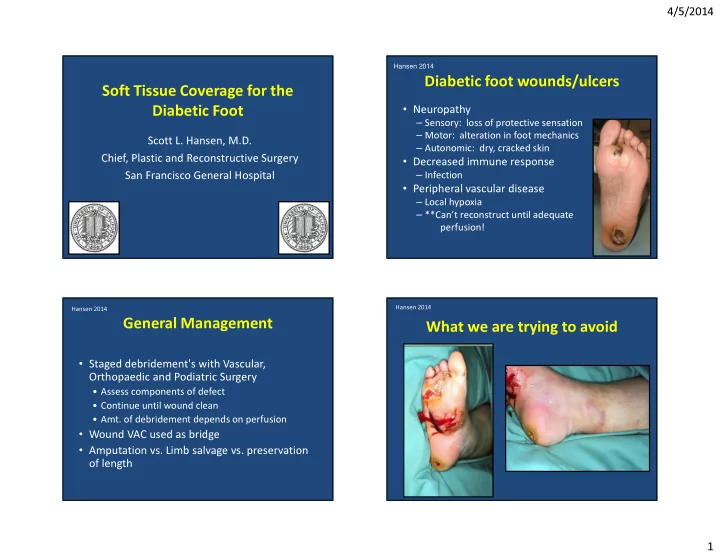
4/5/2014 Hansen 2014 Diabetic foot wounds/ulcers Soft Tissue Coverage for the • Neuropathy Diabetic Foot – Sensory: loss of protective sensation – Motor: alteration in foot mechanics Scott L. Hansen, M.D. – Autonomic: dry, cracked skin • Decreased immune response Chief, Plastic and Reconstructive Surgery – Infection San Francisco General Hospital • Peripheral vascular disease – Local hypoxia – **Can’t reconstruct until adequate perfusion! Hansen 2014 Hansen 2014 General Management What we are trying to avoid • Staged debridement's with Vascular, Orthopaedic and Podiatric Surgery • Assess components of defect • Continue until wound clean • Amt. of debridement depends on perfusion • Wound VAC used as bridge • Amputation vs. Limb salvage vs. preservation of length 1
4/5/2014 Hansen 2014 Hansen 2014 Wound Analysis What we are trying to avoid • Location • Hindfoot/Midfoot/Forefoot • Wound size • Components of wound – Skin -Nerve - Subcutaneous tissue -Cartilage – Muscle -Bone – Vessels • Etiology • Pressure, non-compliance Result = Amputation Hansen 2014 Hansen 2014 Healing / Secondary Intention Reconstructive Ladder – pulls “ like ” tissue into wound • Advantage • Disadvantage – duration of healing • Consider for smaller wounds 2
4/5/2014 Hansen 2014 Hansen 2014 Indications for Flap Coverage Split-Thickness Skin Graft • Skin graft cannot be used – Exposed cartilage, tendon (without paratenon), bone, open joints, metal implants • Flap coverage is preferable – Exposed nerves or vessels, durability required, multiple tissues required, dead space present Hansen 2014 Hansen 2014 Reconstructive options depend on Principles location of wound • The final reconstruction should be functional Forefoot – Durable – Maintain Sensation – Contour (not bulky) Mid plantar Hindfoot/Heel/Malleolus 3
4/5/2014 Hansen 2014 Hansen 2014 Hindfoot & Mid Plantar Hindfoot & Mid Plantar • Goal is to provide sensate coverage by using like • >2/3 of heel tissue from non-weight bearing midsole area • Free tissue transfer • <1/3 of heel • Non-weight bearing heel, instep, malleoli • Split & full thickness skin grafts • Skin graft • Sural Flap: Suprafascial rotation flap • Rotation flaps • 1/3 to 2/3 of heel • Reverse pedicled fasciocutaneous flaps • Flexor digitorum brevis muscle turnover flap • Extensor digitorum brevis flap • Instep island flap • Abductor hallucis & abductor digiti minimi muscle flap • Free muscle or fasciocutaneous flap if deep Hansen 2014 Hansen 2014 Hindfoot Hindfoot Calcanectomy & closure Flexor digitorum brevis flap 4
4/5/2014 Hansen 2014 Hansen 2014 Hindfoot Hindfoot Reconstruction Flexor digitorum brevis flap Blood Supply: Branches of Medial and Lateral Plantar artery Hansen 2014 Hansen 2014 Hindfoot Reconstruction Flexor digitorum brevis flap 5
4/5/2014 Hansen 2014 Hansen 2014 Hindfoot Instep island flap Local rotational flap, Length:Width ratio 2:1 Based on branches of the medial plantar artery Hansen 2014 Hansen 2014 V to Y Advancement 6
4/5/2014 Hansen 2014 Hansen 2014 Lateral Calcaneal Artery Flap Lateral Supramalleolar Flap *Supplied by a perforating branch of the peroneal artery Hansen 2014 Hansen 2014 Lateral Calcaneal Artery Flap Lateral Calcaneal Artery Flap 7
4/5/2014 Hansen 2014 Hansen 2014 Sural Flap Neurocutaneous Flap • Sural artery flap • Small artery and vein supplying the sural nerve • Pivot point is 5cm proximal to lateral malleolus (peroneal artery) Hansen 2014 Hansen 2014 Midfoot Sural Flap V-Y advancement island flaps 8
4/5/2014 Hansen 2014 Hansen 2014 Midfoot V-Y advancement flaps Hansen 2014 Hansen 2014 Microvascular Transplantation (MVT) Plantar rotation flaps • Myriad of Flaps Available • Based on the vascular plexus superficial to the • Muscle plantar fascia • Skin • Donor site is skin grafted • Combination • Dead space present • Osteomyelitis • Local tissues not available 9
4/5/2014 Hansen 2014 Hansen 2014 Muscle and Musculocutaneous Flaps Fasciocutaneous and Perforator Flaps • Latissimus dorsi • Radial Forearm Flap • Rectus abdominis • Anterolateral Thigh Flap • Gracilis Hansen 2014 Hansen 2014 Heel Reconstruction Muscle vs. fasciocutaneous flap coverage 10
4/5/2014 Hansen 2014 Hansen 2014 Hindfoot Heel Reconstruction Latissimus flap Hansen 2014 Hansen 2014 Hindfoot Hindfoot Latissimus flap Latissimus free flap 11
4/5/2014 Hansen 2014 Hansen 2014 Perforator Flap Perforator Flap Anterolateral thigh flap (ALT): Blood supply- Descending branch of the lateral circumflex Hansen 2014 Hansen 2014 Perforator Flap Forefoot • Plantar flaps cannot be mobilized distally due to tethering effect by plantar nerves • Sensate toe flap; unfavorable donor defect • Free tissue transfer provide most stable, durable coverage – Latissimus dorsi muscle flap 12
4/5/2014 Hansen 2014 Hansen 2014 Forefoot Forefoot Ray amputation +STSG Transmetatarsal amputation Hansen 2014 Hansen 2014 Forefoot Forefoot Transmetatarsal amputation Transmetatarsal amputation 13
4/5/2014 Hansen 2014 Hansen 2014 Forefoot Forefoot Toe filet flaps Neurovascular island flaps Hansen 2014 Hansen 2014 Forefoot Forefoot Neurovascular island flaps V-Y advancement flaps 14
4/5/2014 Hansen 2014 Hansen 2014 Forefoot Large Defects V-Y advancement flaps Hansen 2014 Hansen 2014 Large Defects Large Defects 15
4/5/2014 Hansen 2014 Hansen 2014 Midfoot Amputation Salvage Hansen 2014 Hansen 2014 Midfoot Foot Dorsum Amputation Salvage • Skin grafts • Direct exposed tendon or bone – Free flaps • Radial forearm/ALT flap • Latissimus muscle • Gracilis flap 16
4/5/2014 Hansen 2014 Hansen 2014 Post-op Management • Foot immobilization post-op – Consider ex-fix • Protect pressure points • Continue to optimize medical management • Close follow-up Hansen 2014 Conclusions • Team approach = more chance of success • Reconstructive ladder helpful in choosing reconstruction • Limb salvage prolongs survival of diabetic patients • Diabetes is NOT a contraindication to local or free flap reconstruction 17
Recommend
More recommend