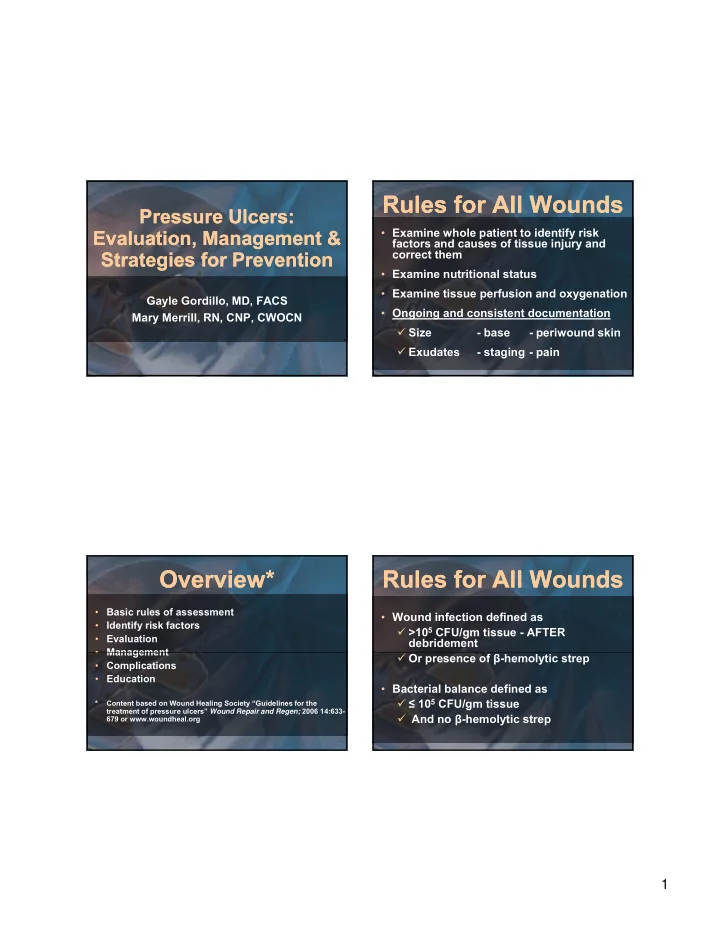
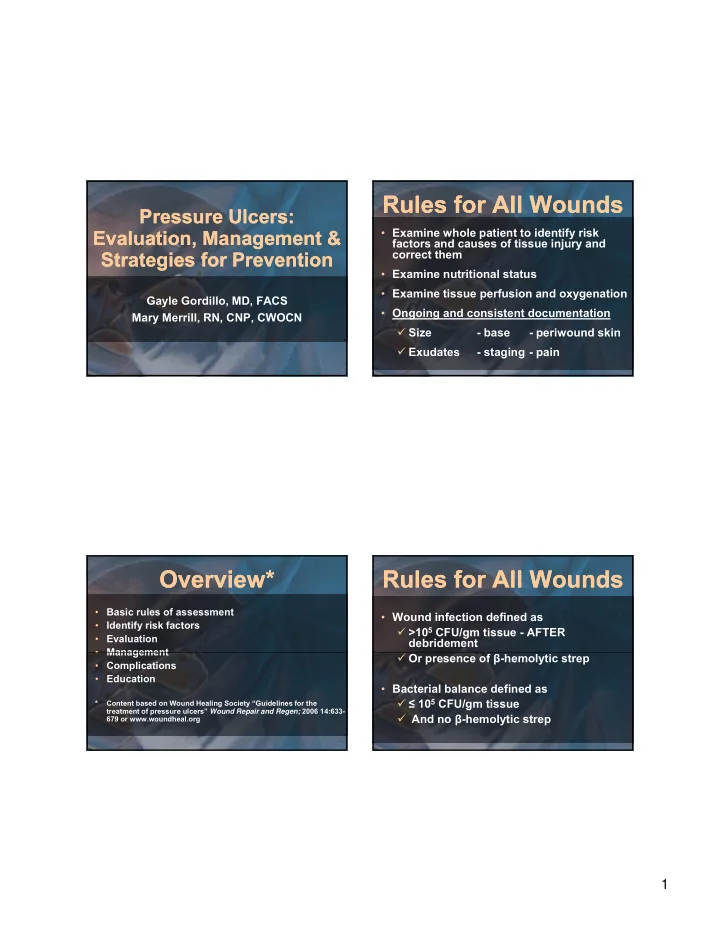
Rules for All Wounds Rules for All Wounds Pressure Ulcers: Pressure Ulcers: • Examine whole patient to identify risk Evaluation, Management & Evaluation, Management & factors and causes of tissue injury and correct them Strategies for Prevention Strategies for Prevention • Examine nutritional status • Examine tissue perfusion and oxygenation Gayle Gordillo, MD, FACS • Ongoing and consistent documentation Mary Merrill, RN, CNP, CWOCN � Size - base - periwound skin � Exudates - staging - pain Overview* Overview* Rules for All Wounds Rules for All Wounds • Basic rules of assessment • Wound infection defined as • Identify risk factors � >10 5 CFU/gm tissue - AFTER • Evaluation debridement • Management • Management � Or presence of β -hemolytic strep • Complications • Education • Bacterial balance defined as � ≤ 10 5 CFU/gm tissue * Content based on Wound Healing Society “Guidelines for the treatment of pressure ulcers” Wound Repair and Regen; 2006 14:633- � And no β -hemolytic strep 679 or www.woundheal.org 1
Risk Factors Risk Factors Yeast Dermatitis Yeast Dermatitis • Poor nutritional status • Flexion contractures • Wheelchair - esp extremes of mobility • Prolonged hospitalization with bedrest • Mechanical/shear � Transfers � Hygiene • Moisture – especially incontinence Etiology Etiology Incontinence Dermatitis Incontinence Dermatitis • External pressure exceeds capillary pressure (20-30 mmHg) • Pressure is greatest over bony prominences � Must be over bony prominence Must be over bony prominence � Decubitus= pressure sore acquired while recumbent � Ischial sore = sitting sore • Cone of destruction with apex at skin surface � Muscle tissue least tolerant of ischemia � Skin most tolerant to ischemia 2
Stage II Pressure Ulcer Stage II Pressure Ulcer Stage I Pressure Ulcer Stage I Pressure Ulcer Stage III Pressure Ulcer Stage III Pressure Ulcer 3
Deep Tissue Injury Deep Tissue Injury Stage IV Pressure Ulcer Stage IV Pressure Ulcer Evaluation Evaluation Unstageable Pressure Ulcer Unstageable Pressure Ulcer • Critical surfaces � Chair � Cushion � M � Mattress • Pressure mapping • Nutritional status � Pre-albumin � Albumin for renal failure patients 4
Evaluation Evaluation Evaluation Evaluation • Assess nutrition on entry to new health care system or change in condition • Ambulatory status – avoid bedrest, unless • Ensure adequate dietary intake an ischial sore is present • Encourage dietary supplements if deficiency • Flexion contractures Flexion contractures suspected • Spasticity � Appetite stimulants • Incontinence/moisture � MVI � Increase protein intake • Monitor nutritional status with weekly pre- albumin levels Management Management Evaluation Evaluation • Physical exam • Establish repositioning schedule and avoid � Location positioning on wound � Measurements: L x W x D, tunneling • Maintain head of bed at lowest elevation � Appearance pp possible ( < 30º elevation) • Odor • Use pressure reducing surface for high risk • Size patients • Base/necrotic debris • Periwound skin • Get seat and cushion check yearly • Exudates • Staging 5
Management Management Management Management • Use topical antimicrobials to decrease • Perform initial and maintenance infected wound bacterial levels debridement • Remove all necrotic debris � IV antibiotics do not effectively decrease bacterial levels in granulating wounds bacterial levels in granulating wounds � Enzymatic � Once in “bacterial balance” (10 5 CFU/gm � Sharp tissue and no β -hemolytic strep) d/c � Mechanical topical antimicrobials • Infection control – reduce bacterial burden/ • Achieve “bacterial balance” before achieve “bacterial balance” attempting surgical closure Management Management Management Management • Wounds can harbor persistent organisms • Routine wound cleansing with neutral non- due to contamination from distant sites of toxic solution infection, e.g. urine • Achieve local moisture balance • Infection surveillance – obtain specimen Infection surveillance obtain specimen AFTER debridement � Maintain moist wound environment � Tissue biopsy - preferred � Manage exudate to protect periwound skin • Dressing must stay in place and minimize � Quantitative swab culture shear/friction/skin irritation • Check for infection if ≥ 2 weeks stalled • Select cost effective dressing healing in debrided wound 6
Wound Dressings Wound Dressings Complications Complications Dressing Indications Examples • Infection foam med exudate Mepilex � Tissue biopsy/quantitative swab for antibacterial infected Kerlix AMD culture alginate hi exudate - requires Kaltostat, Silvercel � Radiology gy secondary drsg hydrogel dry or fibrinous exudate, Duoderm gel � Labs granulating hydrocolloid superficial wound with Duoderm • Secondary Amyloidosis minimal exudate hydrofiber low exudate - autolytic Aquacel (Ag) • Autonomic dysreflexia – peri-op debride bioactive advanced therapy Regranex, Promogran • Marjolin’s ulcer barriers periwound maceration Aloe Vesta • Urethrocutaneous fistula Aloe Vesta antifungal Management Management • Negative Pressure Wound Therapy � Indications • Stage III or IV ulcer • Clean wound � Contraindications • Dirty/not debrided ( > 30% necrotic tissue) • Fistula • Stool or urine contamination • Active bleeding • Untreated osteo 7
Candidates for Surgery Candidates for Surgery • Grade III or Grade IV ulcer • Clean wound Clean wound • Chair and cushion evaluated ≤ 12 mos • Adequate nutritional status Candidates for Surgery Candidates for Surgery • Spasticity controlled • No significant flexion contractures • Evidence of patient compliance � Post-op bedrest for 30 days � One sore repaired per surgery • Adequate psychosocial support � Pt insight into ulcer condition � Evidence of social support structure 8
Causes of Surgical Failure Causes of Surgical Failure • Spasticity • Flexion contractures • Improper cushion • Infection Infection � Hold bowel regimen immed post-op x 72 hours � Urinary catheter • Hematoma/seroma • Shear -poor patient compliance with bedrest • Poor nutritional status Education Education • Patient and their caregivers � Pressure relief � Moisture � Nutrition � Chair and cushion selection and maintenance � Psychosocial support 9
Education Education Resources Resources • Health care providers - especially for prevention 1. Ohio State’s Wheelchair Seating and Positioning Clinic • of ulcers � Dodd Hall Rehabilitation Services Outpatient Therapy � Pressure relief OSU Martha Morehouse Medical Plaza � Frequent checks 2050 Kenny Road, Suite 2100 • Columbus, Ohio 43221 • 3P’s: pain, positioning, potty (614) 293-3847 (phone) • (614) 293-6400 (fax) (614) 293 3847 (phone) (614) 293 6400 (fax) • Skin- esp around devices, e.g splints, cervical collars, etc � Management of incontinence 2. Information for finding a good rehab Suplier/Clinican • � Physical Therapy to prevent flexion outside of central Ohio: contractures � http://resna.org/find-a-certification (has listing of ATP � Nutrition support professionals across the country) � Infection surveillance � www.nrrts.org (resource for w/c suppliers) � Consistent and ongoing documentation Summary Summary Optimize conditions for both prevention and healing • � Pressure relief • Surfaces • Positioning • Chair and cushion pressure mapping � � Moisture management Moisture management Nutritional monitoring/optimization � � Infection surveillance � Prevention of flexion contractures � Education • Patient • Family/caregiver • Healthcare staff Consider referral to Wound Care Center • 10
Recommend
More recommend