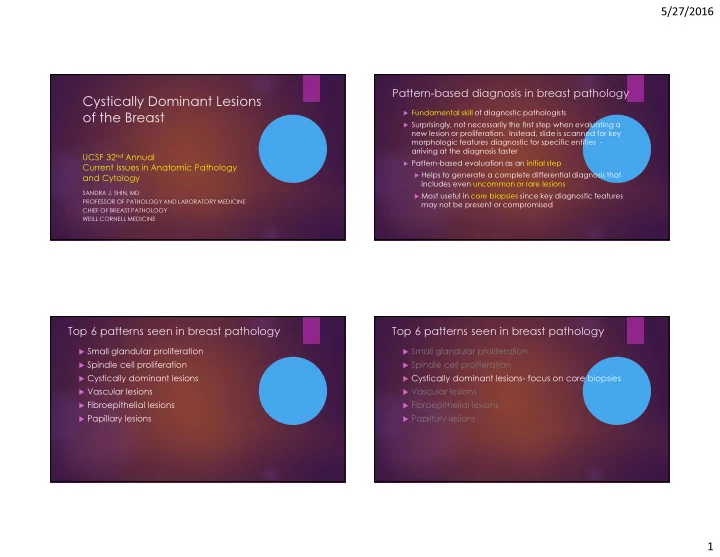
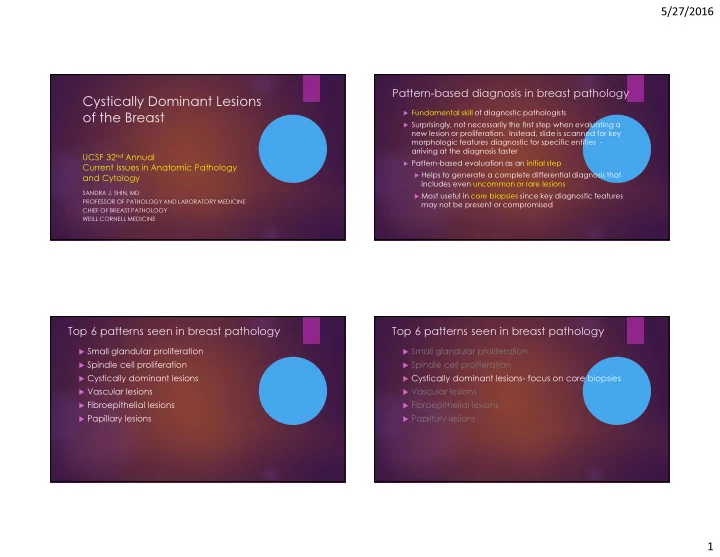
5/27/2016 Pattern-based diagnosis in breast pathology Cystically Dominant Lesions � Fundamental skill of diagnostic pathologists of the Breast � Surprisingly, not necessarily the first step when evaluating a new lesion or proliferation. Instead, slide is scanned for key morphologic features diagnostic for specific entities - arriving at the diagnosis faster UCSF 32 nd Annual � Pattern-based evaluation as an initial step Current Issues in Anatomic Pathology � Helps to generate a complete differential diagnosis that and Cytology includes even uncommon or rare lesions SANDRA J. SHIN, MD � Most useful in core biopsies since key diagnostic features PROFESSOR OF PATHOLOGY AND LABORATORY MEDICINE may not be present or compromised CHIEF OF BREAST PATHOLOGY WEILL CORNELL MEDICINE Top 6 patterns seen in breast pathology Top 6 patterns seen in breast pathology � Small glandular proliferation � Small glandular proliferation � Spindle cell proliferation � Spindle cell proliferation � Cystically dominant lesions � Cystically dominant lesions- focus on core biopsies � Vascular lesions � Vascular lesions � Fibroepithelial lesions � Fibroepithelial lesions � Papillary lesions � Papillary lesions 1
5/27/2016 Cystically Dominant Lesions with calcs +/- secretions NEEDLE MAMMO � Larger caliber ducts CORE CALCS BIOPSY � Cysts in the fibrocystic disease � Duct stasis/ duct ectasia � Cystic hypersecretory lesions � Juvenile Papillomatosis � Lobulocentric / TDLU DIAGNOSIS � Columnar cell lesions and flat epithelial atypia � Pregnancy-like (pseudolactational) change or hyperplasia � Mucocele-like lesions Secretions and Calcifications Cysts of fibrocystic disease � Secretions www.pathology.washington.edu � May or may not be present within glandular/cystic lumens � Vary in amount, color, consistency � None are pathognomic for an entity � Calcifications � Associated with full spectrum of breast disease Blue-domed Cyst � Vary in amount, size, appearance, location � None are pathognomic for an entity 2
5/27/2016 Cysts of fibrocystic disease Cysts of fibrocystic disease Calcium Oxalate Crystals Thin, translucent lightly eosinophilic or basophilic secretions Duct ectasia Cysts of fibrocystic disease on core biopsy No excisional biopsy if there is pathologic-radiologic concordance Courtesy of Dr. Timothy D’Alfonso 3
5/27/2016 Duct stasis Duct ectasia No calcifications Macrophages Fluffy translucent lightly eosinophilic secretions Translucent pale blue/gray secretions Duct ectasia on core biopsy Cystic Hypersecretory Lesions No excisional biopsy if there is pathologic-radiologic concordance 4
5/27/2016 Cystic hypersecretory lesions Cystic hypersecretory hyperplasia CAN BE MISTAKEN FOR CYSTS OF FIBROCYSTIC DISEASE AT SCANNING MAGNIFICATION Parallel Cracks “Venetian Blinds” Histiocytes Lymphocytic inflammation Retracted Dense Colloid-Like 5
5/27/2016 Am J Surg Pathol 2014; 38:45-53 Atypical cystic hypersecretory hyperplasia 10 patients; female; average age 63 years Clinical presentation: mass but also calcifications and bloody nipple discharge Microscopic extent: 9 mm (2 mm to 2.7 cm) Histology: micropapillary growth pattern; intermediate or high nuclear grade arising in a background of CHH and/or atypical CHH Biomarker profile: ER+ HER2- (80%) ER/PR- HER2- (20%) including one case with microinvasive carcinoma and micrometastasis to one SLN 1/10 (10%) lacked investing myoepithelium by p63, SMM, CK5 Treatment of 4 patients: EXBX + RT (2 patients); EXBX + RT + Chemo (1 patient); MX + Tamoxifen (1 patient) Clinical follow-up: All NED mean 5.5 years Cystic hypersecretory (in-situ) carcinoma 6
5/27/2016 Invasive cystic hypersecretory carcinoma Cystic hypersecretory (in-situ) carcinoma DIMINISHED SECRETIONS AND HIGH NUCLEAR GRADE ER Cystic hypersecretory hyperplasia on core biopsy Columnar cell lesions Flat epithelial atypia Recommend excisional biopsy regardless of pathologic-radiologic concordance or lack of atypia 7
5/27/2016 Flat epithelial atypia Columnar cell change (columnar cell change with atypia) FLAT EPITHELIAL ATYPIA FLAT EPITHELIAL (COLUMNAR CELL ATYPIA CHANGE WITH ATYPIA) (COLUMNAR CELL HYPERPLASIA WITH ATYPIA) Courtesy of Dr. Stuart Schnitt Courtesy of Dr. Stuart Schnitt 8
5/27/2016 Columnar Cell Flat Epithelial Atypia Columnar Cell Change Hyperplasia Hallmark Features Columnar Cell Change Flat Epithelial Atypia � Elongated nuclei � Rounded nuclei � Epithelial polarization � Loss of epithelial polarization “jumbled” � No cytologic atypia � Low grade cytologic � Round or irregular shaped atypia-monomorphic lumens � Round shaped lumens � Monolayer or broad papillary tufting growth � Monolayer or pattern pseudostratified growth pattern Courtesy � No mitoses of � No mitoses Dr. Stuart � Calcifications Schnitt � Calcifications Columnar Cell Columnar Cell Flat Epithelial Atypia Hyperplasia Yamashita Y, et al. Virchows Arch Change March 2016 Morphometric Analysis 7917 nuclei of 22 FEA cases 5010 nuclei of 13 CCC/CCH cases Results/Conclusions Nuclear roundness was more characteristic of FEA than CCC/CCH (statistically significant; p<0.001) Nuclear roundness was more characteristic of FEA with malignancy Courtesy of than FEA without malignancy Dr. Stuart (statistically significant; p<0.001) Schnitt 9
5/27/2016 Inv tubular ca LCIS CCL/FEA +1q -16q Tubular ca FEA Courtesy of Dr. Stuart Schnitt Abdel-Fatah T, et al AJSP 2007;31:417-426 10
5/27/2016 Recommend excisional biopsy only if flat epithelial atypia is identified p63 Juvenile Papillomatosis Rosen PP, et al. Cancer 1985;55:1345-1352 30 yrs or younger (range 12-48; mean 23) Painless and mobile mass – clinically mistaken for fibroadenoma Usually solitary, sometimes bilateral 25/180 (14%) recurrent JP Juvenile Papillomatosis Family history of breast cancer: Majority of secondary relatives (23/39; 59%) were from maternal side 11
5/27/2016 Spectrum of benign changes arranged Juvenile Papillomatosis in a localized fashion: Cysts – simple or apocrine; with luminal histiocytes Hyperplasia- ductal and apocrine with histologic merging Papillary epithelial proliferation (papillomas or papillomatosis) Sclerosis/ radial sclerosing changes Courtesy of Dr. Timothy D’Alfonso Merging of Ductal and Apocrine Hyperplasia 12
5/27/2016 Juvenile Papillomatosis and Carcinoma � Pts with carcinoma: slightly older at time of JP dx (27 yrs versus 23 yrs) and higher frequency of positive family history (56%) Lobular carcinoma in-situ (LCIS) � Management: EXBX with clear margins of Arising in Juvenile Papillomatosis JP; clinical follow up of pt and pt’s female relatives Juvenile Papillomatosis on Core Biopsy Pregnancy-like (pseudolactational) change/hyperplasia Recommend excisional biopsy with clear margins 13
5/27/2016 Pregnancy-like (pseudolactational) change 12 cases of PLH as primary dx (4- NCB; 8- EXBX) 5/12 performed for mammo calcs 4/12 mass; 1/12 “abnl mammo”; 1/12 galactorrhea 5/12 co-existing CHH Am J Surg Pathol 2000; 24(12):1670-1674 3/5 merging and with atypia 1/5 separate and PLH with atypia 1/5 separate and no atypia 4/5 with co-existing CHH also showed atypia Take home messages: Do not mistake PLH for ADH Recognize PLH and CHH can co-exist and even merge Pregnancy-like Change Pregnancy-like Hyperplasia Atypical Pregnancy-like Hyperplasia 14
5/27/2016 9 cases of DCIS (plus inv ca in 1) arising Histologically Combined PLH and CHH Lesions from PLH and CHH All women; age 35-49 years old (average 42) 6/9 performed for mammo calcs 2/9 mass; 1/9 nipple discharge 5/9 merging PLH and CHH (one or both Am J Surg Pathol 2004; 28:789-793 with atypia) DCIS: 2/9 micropapillary type, both from PLH 7/9 CHC type; 4 arising from atypical CHH; 1 also had invasive ca – well diff IFDC- 4mm with ITC in 1 SLN Take home messages: If PLH or CHH with atypia or combined PLH-CHH without atypia are identified in NCB; recommend EXBX Calcifications Atypical Pregnancy-like Hyperplasia Micropapillary DCIS Associated With Pregnancy-like (pseudolactational) Proliferations 15
5/27/2016 Secretions in Pregnancy-like change on core biopsy Pregnancy-like (pseudolactational) Proliferations Recommend excisional biopsy only if atypia or combined PLH-CHH is identified Mucocele-like lesion Mucocele-like lesions 16
5/27/2016 Secretions in Mucocele- like Lesions Calcifications Associated With Mucocele-like Lesions Pathologic upgrade rate in EXBX of benign MLL diagnosed in core biopsy Take home messages: Most MLLs today are biopsied Authors Year N total N Upgrade % excised upgrade diagnosis upgrade due to their association with Ha et al 2015 23 0 - 0 calcs Diorio et al 2015 35 2 DCIS 5.7 Even in studies with an inherent selection bias, the pathologic upgrade rate is Rakha, et al 2013 54 2 DCIS 4 low Sutton et al 2012 22 0 - 0 Recent studies suggest that Jaffer et al 2011 45 1 DCIS 2.2 not all benign MLLs need to Carkaci et al 2011 9 0 - 0 be excised 17
5/27/2016 Mucocele-like lesion in core biopsy MLLs and columnar cell lesions Recommend excisional biopsy occurring as a only if atypical ductal hyperplasia morphologic or carcinoma is identified continuum Not all benign MLLs may need to Fadare O, Mariappan MR be excised and such cases J Med Case Reports 2008; 2:138 should be managed in a multidisciplinary setting Thank You 18
Recommend
More recommend