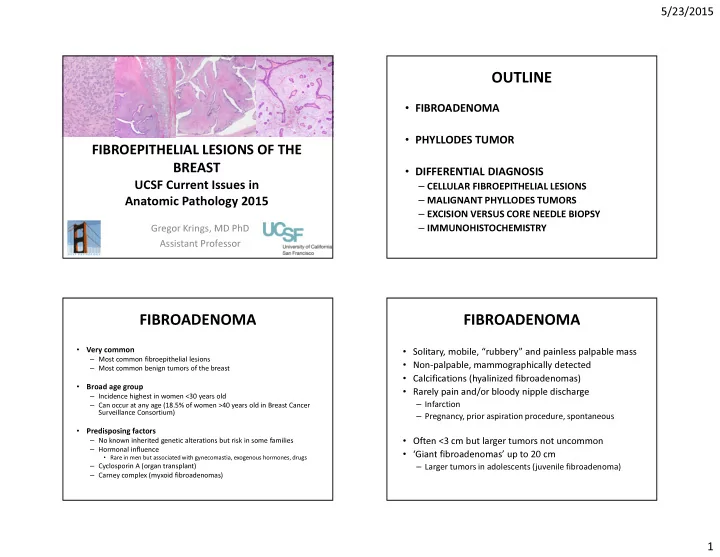
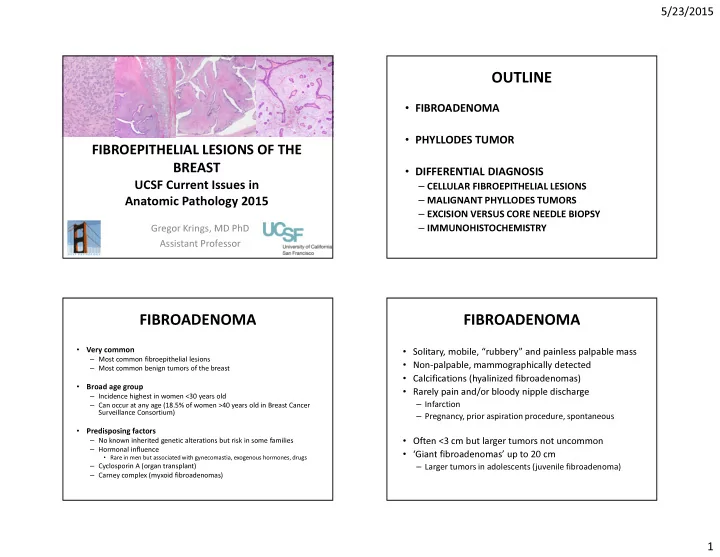
5/23/2015 OUTLINE • FIBROADENOMA • PHYLLODES TUMOR FIBROEPITHELIAL LESIONS OF THE BREAST • DIFFERENTIAL DIAGNOSIS UCSF Current Issues in – CELLULAR FIBROEPITHELIAL LESIONS – MALIGNANT PHYLLODES TUMORS Anatomic Pathology 2015 – EXCISION VERSUS CORE NEEDLE BIOPSY – IMMUNOHISTOCHEMISTRY Gregor Krings, MD PhD Assistant Professor FIBROADENOMA FIBROADENOMA • Very common • Solitary, mobile, “rubbery” and painless palpable mass – Most common fibroepithelial lesions • Non-palpable, mammographically detected – Most common benign tumors of the breast • Calcifications (hyalinized fibroadenomas) • Broad age group • Rarely pain and/or bloody nipple discharge – Incidence highest in women <30 years old – Infarction – Can occur at any age (18.5% of women >40 years old in Breast Cancer Surveillance Consortium) – Pregnancy, prior aspiration procedure, spontaneous • Predisposing factors – No known inherited genetic alterations but risk in some families • Often <3 cm but larger tumors not uncommon – Hormonal influence • ‘Giant fibroadenomas’ up to 20 cm • Rare in men but associated with gynecomastia, exogenous hormones, drugs – Cyclosporin A (organ transplant) – Larger tumors in adolescents (juvenile fibroadenoma) – Carney complex (myxoid fibroadenomas) 1
5/23/2015 Usual-type Hyalinized Intracanalicular Pericanalicular Mixed Myxoid Mixed 2
5/23/2015 Myxoid FA Mucinous carcinoma Myxoid FA Mucinous carcinoma ● Myxoid fibroadenoma may mimic invasive mucinous carcinoma ● Misdiagnosis on imaging - 16/17 myxoid fibroadenomas with rapid growth or size >3 cm misdiagnosed as mucinous carcinoma on ultrasound Yamaguchi Human Pathology 2011;42:419-423 ● Misdiagnosis on FNA and core biopsy Simsir 2001 Diagn Cytopathol. 2001;25:278-284 COMPLEX FIBROADENOMA COMPLEX FIBROADENOMA ● Sclerosing adenosis, papillary apocrine metaplasia, cysts >3mm or epithelial calcifications • Managed like typical FA in absence of atypia or rad-path discordance • We do not use this term in diagnosis Sklair-Levy M et al. AJR 2008;190(1):214-8 3
5/23/2015 CELLULAR FIBROADENOMA • Focal or diffuse mildly increased stromal cellularity without stromal atypia – No threshold criteria for defining hypercellularity – Stromal atypia is subjective • Stromal mitotic figures may be present (up to 2 MF/10 HPF typically acceptable) • Overlapping features with benign phyllodes tumors • Uniform cellularity and epithelial:stromal distribution JUVENILE FIBROADENOMA • More common in adolescents and women <20 years old • Usual-type fibroadenoma most common in all age groups • May mimic phyllodes tumor – Rapid growth, large size, histologic features • Cellular stroma with pericanalicular growth • Stromal mitotic activity may be present • No stromal cytologic atypia • Uniform cellularity and epithelial:stromal distribution • ‘Gynecomastoid’ usual ductal hyperplasia • Excision with preservation of adjacent breast 4
5/23/2015 ALH E-cadherin ● Atypia or carcinoma may involve fibroadenomas primarily or secondarily - ALH/LCIS most common - ADH/DCIS - Invasive carcinoma ALH E-cadherin PHYLLODES TUMORS • Rare <1% primary breast tumors <2.5% fibroepithelial lesions in tertiary centers • Age 40-50 years (but wide range, adolescence to 90) – 15-20 years older than FA, on average ADH Tangential – Tumors in adolescents often benign • More common in Asian and Latina women – May present at younger age in this group • Li-Fraumeni Syndrome (p53 mutations) predisposed 5
5/23/2015 PHYLLODES TUMORS PHYLLODES TUMORS • Present as mass lesion – Rapidly growing or accelerated growth of previously “fibroepithelial neoplasms, stable lesion histologically resembling intracanalicular fibroadenomas, characterized by a double- • 4-5 cm in size, but wide range (<3-20+ cm) layered epithelial component arranged in clefts – Smaller lesions increasingly detected by screening surrounded by a hypercellular stromal/mesenchymal component which in • Not reliably distinguished from fibroadenoma combination elaborate leaf-like structures” by imaging PHYLLODES TUMOR DIAGNOSIS BASED LEAF-LIKE GROWTH ON A CONSTELLATION OF FEATURES • Increased stromal cellularity* • Leaf-like growth ± periductal stromal condensation • Stromal heterogeneity • +/- mitotic activity* • +/- infiltrative border* • +/- stromal overgrowth* • +/- stromal cytologic atypia* • +/- malignant heterologous stroma* * Used to establish grade 6
5/23/2015 LEAF-LIKE GROWTH LEAF-LIKE GROWTH SUBEPITHELIAL STROMAL CONDENSATION SUBEPITHELIAL STROMAL CONDENSATION 7
5/23/2015 STROMAL HETEROGENEITY INTRALOBULAR STROMAL COMPRESSION OF FIBROADENOMA BENIGN PHYLLODES TUMOR GRADING PHYLLODES TUMORS Adapted from WHO Classification of Tumours of the Breast, 4 th ed. 2012 8
5/23/2015 MALIGNANT PHYLLODES TUMOR INFILTRATIVE BORDERS Stromal overgrowth (4x low power field) often diffuse 9
5/23/2015 MALIGNANT HETEROLOGOUS STROMA Most commonly liposarcomatous SATB2 is a useful marker of SATB2 osseous differentiation BORDERLINE PHYLLODES TUMOR SATB2 10
5/23/2015 Phyllodes tumor histologic grade FEATURES PREDICTIVE OF PHYLLODES predicts local recurrence TUMOR RECURRENCE - 605 phyllodes tumors (diagnosed over 18 years, 1992-2010) - 552 patients with clinical follow-up - 29.8/24.6 months mean/median time to recurrence ‘A.M.O.S.’ criteria Tan PH et al J Clin Pathol 2012;65:69-76 NOMOGRAM FOR PREDICTING PHYLLODES NOMOGRAM FOR PREDICTING PHYLLODES TUMOR RECURRENCE FREE SURVIVAL TUMOR RECURRENCE FREE SURVIVAL A. A. M. M. REQUIRES ADDITIONAL * Positive O. O. margin status VALIDATION IN OTHER S. best predictor S. of recurrence* POPULATIONS Tan PH et al J Clin Pathol 2012;65:69-76 Tan PH et al J Clin Pathol 2012;65:69-76 11
5/23/2015 PHYLLODES TUMOR: HISTOLOGIC GRADE AND PROGNOSIS 21/48 (43.8%) 4/48 (8.3%) initially benign benign Benign Borderline Malignant tumors recurred tumors as higher grade recurred as 2/16 (12.8%) malignant initially borderline Local recurrence* 4-17% 14-25% 23-30% tumors recurred as malignant Tan PH et al J Clin Pathol 2012;65:69-76 * Margin status remains the best predictor of local recurrence ● Other studies with similar results Hart WR et al. Am J Clin Pathol 1978;70(2):211-6 Moffat CJ et al. Histopathology 1995;27(3):205-18 - 6-19% benign tumors reported to recur as malignant De Roos WK et al. British J Surg 1999;86(3):396-9 Tan PH et al. J Clin Pathol 2012;65:69-76 Barth RJ Jr. Breast Cancer Res Treat 1999;57(3):291-5 ● Highlights importance of preventing local tumor recurrence Kim S et al. Breast Cancer Res Treat 2013 141;353-363 WHO 2012 DISTANT PHYLLODES TUMOR METASTASIS PHYLLODES TUMOR: • Stromal overgrowth and malignant HISTOLOGIC GRADE AND PROGNOSIS heterologous stromal elements are best predictors of distant spread Benign Borderline Malignant • Metastasis essentially always stromal % of phyllodes 65-70% 15-20% 10-20% component only Metastasis** (<10% overall) 0% 0-4% 13-29% • Lung/pleura (>75%) and skeletal system most ** Essentially only malignant tumors metastasize common sites Tan PH et al. J Clin Pathol 2012 65(1):69-76 Kim S et al. Breast Cancer Res Treat 2013 141;353-363 WHO 2012 12
5/23/2015 Lung Vulva PHYLLODES TUMOR TREATMENT • Excision with negative margins to minimize recurrence risk – 1 cm normal rim preferable (but no data to support this arbitrary margin width) – Rationale • Margin status primary predictor of recurrence • Recurrences may be of higher grade • Metastatic tumors may be preceded by local recurrences • No routine role for radiation or chemotherapy DIFFERENTIAL DIAGNOSIS OF Benign phyllodes Fibroadenoma FIBROEPITHELIAL LESIONS Mean age ~45-50 (but any age) ~30 y (but any age) OVERLAP Few cm up to 20 cm <3 cm; rarely up to 20 cm Size OVERLAP benign borderline malignant Growth May be rapid; rapid growth of previously Stable stable mass NOT RELIABLE Clinical and radiologic features do not reliably distinguish between phyllodes tumor and fibroadenoma MAY BE PROBLEMATIC IN Jacobs et al Am J Clin Pathol. 2005 Sep;124(3):342-54 EXCISIONS AND CORE BIOPSIES WHO 2012 13
5/23/2015 BENIGN FIBROADENOMA PHYLLODES CELLULAR FIBROADENOMA BENIGN PHYLLODES TUMOR Present, well-developed Leaf-like architecture Usually absent, may be focal ± periductal condensation Stromal heterogeneity May be present Absent Distribution of epithelium and stroma Often non-uniform Uniform Hypocellular or Stromal cellularity Mild Mild (*cellular and juvenile fibroadenoma) Rare-up to 2/10 HPF allowed Stromal mitoses Few (0-4/10 HPF) (*cellular and juvenile fibroadenoma) Cellular atypia Mild Absent (*stromal giant cells) Squamous metaplasia Rarely present Virtually absent BENIGN FIBROADENOMA PHYLLODES Present, well-developed Leaf-like architecture Usually absent, may be focal ± periductal condensation Stromal heterogeneity May be present Absent Distribution of epithelium and stroma Often non-uniform Uniform Hypocellular or Stromal cellularity Mild Mild (*cellular and juvenile fibroadenoma) Rare-up to 2/10 HPF allowed Stromal mitoses Few (0-4/10 HPF) (*cellular and juvenile fibroadenoma) Cellular atypia Mild Absent (*stromal giant cells) Squamous metaplasia Rarely present Virtually absent 14
Recommend
More recommend