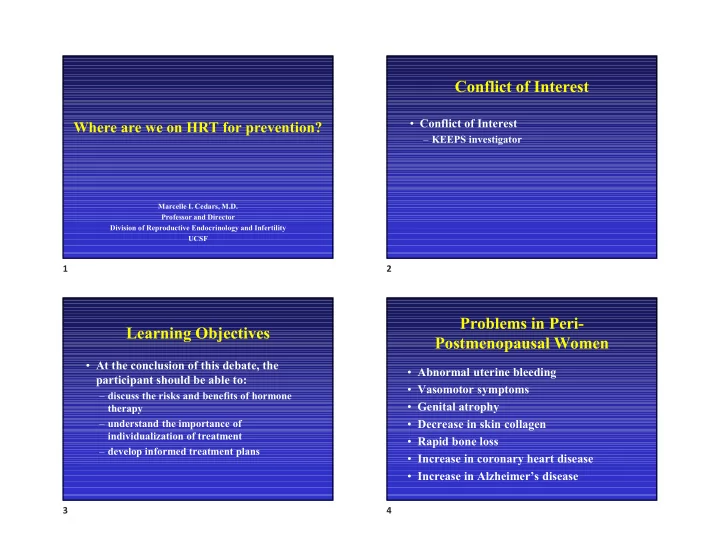
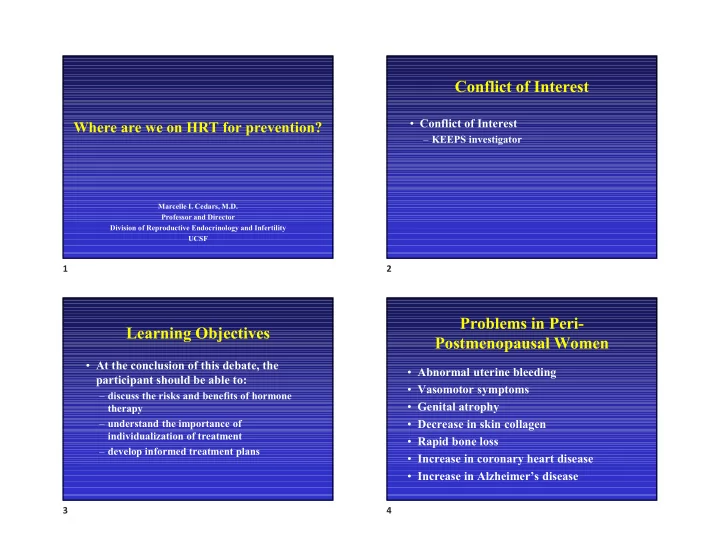
10/18/2019 Conflict of Interest • Conflict of Interest Where are we on HRT for prevention? – KEEPS investigator Marcelle I. Cedars, M.D. Professor and Director Division of Reproductive Endocrinology and Infertility UCSF 1 2 Problems in Peri- Learning Objectives Postmenopausal Women • At the conclusion of this debate, the • Abnormal uterine bleeding participant should be able to: • Vasomotor symptoms – discuss the risks and benefits of hormone • Genital atrophy therapy • Decrease in skin collagen – understand the importance of individualization of treatment • Rapid bone loss – develop informed treatment plans • Increase in coronary heart disease • Increase in Alzheimer’s disease 3 4 1
10/18/2019 1995 PEPI trial 2015 1966 ELITE “Feminine Forever” 1992 – American College of Physicians Recommends MHT to prevent CHD Menopausal Hormone Therapy (MHT) over the decades 1980’s – cohort and case/control Studies – support MHT reduces CHD and osteoporosis 2002 WHI – E+P2004 1998 HERS WHI - ERT 5 6 WHI vs. Observational studies HRT for Prevention A. HRT should be used for 53% prevention in all women 32% B. HRT should be used for prevention in young women 15% C. HRT should not be used for prevention . . . . . f . . . d r r o o e s f f u d d e e e s s b u u t e e o b b n d d d l l l u u u o o o h h h s s s T T T R R R H H H Manson JE, et al. 2006; 13:139 7 8 2
10/18/2019 Early vs Late Intervention Patient Characteristics: Age the “timing” hypothesis Trial with Estrogen (ELITE) • Grodstein et al. J Womens Health 2006 – Nurse’s Health Study: evaluating time from menopause – women near menopause reduced CV risk (RR 0.66 CI: 0.54-0.80) • Manson et al. NEJM 2007 – WHI: coronary calcium – women 50-59, coronary calcium score lower in women on ET vs. placebo (OR 0.69 CI: 0.48-0.98) • ELITE Trial – Hodus HN 2015 Hodis H, NEJM 2016 – Protection from CIMT changes in younger women 9 10 Estrogen and the Brain Estrogen and the Brain Alzheimer Disease • Direct effects – Enhances synaptic plasticity, neurite growth, • Observational studies suggest protection hippocampal neurogenesis and long-term • Meta-analyses suggest risk reduction of potentiation (memory) approximately 1/3 – Protects against apoptosis and neural injury • Contradicted by the WHIMS trial (ages 65-79) – Stimulates aceytlcholine (memory), serotonin, noradrenalin – Risk of dementia increased two-fold with combined HRT – Decrease deposition of b -amyloid – Impact noted within a few years, suggesting impact – Promotes morphological and electrophysiological primarily on the vasculature correlates of learning and memory – Past history of use associated with lowered incident • Indirect effects risk of dementia (including Alzheimer Disease) – Vasculature • Initiation in older women WITH disease is not – Immune system beneficial NIA – Frontiers proposal – Bench to Bedside Estrogen as a case-study (2009) 11 12 3
10/18/2019 Verbal Memory Estrogen and the Brain Decrement in • Estrogen effect on memory immediate (A) • Estrogen effect on mood and delayed (B) verbal recall • Estrogen effect on stress and cognition – Reduction in cortisol response to stress – Reduction in effect of stress to reduce Epperson JCEM working memory 2013 13 14 Early effects of estrogen Estrogen and the Brain • Girard: Scientific Reports 2017 • Alzheimer Disease • Neurocognitive function – Early and consistent symptom – loss of episodic memory (failing to recall – Cognitive control; mental set shifting appointments and events) – Response to environmental context – In the laboratory: estrogen reduces the • Functional MRI formation of b -amyloid formation and – Prefrontal functions diminishes hyperphosphorylation of tau – Cognitive flexibility protein • Method to identify effect (pre-behavioral) 15 16 4
10/18/2019 Age-stratified Risk for Estrogen effect on verbal recall Alzheimer Disease OR Adjusted OR Entire Sample (age 50-99) HRT 0.47 0.70 (0.35-0.63) (0.51-0.95) Ages 50-63 HRT 0.35 0.35 (0.19-0.64) (0.19-0.66) Joffe, H Henderson VW Menopause 2006 Ages 64-71 MIRAGE 2005 HRT 0.65 0.86 (0.39-1.1) (0.5-1.5) 17 18 Amyloid Deposition Cognition and Estrogen • No risk with early exposure – KEEPS – ELITE – WHIMSY Kantarci J J Alzheimer Disease 2016 19 20 5
10/18/2019 The “Menopausal Syndrome” Trouble Sleeping by Cycle Day • Epidemiological Studies: proximity to menopause, not associated with aging, relieved with estrogen – Vasomotor Symptoms – Vaginal dryness/dyspareunia – Difficulty sleeping/insomnia – Mood and depression – Changes in cognitive function Kravitz, H. M. et al. Arch Intern Med 21 22 Duration of VMS Hot Flashes worsen Sleep • 20 healthy premenopausal women receiving GnRHa • 80% concordance between subjective/objective VMS (sVMS/oVMS) • Sleep efficiency (actigraphy) worse with oVMS, quality worse with sVMS (questionnaire) Joffe H, Menopause 2013 PMID 23481119 Avis, NE: JAMA Int Med 2015 23 24 6
10/18/2019 Adjusted OR for CES-D > 16 Estradiol and Depressive Disorders Across Menopausal Transition (Soares et al., Arch Gen Psychiatry 2001;58:529) • 50 perimenopausal women aged 40-55 with irregular menstrual periods and FSH > 25 IU/L meeting Pre Early Peri Late Peri Post HT Users criteria for major depressive, dysthymic, or minor depressive disorder by DSM-IV blindly randomized 1.8 1.6 to transdermal estradiol (0.1 mg) or placebo for 12 1.4 wks 1.2 • Remission of depression observed in 17 of 25 (68%) 1 on E 2 and 5% on placebo 0.8 0.6 • Regardless of DSM-IV diagnosis, subjects responded 0.4 similarly to E 2 0.2 0 Bromberger, J Affect Disord 2007 25 26 Estrogen for Depression Breast Cancer Prevention Risk Factors • Low body weight • High mammographic breast density Gordon, J JAMA Psychiatry • Late menopause 2018 27 28 7
10/18/2019 Cumulative Breast Cancer Severity of Cancer by Treatment Group Mortality in WHI Women Taking in WHI Women with Breast Cancer E +P vs. Placebo 80 p = 0.51 Percent of Breast Cancers Tested 2.6 70 vs. E + P 1.3 Placebo deaths per 10,000 60 women per year 193/260 232/332 50 Cumulative Breast Cancer Mortality in WHI Women Taking E +P vs. Placebo 40 30 p = 0.03 p = 0.07 20 81/341 91/379 43/263 10 53/291 0 With Positive Nodes SEER Stage R or D Not well Differentiated Severity Adapted from: Chlebowski RT, et al. JAMA 2010;304:1684 Chlebowski RT, et al. JAMA 2010;304:1684 29 30 Breast Cancer Breast Cancer Risk Factors The ‘Gap’ Hypothesis • Was there truly a “protective” effect of • Starting estrogen remote from menopause estrogen in the E-only arm – WHI? decreases risk while treatment within 2 years increases breast cancer risk • Estrogen • The ‘gap hypothesis’ and the ‘timing – Role of estrogen deprivation hypothesis’ are thus in conflict • Whether natural or via anti-estrogens (tamoxifen/aromatase inhibitors) – Estrogen as a pro-apoptotic 31 32 8
10/18/2019 Breast Cancer Role of Progestational Agents Risk Factors • Gompel, Climacteric 2018 • Low body weight – Estrogen alone lowest risk • High mammographic breast density • Not indicated with uterus in situ • Late menopause – Synthetic progestins higher risk • Starting close to menopause • Higher affinity for glucocorticoid receptor • Also androgen receptor and mineralocorticoid – Natural progesterone risk lowest • 2 years after stopping HRT – risk equivalent to never users 33 34 WHI E+P: During Study and U.S Preventative Task Force Follow-up: Mortality Gartlehner, JAMA 2017 Gross D, JAMA 2017 Modified from Heiss et al. JAMA 2008;299:1036-45 35 36 9
10/18/2019 Danish Osteoporosis DOPS - 2012 Prevention Study (DOPS) • 1006 women • Randomized 45-58 years, last vaginal bleeding 3-24 months prior to enrollment and increased FSH • Randomized, open-label, trial of estrogen (2mg daily), triphasic estradiol + norethisterone (uterus) vs. no treatment Schierbeck LL, BMJ 2012 Schierbeck LL, BMJ 2012 37 38 Menopausal Hormone Therapy Long-term risk/benefit Good Prevention Strategy Mikkola TS. Menopause 2015 • Rise in mortality for women - increased 44% compared with 3% for men since 2002 • Only other preventative strategy - lifestyle 39 40 10
10/18/2019 Menopausal Hormone Therapy Menopausal Hormone Therapy Good Prevention Strategy Good Prevention Strategy • Prevention of cardiovascular disease • Absolute risks • Prevention of osteoporosis and fractures – Breast cancer: 5-8/10,000 women years • Reduction in new onset diabetes – Venous thrombosis: 5/10,000 women years • Use of non-oral eliminates risk • Reduction in dementia • Reduction in all-cause mortality • Improved quality of life 41 42 Modified from Heiss et al. JAMA Endocrine Society 2010 2008;299:1036-45 Study Oral Transdermal Publication Estrogen Estrogen Scarabin, et al (1) 3.5 0.9 (1.8-6.8) (0.5-1.6) Canonico, et al (2) 4.2 0.9 (1.5-11.6) (0.4-2.1) 1.Lancet, 2003,362: 428-3 2. Circulation, 2007,115: 840-845 43 44 11
Recommend
More recommend