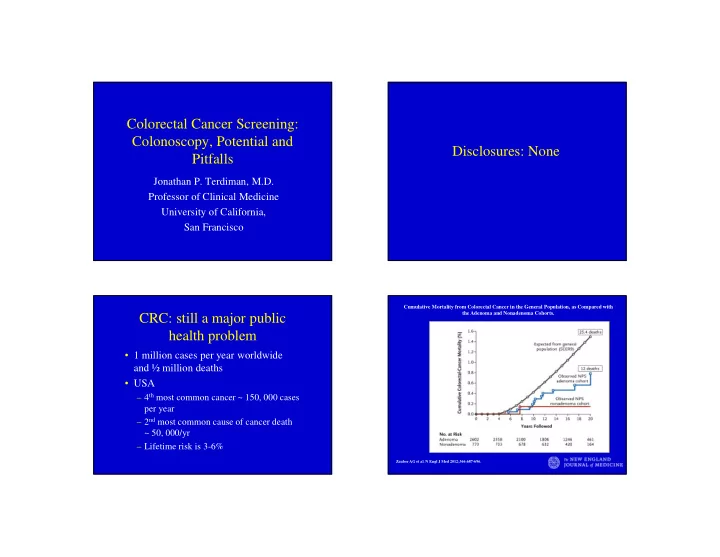
Colorectal Cancer Screening: Colonoscopy, Potential and Disclosures: None Pitfalls Jonathan P. Terdiman, M.D. Professor of Clinical Medicine University of California, San Francisco Cumulative Mortality from Colorectal Cancer in the General Population, as Compared with the Adenoma and Nonadenoma Cohorts. CRC: still a major public health problem • 1 million cases per year worldwide and ½ million deaths • USA – 4 th most common cancer ~ 150, 000 cases per year – 2 nd most common cause of cancer death ~ 50, 000/yr – Lifetime risk is 3-6% Zauber AG et al. N Engl J Med 2012;366:687-696.
Screening Colonoscopy Screening Options • FOBT q year • Compelling indirect evidence that this is the “best” test • Flexible sigmoidoscopy q 5 yrs – FOBT studies • FOBT and Flexible sigmoidoscopy – Flex Sig Studies • Colonoscopy q 10 years – Polypectomy Studies • CT colonography q 5 years – Cohort studies Screening Colonoscopy: VA Colonoscopy in the real world: The Cooperative Study Polyp Prevention Trials (Lieberman et al. NEJM, 2000) • 9 studies with > 20, 000 years of • Advanced adenoma in 7.9% patient follow-up • Cancer in 1.0% • Incidence of CRC = 1.7-2.4/1, 000 – 73% with Stage I or II disease person-years – 20% with Stage III and 6% with Stage IV • Incidence is equivalent to general • 44% of patients with advanced neoplasia would have been missed by population and 4 x that in National flex sig first screen Polyp Study!!! • 30% missed by sig + FOBT Gastroenterology 2005;129:34-41 Gastrointest Endosc 2005;61:385-91
Impact of colonoscopy on CRC Incomplete Exam death Gastro, 2007 Baxter NN . Ann Int Med, 2009 • Pop-based study in Canada • 10, 292 CRC deaths and 51, 940 • > 300, 000 exams, 13% incomplete controls among 1.2 million Canadians, • Risk Factors 1996-2001 – Older age • OR for death with colonoscopy = 0.69 – Women – Left sided cancers, OR = 0.33 – Prior operation – Right sided cancer, OR = 0.99 – Test in MD office AN: Left vs. Right Polyps Missed Cancers Gupta S, et al. Clinical Gastroenterology and Hepatology 2012; 10:1395-1401. Gastro, 2007 • Cancers diagnosed within 3 yrs of colonoscopy • Risk Factors – Older age – Diverticular disease – Right sided cancer – Internist/Family MD doing the test – Test in a MD office
Flat & Depressed Polyps Incomplete Polyp Resection Soetikno R, Jama 2008 Pohl H, Gastroenterology 2012 • 1819 exams, use of dye spray to confirm • Prevalence = 9.4% (95% CI, 8.1-10.8) • Prospective study of 1427 patients • OR for cancer = 9.8 who underwent colonoscopy • 10% inadequately resected • Wide range by MD (6.5-23%) • Risk Factors – Large size: 17% for > 10 mm – Serrated polyps: 31% – Less than 20 polypectomies/year Advanced Polypectomy Biological Variability Holt BA, Clin Gastro Hepatol, 2012 • 51 interval cancers – within 5 years of colonoscopy • MSI in 30.4% of interval cancers versus 10.3% of others (p = 0.003) – Interval cancers 3.7 x more likely to be MSI • 27% of interval cancers at previous polypectomy segment • Interval cancers 3 times more likely to be R sided Farrar WD Gastro, 2006 Sawhney MS Clin Gastro Hepatol, 2006
Mean adenoma detection rate according Doing colonoscopy well to colonoscopic withdrawal times Barclay RL NEJM, 2007 • 12 endoscopists doing over 2000 screening exams • Range of adenoma detection – 9.4% to 32.7% • Range of scope withdrawal times – 3.1 to 16.8 minutes • Detection rate < versus > 6 minutes – 11.8% versus 28.3% for any adenoma (p < 0.001) – 2.6% versus 6.4% for advanced adenoma (p = 0.005) Benchmarks for GOOD Cumulative Hazard Rates for Interval Colorectal Cancer, According to the Endoscopist's Adenoma Detection Rate (ADR). Colonoscopy • Adenoma Detection Rate – > 25% men, 15% women – PLCO data: 2.4 fold risk of interval cancer in those with lowest quartile of ADR vs. highest • Documentation of Prep – 100% • Cecal Intubation – >/= 95% – Recent population-based study in Canada rate was only 87% • Withdrawal Times – >/= 6 minutes? Kaminski MF et al. N Engl J Med 2010;362:1795-1803.
Colonoscopy done well Brenner, Ann Int Med, 2011 • Population-based case-control study in Germany • 1688 CRC cases and 1932 controls • Colonoscopy within 10 years – 77% risk reduction for CRC – 84% for left-sided cancer – 66% for right-sided
Recommend
More recommend