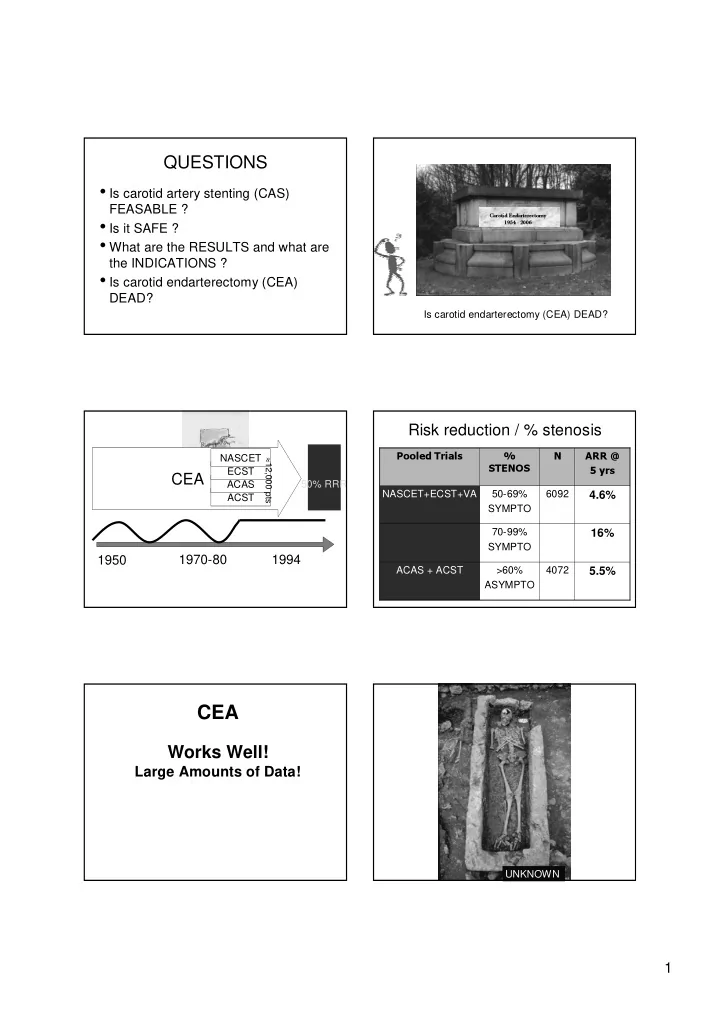
QUESTIONS • Is carotid artery stenting (CAS) FEASABLE ? Carotid Endarterectomy • Is it SAFE ? 1954 - 2006 • What are the RESULTS and what are the INDICATIONS ? • Is carotid endarterectomy (CEA) DEAD? Is carotid endarterectomy (CEA) DEAD? Risk reduction / % stenosis NASCET Pooled Trials % N ARR @ ≈ 12,000 pts ECST STENOS 5 yrs CEA ACAS 50% RRR NASCET+ECST+VA 50-69% 6092 4.6% ACST SYMPTO 70-99% 16% SYMPTO 1950 1970-80 1994 ACAS + ACST >60% 4072 5.5% ASYMPTO CEA Works Well! Large Amounts of Data! UNKNOWN 1
NASCET ECST CEA ACAS Le Roi STENT ACST 1950 1970-80 1994 C Angioplasty 2000 E CAS P D 1 Stent Eradicates 10.000 Vascular Surgeons LE TRONE DU STENT CAROTIDIEN Literature Review CAS IS IT FEASABLE ? IS IT SAFE ? 2
s Literature Review Leicester 1998, UK g i s n y r i l a o n t i a n o m m i r e a t t n • Leicester a i 29 patients, ∑ >70% • SAPPHIRE d t s y r b i f F/U 1 mo d e • Wall stent e h • Non-randomized p t p t a Stroke/Death/HITs D30 o t e S • Kentucky e case series t t i m m • CAVATAS o • CREST c • Non-randomized 6 excluded • ICSS On – going TRIALS case series • EVA – 3s • SPACE Endovacular Surgery BEFORE EPD AFTER EPD 5/7 strokes JVS 1998 Abandoned by commercial sponsors Wallstent 2001, USA Wallstent 2001 219 pts, ∑ >60% • No protection devices used F/U 1,12 mo • Lack of experience of interventionalists Stroke/Death/MI D30 • Stent primarily not dedicated to carotid artery No protection devices • Stroke and MI rates > CEA group Ticlopidine • Prematurely arrested • Abandoned by commercial sponsors Endovascular Surgery < 12.1% (1 yr) 3.6% (1 yr) CAVATAS 2001 Kentucky 2001, USA Europe, Australia, Canada Clopidogrel 104 patients, ∑ >70% 504 patients, ∑ /a ∑ F/U 1,6,12,60 mo F/U 1,3,6,12,24 mo Stroke / Death D30 Stroke/Death/Restenosis Recruitement 1992-1997 Not the best No protection devices current clinical Limited series Pre 1994 (74%) practice Post 1994 (26%) Endovacular Surgery = Endovacular Surgery 1/53 TIA 1/53 MI 251 253 JACC 2001 Lancet 2001 3
Kastrup, Stroke 2003 Interv Cardiovasc Catheter 2000 STROKE & DEATH Interv Cardiovasc Catheter 2000 Embolic Protection Device EPD Kastrup, Stroke 2003 4
Embolic protection methods FilterWire EX/EZ Carotid WallStent = 3.7% = 0.5% = 1.1% = 0.3% = 0.8% = 0.8% = 5.5% = 1.1% Kastrup, Stroke 2003 Interv Cardiovasc Catheter 2006 Literature Review • Leicester • SAPPHIRE • Wall stent • Non-randomized • Kentucky case series • CAVATAS • CREST • Non-randomized • ICSS On – going TRIALS case series • EVA – 3s • SPACE BEFORE EPD AFTER EPD Heart 2003 ALKK CAS registry hospitals • 28 centres • 7/1996-5/2004 • 1888 pts Z Cardiol 2005 Z Cardiol 2005 5
Short-Term Death/Stroke rate (%) Impact of EPDs 10 9 7,6 8 « Embolic protection should be considered 6,3 7 the standard of care in carotid stenting. 5,6 6 4,9 4,7 When use of an EPD is precluded by 5 anatomic factors, alternative treatment 4 3,2 2,9 strategies (CEA or medical therapy) must 3 2 1,9 be strongly considered » 2 1 0 1996 1997 1998 1999 2000 2001 2002 2003 2004 Roubin, Circulation 2006 Z Cardiol 2005 CAROTID ARTERY STENTING Results / indications CAS vs CEA Distal protection Simplicity Feasibility ? WHAT ARE THE RESULTS ? CAS vs CEA WHAT ARE THE RESULTS ? 6
GUIDELINES for CEA Surgeon INDICATION LEVEL SYMPTOMATIC ASYMPTOMATIC PROVEN 70 -99 % > 60 % RISK < 6 % RISK < 3 % Life expectancy > 5 y ACCEPTABLE 50 -69 % > 60 % RISK < 3 % RISK < 3 % Planned CABG UNACCEPTABLE < 29 % < 60 % OR OR RISK > 5 % RISK > 6 % No CABG Endarterectomy Kit Stroke Council, AHA, Stroke 1998 CAS vs CEA SAPPHIRE 2002, USA RESULTS IN SUBGROUPS • 747 pts • SYMPTOMATIC PATIENTS • ∑ > 50% stenosis, • ASYMPTOMATIC PATIENTS • a ∑ > 80% stenosis • MODERATE CAROTID STENOSIS • F/U 1,12 mo • SEVERE CAROTID STENOSIS • Stroke/Death/MI D30 • HIGH SURGICAL RISK • HIGH SURGICAL RISK NEJM 2004 Criteria for high risk Criteria for high risk • Age >80 yr • Contralateral carotid occlusion • Previous radical neck surgery or • Clinically significant cardiac radiation therapy to the neck disease • Recurrent stenosis after –(CHF, abnormal stress test, or endarterectomy need for CABG) • High lesions behind the mandible • Severe COPD • Low lesions requiring thoracic exposure NEJM 2004 NEJM 2004 7
SAPPHIRE 2002, USA SAPPHIRE 2002, USA 747 pts High Surgical Risk CAS = 87.8% 406 Excluded CEA = 79.9% Not suitable for stenting Endovascular Surgery = 20/167 32/167 NEJM 2004 NEJM 2004 CAS vs CEA CAS vs CEA RESULTS IN SUBGROUPS RESULTS IN SUBGROUPS • SYMPTOMATIC PATIENTS • SYMPTOMATIC PATIENTS ? • ASYMPTOMATIC PATIENTS • ASYMPTOMATIC PATIENTS • HIGH SURGICAL RISK • HIGH SURGICAL RISK • MODERATE CAROTID STENOSIS • MODERATE CAROTID STENOSIS • SEVERE CAROTID STENOSIS • SEVERE CAROTID STENOSIS ! ! CREST 2004, USA EVA-3S 2004, France ! ! E T I D ) I r B e s R 2500 patients, ∑ >50% s 1000 pts, ∑ O u M o F/U 1 mo B F/U 1,24-48 mo E G D Stroke/Death/Restenosis Stroke/Death/MI D30 M S r E u C e s X s E e f Recruitement 2000 R Recruitement 2000 o Clopidogrel/ U r P O 454 randomized pts 452 randomized pts e P Ticlopidine l R e m E T a E d a R M R ( A Endovacular + Surgery Endovacular Surgery Cerebral protection JVS 2004 Stroke 2004 8
ICSS 2004 (= CAVATAS-2), UK SPACE 2001, Germany 1900 pts, ∑ >70% 1500 pts, ∑ >70% F/U 1 mo F/U 1 mo Stroke/Death D30 Stroke/Death/MI D30 Restenosis 24 mo Recruitement 2001 Recruitement 2002 > 600 so far 970 pts Endovacular Endovacular Surgery Surgery ± CP ± CP Cerebrovasc Dis 2004 Cerebrovasc Dis 2004 Je n’ai plus de Literature Review Données! Nous sommes • Leicester • SAPPHIRE perdus!!! • Wall stent • Non-randomized • Kentucky case series • CAVATAS • CREST • Non-randomized • ICSS On – going TRIALS case series • EVA – 3s • SPACE BEFORE EPD AFTER EPD CAS or CEA Carotid Revascularization 1. Available data (one trial) show Indicated that CAS is superior to CEA in selected high risk patients. CEA Risk 2. In all other patient groups no data is currently available to High Low answer this question CEA CAS CEA vs CAS Trial 9
CAS: Contradications Carotid Revascularization Indicated • Intolerance to antiplatelet agents. • Major surgery within 3 to 4 weeks that will require cessation of antiplatelet therapy Yes CEA Risk • Contrast nephropathy (< 75 mL of contrast) High Low • Intracranial arterial stenoses Relative • arteriovenous malformations ? CEA CAS • Stable aneurysms CEA vs CAS Trial Roubin, Circulation 2006 Increased Procedural Risks CAS: Contradications After CAS Risk Factor Features • Specific angiographic findings Clinical Advanced age Age > 80 y Decreased Dementia – excessive tortuosity Cerebral Prior (remote) stroke – massive calcifications reserve Multiple lacunar infarcts Intracranial microangiopathy circumrferencial 2 90 o bends within 5 cm of Angiographic Excessive tortuosity the lesion –Thrombus burden Heavy Concentric, circumferential, calcification Width 3 mm Roubin, Circulation 2006 Age & risk of Stroke / Death Age strata N Events (%) OR (95% CI) Impact of age on risk of stroke <60 120 2 (1.7%) 1.0 and death D30 60-69 229 3 (1.3%) 0.78 (0.13-4.75) CREST lead-in phase 70-79 301 16 (5.3%) 3.31 (0.75-14.63) 80+ 99 12 (12.1%) 8.14 (1.78-37.30 CREST lead-in phase, JVS 2004 10
Increased Procedural Risks Excessive tortuosity After CAS • Difficulty of access Risk Factor Features • Failure of device delivery Clinical Advanced age Age > 80 y • Prevent EPD positioning Decreased Dementia • Unsufficient “landing zone” Cerebral Prior (remote) stroke • Atheroembolism reserve Multiple lacunar infarcts • Air embolism Intracranial microangiopathy • Excessive contrast 2 90 o bends within 5 cm of Angiographic Excessive tortuosity the lesion • Bifurcation plaque disruption Heavy Concentric, circumferential, • ICA dissection calcification Width 3 mm Increased Procedural Risks After CAS Risk Factor Features Clinical Advanced age Age > 80 y Decreased Dementia Cerebral Prior (remote) stroke reserve Multiple lacunar infarcts Intracranial microangiopathy 2 90 o bends within 5 cm of Angiographic Excessive tortuosity the lesion Before After Heavy Concentric, circumferential, calcification Width 3 mm Carotid Plaque Calcifications Revascularization Difficulty in CEA Risk • Tracking devices Low High • Lesion dilation CEA Consider CAS • Stent positioning CEA vs CAS Trial • Achieving adequate expansion Risk for CAS Low High Low CEA or CAS Medical Therapy 11
Pourriez– vous répéter votre topo SVP Car je ne faisais pas attention Angiographic Restenosis RESTENOSIS • 2167 pts CAS (stenting rate 95%) • 5-year follow-up • 85% of pts alive & free from ipsilateral stroke • Restenosis rate 4%. Gray, STROKE 2002 Bosier, J Cardiovasc Surg (Torino) 2005 12
Recommend
More recommend