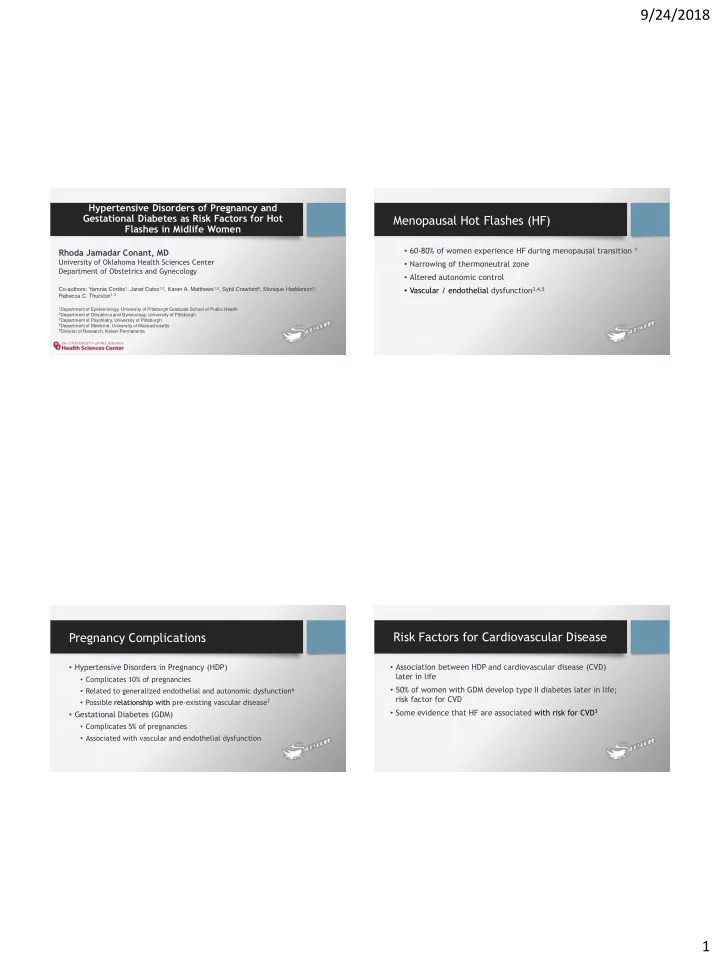
9/24/2018 Hypertensive Disorders of Pregnancy and Gestational Diabetes as Risk Factors for Hot Menopausal Hot Flashes (HF) Flashes in Midlife Women • 60-80% of women experience HF during menopausal transition 1 Rhoda Jamadar Conant, MD University of Oklahoma Health Sciences Center • Narrowing of thermoneutral zone Department of Obstetrics and Gynecology • Altered autonomic control • Vascular / endothelial dysfunction 3,4,5 Co-authors: Yamnia Cortés 1 , Janet Catov 1,2 , Karen A. Matthews 1,3 , Sybil Crawford 4 , Monique Hedderson 5 , Rebecca C. Thurston 1,3 1 Department of Epidemiology, University of Pittsburgh Graduate School of Public Health 2 Department of Obstetrics and Gynecology, University of Pittsburgh 3 Department of Psychiatry, University of Pittsburgh 4 Department of Medicine, University of Massachusetts 5 Division of Research, Kaiser Permanente Pregnancy Complications Risk Factors for Cardiovascular Disease • Hypertensive Disorders in Pregnancy (HDP) • Association between HDP and cardiovascular disease (CVD) later in life • Complicates 10% of pregnancies • 50% of women with GDM develop type II diabetes later in life; • Related to generalized endothelial and autonomic dysfunction 6 risk factor for CVD • Possible relationship with pre-existing vascular disease 7 • Some evidence that HF are associated with risk for CVD 3 • Gestational Diabetes (GDM) • Complicates 5% of pregnancies • Associated with vascular and endothelial dysfunction 1
9/24/2018 Study Purpose and Hypothesis Study of Women’s Health Across the Nation To examine the relationship between women with a history of HDP Boston,MA = Black and/or GDM and HF in midlife. Detroit, MI = Hispanic Newar ark, NJ Chicag ago, IL Oakland, CA = Chinese Pittsb sburgh,PA PA • Hypothesis 1: Women with a history of HDP and/or GDM may = Japanese experience a greater number of HF Los Angeles, s, CA • Hypothesis 2: Nulliparous women may have fewer HF Multi-site, multi-ethnic, longitudinal study of the natural history of the menopause transition. Study of Women’s Health Across the Nation Methods • Longitudinal analysis, 13 visits over 15 years • Pregnancy Questionnaire (Visit 13): • Inclusion criteria (baseline) • Preeclampsia/toxemia (high blood pressure and proteinuria), gestational hypertension or pregnancy induced hypertension, • Age 42-52 years gestational diabetes (no diabetes pre-pregnancy) • Pre or early perimenopausal • HF (at each visit): • Intact uterus and at least one ovary • Were recorded as any vs none; 0 days, 1-5 days, 6+ days in past two • Menstrual bleeding in past 3 months and no hormone therapy weeks NULLIPAROUS NO HDP/GDM HDP/GDM 2
9/24/2018 3 Groups Statistical Methods • ANOVA or Kruskal-Wallis tests for continuous data and Chi-Square or Fisher's Exact for categorical variables Nulliparous HDP/GDM No HDP/GDM n= 395 (17.6%) n= 208 (9.2%) n= 1646 (73.2%) • Visits with HT use excluded • Pregnancy history examined in relation to HF using generalized estimating equations adjusting for: HDP only GDM only Both GDM/HDP • Model 1: age (time-varying) n=176 (85%) n=27 (13%) n=27 (2%) • Model 2: study site, race/ethnicity, financial strain, education • Model 3: menopause status (time-varying) Table 1. Participant Characteristics at SWAN Visit 13 (n=2249) Nulliparous No HPD/GDM HPD/GDM P Table 2. Odds of reporting any hot flashes in past 2 weeks across SWAN visits by pregnancy history (n=395) (n=1646) (n=208) Model 1 P Model 2 a P Model 3 a P OR (95% CI) OR (95% CI) OR (95% CI) Age, Mean ± SD 61.6 ± 2.6 62.1 ± 2.7 61.4 ± 2.4 <0.0001 Nulliparous 0.81 (0.71, 0.92) 0.002 0.96 (0.80, 1.14) 0.62 0.96 (0.79, 1.16) 0.66 Race/Ethnicity, n (%) (n=2112) <0.0001 White 262 (67.0) 714 (44.2) 95 (46.3) Black 55 (14.1) 461 (28.5) 76 (37.1) No HDP/GDM Reference -- -- -- -- -- Hispanic 7 (1.8) 102 (6.3) 10 (4.9) Chinese/Japanese 67 (17.1) 339 (21.0) 24 (11.7) HDP/GDM 1.20 (1.01, 1.42) 0.04 1.06 (0.86, 1.30) 0.61 1.03 (0.82, 1.30) 0.82 262 (67.5) 665 (41.5) 88 (43.1) <0.0001 Education, n (%) (n=2194) College degree/post college • Nulliparous women had a lower odds of reporting any HF 28.7 ± 7.3 29.1 ± 7.4 32.5 ± 7.0 <0.0001 Body mass index (kg/m 2 ), Mean ± SD • HDP/GDM had a greater odds of any HF HOMA-IR, Median [IQR] 2.0 [1.2, 3.3] 2.2 [1.3, 3.8] 2.9 [1.8, 4.7] 0.0009 Anti-hypertensive, n (%) (n=2223) 150 (38.2) 735 (45.3) 123 (59.7) <0.0001 Model 1: age (time-varying) Lipid-lowering medications, n (%) (n=2248) 104 (26.3) 471 (28.6) 83 (39.9) 0.001 HPD = hypertensive pregnancy disorder Model 2: study site, race/ethnicity, financial strain, education GDM = gestational diabetes Anti-diabetics, n(%) (n=2198) 52 (13.4) 239 (14.9) 51 (25.0) 0.0004 Model 3: menopause status (time-varying) 3
9/24/2018 Table 3. Odds of being in higher hot flash frequency categories in past 2 weeks and pregnancy history Conclusions Model 2 a Model 3 a Model 1 P P P OR (95% CI) OR (95% CI) OR (95% CI) Nulliparous 0.83 (0.73, 0.95) 0.008 1.00 (0.84, 1.19) 0.97 1.02 (0.84, 1.24) 0.83 No HPD/GDM Reference -- -- -- -- -- • HDP/GDM associated with a likelihood of HF 19 • Nulliparity may be associated with fewer HF 20 HPD/GDM 1.19 (1.00, 1.41) 0.05 1.02 (0.83, 1.25) 0.88 1.01 (0.81, 1.27) 0.92 • Associations between pregnancy history and HF attenuated after adjusting for education • Nulliparous women had a lower odds of frequent HF (6+ days) • Important role of socioeconomic factors in pregnancy outcomes • HDP/GDM group had a greater odds of frequent HF and HF Model 1: age (time-varying) HPD = hypertensive pregnancy disorder Model 2: study site, race/ethnicity, financial strain, education GDM = gestational diabetes Model 3: menopause status (time-varying) References Clinical Implications & Future Studies 1.Thurston, R.C. and H. Joffe, Vasomotor symptoms and menopause: findings from the Study of Women's Health across the Nation. Obstet Gynecol Clin North Am, 2011.38(3): p. 489- 501. 2.Freedman, R.R. and W. Krell, Reduced thermoregulatory null zone in postmenopausal women with hot flashes. Am J Obstet Gynecol, 1999. 181(1): p. 66-70. • Pregnancy complications associated with worse CV risk factor profile 3.Thurston, R.C., I.C. Christie, and K.A. Matthews, Hot flashes and cardiac vagal control: a link to cardiovascular risk? Menopause, 2010. 17(3): p. 456-61. 4.Sassarini, J. and M.A. Lumsden, Vascular function and cardiovascular risk factors in women with severe flushing. Maturitas, 2015. 80(4): p. 379-835.Thurston, R.C., et al., Hot flashes in midlife and subclinical cardiovascular disease: findings from the Study of Women's Health Across the Nation Heart Study. Circulation, 2008. 118(12): p. 1234-40. 6.Roberts, J.M., R.N. Taylor, and A. Goldfien, Clinical and biochemical evidence of endothelial cell dysfunction in the pregnancy syndrome preeclampsia. Am J Hypertens, 1991. 4(8): p. 700-8. 7.Levine, R.J., et al., Serum sFlt1 concentration during preeclampsia and mid trimester blood pressure in healthy nulliparous women. Am J Obstet Gynecol, 2006. 194(4): p. 1034-41. • May be associations between pregnancy complications and hot 8.White, W.M., et al., A history of preeclampsia is associated with a risk for coronary artery calcification 3 decades later. Am J Obstet Gynecol, 2016. 214(4): p. 519 e1-8. 9.Morris, E.A. and I.M. Bernstein, Re: Endothelial dysfunction and vascular stiffness in women with previous pregnancy complicated by early or late pre-eclampsia. R. Orabona, E. Sciatti, E. Vizzardi, I. Bonadei and A. Valcamonico. Ultrasound Obstet Gynecol 2017; 49: 116-123. Ultrasound Obstet Gynecol, 2017. 49(1): p. 22-23. flashes in midlife 10.Collen, A.C., K. Manhem, and Y.B. Sverrisdottir, Sympathetic nerve activity in women 40 years after a hypertensive pregnancy. J Hypertens, 2012. 30(6): p. 1203-10. 11.Greenwood, J.P., et al., Sympathetic neural mechanisms in normal and hypertensive pregnancy in humans. Circulation, 2001. 104(18): p. 2200-4. 12.Schobel, H.P., et al., Preeclampsia -- a state of sympathetic overactivity. N Engl J Med, 1996. 335(20): p. 1480-5. In women with HDP/GDM, do HF modulate the risk for CVD later in 13.Jensen, L.A., C.L. Chik, and E.A. Ryan, Review of gestational diabetes mellitus effects on vascular structure and function. Diab Vasc Dis Res, 2016. 13(3): p. 170-82. • 14.Committee on Practice, B.-O., Practice Bulletin No. 137: Gestational diabetes mellitus. Obstet Gynecol, 2013. 122(2 Pt 1): p. 406-16. 15.Bokslag, A., et al., Effect of early-onset preeclampsia on cardiovascular risk in the fifth decade of life. Am J Obstet Gynecol, 2017. life? 16.McDonald, S.D., et al., Cardiovascular sequelae of preeclampsia/eclampsia: a systematic review and meta-analyses. Am Heart J, 2008. 156(5): p. 918-30. 17.Barden, A., et al., Factors predisposing to pre-eclampsia in women with gestational diabetes. J Hypertens, 2004. 22(12): p. 2371-8. 18.Salzer, L., K. Tenenbaum-Gavish, and M. Hod, Metabolic disorder of pregnancy (understanding pathophysiology of diabetes and preeclampsia). Best Pract Res Clin Obstet Gynaecol, 2015. 29(3): p. 328-38. 19.Drost, J.T., et al., More vasomotor symptoms in menopause among women with a history of hypertensive pregnancy diseases compared with women with normotensive pregnancies. Menopause, 2013. 20(10): p. 1006-11 20. Hess R.,et al. Pregnancy and birth history influence women’s experience of menopause. Menopause. 2008 May -June;15(3).435-41. 4
Recommend
More recommend