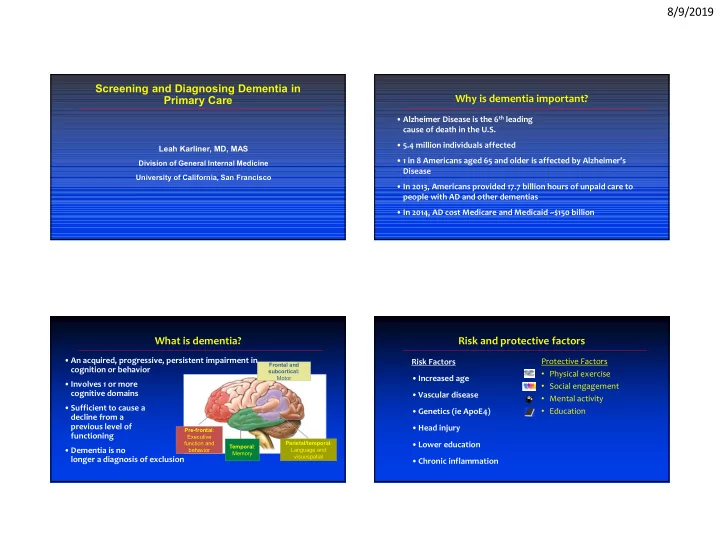
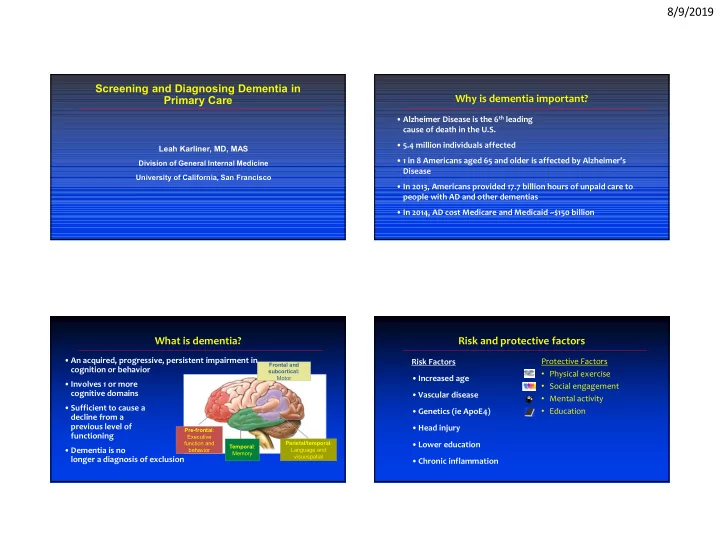
8/9/2019 Screening and Diagnosing Dementia in Primary Care Why is dementia important? • Alzheimer Disease is the 6 th leading cause of death in the U.S. • 5.4 million individuals affected Leah Karliner, MD, MAS • 1 in 8 Americans aged 65 and older is affected by Alzheimer’s Division of General Internal Medicine Disease University of California, San Francisco • In 2013, Americans provided 17.7 billion hours of unpaid care to people with AD and other dementias • In 2014, AD cost Medicare and Medicaid ~$150 billion What is dementia? Risk and protective factors • An acquired, progressive, persistent impairment in Protective Factors Risk Factors Frontal and Frontal and cognition or behavior subcortical: • Physical exercise Motor Motor • Increased age • Involves 1 or more • Social engagement cognitive domains • Vascular disease • Mental activity • Sufficient to cause a • Education • Genetics (ie ApoE4) decline from a previous level of • Head injury Pre-frontal : functioning Executive function and Parietal/temporal : • Lower education Temporal : • Dementia is no behavior Language and Memory visuospatial longer a diagnosis of exclusion • Chronic inflammation 1
8/9/2019 How do you currently screen patients for cognitive USPSTF Guideline impairment or dementia? • Last reviewed in 2014; current update in progress A. I rarely or never screen my patients • USPSTF distinguishes between screening and early detection B. I am inconsistent about how/if I screen patients – “I” or insufficient evidence for formal screening instruments in community-dwelling adults in the general primary care population who are C. I screen all of my older patients regardless of symptoms or older than age 65 years and have no signs or symptoms of cognitive risk factors impairment – Early detection and diagnosis of dementia through the assessment of D. I screen all of my older patients with known risk factors only patient-, family-, or physician-recognized signs and symptoms, some of which may be subtle, are not considered screening E. I only screen patients with symptoms or whose • clinicians should remain alert to early signs or symptoms of cognitive impairment (for companion/caregiver brings up cognitive concerns example, problems with memory or language) and evaluate as appropriate Barriers to dementia screening and early detection in Rationale for screening in primary care primary care • Screening identification of cognitive impairment • Concern re: offending patient • Identification allows • Unsure of who to screen – Treatment of reversible causes of cognitive impairment • Time it takes away from other medical issues during visit – Treatment of conditions exacerbating cognition in dementia • Not knowing what to do with the information – Treatment that can mitigate dementia-related symptoms – PCP ability to contextualize screening for and treatment of other diseases and • Sense of futility due to limited treatments provide anticipatory guidance – Referral to community-based resources for both patients and caregivers • Challenges of screening / diagnostic testing; e.g., lack of familiarity •Educational, support, and skill-building services with screening tools, time, language barriers 2
8/9/2019 Where to begin? KAER Step 1: Kickstart the Conversation • Discuss brain health KAER Model – Gerontological Society of America 2017 – Raise the issue; e.g., ‘brain ages like other parts of our bodies & is important for your overall health’ Kickstart the conversation – Opens the door for patients to express any concerns • Observe for signs and symptoms of cognitive impairment Assess for cognitive impairment – “poor historian” Evaluate for dementias – No-shows for appointments or comes at the wrong time or on the wrong day – Repeatedly and apparently unintentionally fails to follow instructions; e.g., Refer for community resources changing medication https://www.geron.org/programs-services/alliances-and-multi- – Defers to family member to answer questions directed to the patient stakeholder-collaborations/cognitive-impairment-detection-and- earlier-diagnosis • Listen for older adult and family concerns about cognition Case What do you do next? • 80 yo retired chemist who is highly functional and living independently A. Reassure patient that yes everyone has that problem with his wife mentions toward the end of a visit that he sometimes has & it is completely normal 87% trouble finding the right word, and then says ‘but of course everyone B. Explore further, asking about other signs/symptoms has that problem, right?’ of cognitive impairment C. Do a formal cognitive screen in the office D. Send for formal neuro-cognitive testing 9% 2% 2% . . . . . . . . . . e . u n i o e n s e g e b o y a c r c s t g o - a n e h i v r k i u t s t e t a i n n n e , g l i e r o a t h c m a p t l r r a o e u m f r f r u e r o s o s o r f f a a d p l n e o e R x D E S 3
8/9/2019 KAER Step 2: Assess for Cognitive Impairment KAER Step 2: Assess for Cognitive Impairment • Normal brain aging can affect word-retrieval • For a review of how to do this in context of Medicare Annual Wellness Visit: Cordell et al. Alzheimer’s & Dementia 9 (2013) • It can also be a sign of mild cognitive impairment, or – if affecting – Review functional deficits (e.g. managing medications, schedule, money) function – early dementia – Make your own assessment during the visit • The patient’s concern merits further assessment by history – Elicit patient and caregiver (if present) concerns • A formal cognitive screen in the office may be reassuring or highlight If from above, signs or symptoms of cognitive impairment, then do formal cognitive deficits in specific domains cognitive screen • Many screening tools available all with advantages and disadvantages Tool Advantages Limitations Mini-Cog Developed for and validated in primary care Screening Tools Use of different word lists may affect Case http://mini-cog.com/ and with multiple languages and cultural failure rates Score ≤3 is positive groups • Because it was designed to catch mild cognitive Little or no education/language/cultural bias Short administration time impairment, you decide to screen your patient (80 year old chemist) for dementia using the MoCA, so you schedule MMSE Most widely used and studied worldwide Education/age/language/cultural www.parinc.com bias him for a follow-up visit for just this purpose. Required for some drug insurance Score <25 is coverage Ceiling effect (highly educated positive impaired patients pass) • He scores 25/30 – scores normally except for memory Proprietary – unless used from • He recalls 0/5 words on delayed recall memory needs to be purchased • With category prompting he recalls 4/5 MoCA Designed to test for mild cognitive Lacks studies in primary care www.mocatest.org impairment Education bias (≤12 years) Score <26 is Multiple languages accessible on website positive Admin time ≥ 10 min Tests many separate domains 4
8/9/2019 Phenotyping dementias is important for appropriate treatment and anticipatory guidance • Lewy Body Disease • Frontotemporal dementia • This positive screening test merits further diagnostic • Progressive supranuclear palsy evaluation • Corticobasal degeneration • Multiple system atrophy • Many patients (~50%) with cognitive impairment never get a • Amyotrophic lateral sclerosis diagnostic evaluation for dementia • Triplet repeat disease – PCP may not do evaluation (ie Huntington’s Disease) • Paraneoplastic disorders – Family may not want evaluation • Hashimoto’s encephalopathy – Patient may not want / follow-through on evaluation • CNS lymphoma Boustani et al 2005 • Rapidly progressive dementias (ie Fowler et al 2015 Kotagal et al, 2014 Creutzfeld-Jakob disease) McCarten et al, 2012 Adapted from Plassman et al., 2007 Courtesy Howard Rosen Evaluate for Dementia Evaluate for Dementia 1. determine if there is a non-dementia condition causing cognitive In the context of a medical history with patient and informant assessing for impairment --onset, course and nature of memory & other cognitive impairments • Medication/substance evaluation --associated behavioral, medical, psychological issues – Opioids, TCAs, benzos, non-benzo hypnotics, muscle relaxants, --recent illness, falls & head injury, medications, OTC/herbals, substance use antihistamines, anti-epilectics – Substances: alcohol, drugs --vision and hearing problems, depression • Sensory & Mood assessment: Vision, hearing, depression 1. determine if there is a non-dementia condition causing cognitive impairment • Labs: exclude underlying infection, uremia, liver and thyroid disease; check B-12, folate, calcium, fasting glucose, HIV 2. Determine if patient meets diagnostic criteria for neuro-cognitive disorder • Neuro-imaging: MRI (or non-con CT) to exclude tumors, subdural 3. identify the cause of neurocognitive impairment hematomas, hydrocephalus 5
Recommend
More recommend