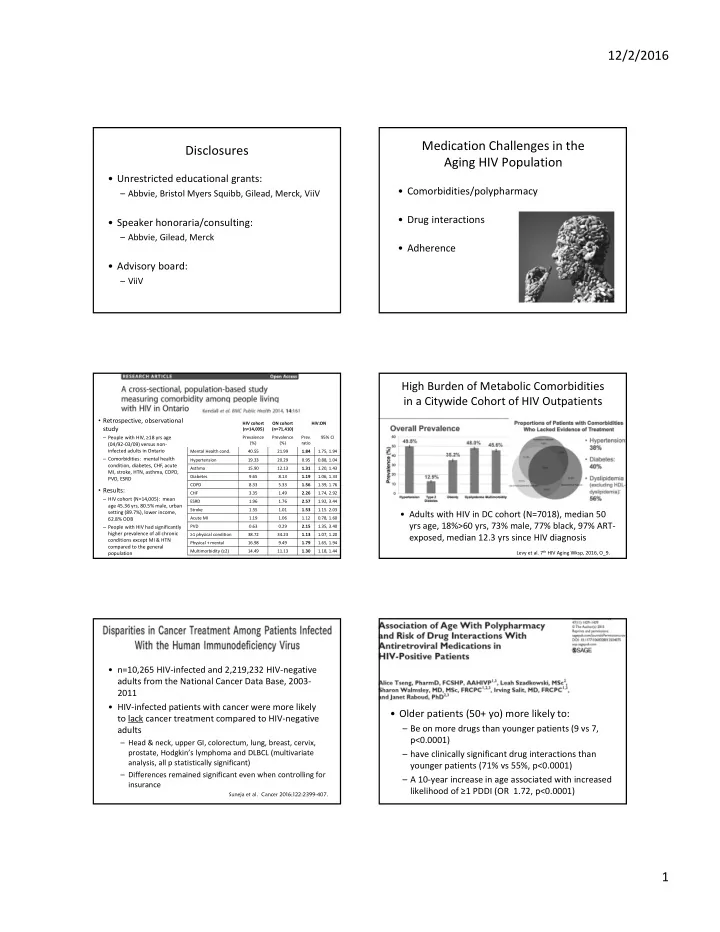
12/2/2016 Medication Challenges in the Disclosures Aging HIV Population • Unrestricted educational grants: • Comorbidities/polypharmacy – Abbvie, Bristol Myers Squibb, Gilead, Merck, ViiV • Drug interactions • Speaker honoraria/consulting: – Abbvie, Gilead, Merck • Adherence • Advisory board: – ViiV High Burden of Metabolic Comorbidities in a Citywide Cohort of HIV Outpatients • Retrospective, observational HIV cohort ON cohort HIV:ON study (n=14,005) (n=71,410) – People with HIV, ≥18 yrs age Prevalence Prevalence Prev. 95% CI (%) (%) ratio (04/92‐03/09) versus non‐ infected adults in Ontario Mental Health cond. 40.55 21.99 1.84 1.75, 1.94 – Comorbidities: mental health Hypertension 19.33 20.29 0.95 0.88, 1.04 condition, diabetes, CHF, acute Asthma 15.90 12.13 1.31 1.20, 1.43 MI, stroke, HTN, asthma, COPD, Diabetes 9.65 8.13 1.19 1.06, 1.33 PVD, ESRD COPD 8.33 5.33 1.56 1.39, 1.76 • Results: CHF 3.35 1.49 2.26 1.74, 2.92 – HIV cohort (N=14,005): mean ESRD 1.96 1.76 2.57 1.92, 3.44 age 45.36 yrs, 80.5% male, urban Stroke 1.55 1.01 1.53 1.15. 2.03 setting (89.7%), lower income, • Adults with HIV in DC cohort (N=7018), median 50 Acute MI 1.19 1.06 1.12 0.78, 1.60 62.8% ODB yrs age, 18%>60 yrs, 73% male, 77% black, 97% ART‐ – People with HIV had significantly PVD 0.63 0.29 2.15 1.35, 3.40 higher prevalence of all chronic ≥1 physical condition 38.72 34.23 1.13 1.07, 1.20 exposed, median 12.3 yrs since HIV diagnosis conditions except MI & HTN Physical + mental 16.98 9.49 1.79 1.65, 1.94 compared to the general Multimorbidity (≥2) 14.49 11.13 1.30 1.18, 1.44 Levy et al. 7 th HIV Aging Wksp, 2016, O_9. population • n=10,265 HIV‐infected and 2,219,232 HIV‐negative adults from the National Cancer Data Base, 2003‐ 2011 • HIV‐infected patients with cancer were more likely • Older patients (50+ yo) more likely to: to lack cancer treatment compared to HIV‐negative – Be on more drugs than younger patients (9 vs 7, adults p<0.0001) – Head & neck, upper GI, colorectum, lung, breast, cervix, prostate, Hodgkin’s lymphoma and DLBCL (multivariate – have clinically significant drug interactions than analysis, all p statistically significant) younger patients (71% vs 55%, p<0.0001) – Differences remained significant even when controlling for – A 10‐year increase in age associated with increased insurance likelihood of ≥1 PDDI (OR 1.72, p<0.0001) Suneja et al. Cancer 2016;122:2399-407. 1
12/2/2016 Older HIV+ Patients More Likely to be On Medication‐Related Problems in HIV‐ Treatment for Comorbid Conditions Infected Adults Over the Age of 60 <50 years ≥50 years P value (n=498) (n=416) 96% Anti-infective 36% 45% <0.0001 74% 70% CAM 5% 9% 0.01 52% GI medications 49% 66% <0.01 29% 29% CV medications 26% 65% <0.0001 17% Anticoagulation/anti-platelet 3% 6% <0.01 4% P<0.01 P=0.03 Systemic hormonal agents 10% 16% <0.01 P=0.07 MSK agents (incl. osteoporosis) 10% 20% <0.0001 Narcotics/analgesics 23% 39% <0.0001 • N=89 (91% Caucasian, 94% male, median age 64, median 13 Antidepressants 19% 25% 0.04 medications (2‐38), 4 ARVs Psychotropics 21% 29% <0.01 • Age/sex‐matched controls (n=28): median 6 medications (p=0.03) Greene et al. J Am Geriatric Soc 2014;62:447‐53. [Tseng A et al. Ann Pharmacother 2013;47:1429‐39.] Potential Consequences of Polypharmacy and Drug Interactions • 1329 HIV+ patients receiving care between 2000‐2013 – Average 47 years old, 5 (3‐7) comorbidities, 3 (1‐5) non‐HIV meds – 34% PI, 46% NNRTI, 29% InSTI regimens • 128 (9.6%) had a contraindicated drug‐drug interaction (XDDI) • 214 (16.1%) patients hospitalized in first year of starting cART • Patients with XDDIs had a significantly higher probability of being hospitalized than patients without an XDDI [Jakeman et al. ICAAC 2015, H‐780] Slide 15 209 admissions in OR (CI) which an ARV was prescribed for HIV+ 3.6 (1.8-7.3) patient Review of Records: 89 potential errors in 77 admissions (25.8%) 4.5 (2.6-8.1) 17 patients (19%) 15 patients (17%) 13 patients 44 patients given HAART > received (15%) received (49%) given 24h after < 3 antiretrovirals contraindicated incorrect dose or 3.9 (1.9-8.1) admission combination of frequency 4.6 (2.6-8.1) drugs 2.8 (1.4-5.3) 12 patients 1 error corrected * 6 – Simvastatin + received within 24h 5.5 (3.1-9.8) boosted PI contraindicated 6 – PPI + Atazanavir drug for > 24h * 2
12/2/2016 ACTG Co‐medication Use Has a Negative A5322: Tassiopoulos, HIV & Aging Wksp 2016, O_8 Impact on ART Continuity & Adherence • n=967, mean age 51 (46‐56), 19% • Patients with non‐ART polypharmacy are female, 48% white, 92% more likely to stop or change ART than VL<50 • 18% had ≥1 patients not experiencing polypharmacy fall in past 18 months (36.8% vs 30%, p<0.01 ) • 7% had recurrent • Polypharmacy is a predictor of ART non‐ falls • 5.2% adherence (multivariate analysis) experienced fracture as a result of fall Krentz et al. AIDS Pt Care STDs 2016;30:1‐7. Cantudo‐ Cuenca et al. J Manag Care Pharm 2014;20:844‐50. Incomplete adherence to modern Mr. LF HAART over time is strongly associated with increased mortality • Saquinavir/ritonavir BID, tenofovir/emtricitabine • Atorvastatin • Inhalers: tiotropium (Spiriva), indacaterol (Onbrez) • New Rx: – tamsulosin (Flomax) – carbidopa‐levodopa (Sinemet) – citalopram (Celexa) Hazard ratio for mortality of 903 patients with HIV, stratified by adherence initial regimen. Vertical bars=95% CI Lima et al. J Acquir Immune Defic Syndr 2009;50:529–536. Mr. LF: Drug Interaction Considerations Mr. LF: DDI Considerations • Ritonavir inhibits CYP3A4, P‐gp, induces • Pharmacodynamic: CYP1A2, 2B6, 2C9/19, UGT Metabolism Potential Management Interaction Tamsulosin CYP3A4 Strong CYP3A4 inhibitors tamsulosin contraindicated. *based on PK studies, could consider 0.4 mg dose with monitoring Possible Carbidopa‐ Decarboxylation, Case report of levodopa toxicity Levodopa O‐methylation> carbidopa‐ (incl. severe dyskinesias) with • Drug‐Disease: transamination, levodopa indinavir use & rechallenge. Use oxidation with caution. – Boosted PI + dyslipidemia; tenofovir DF + renal, bone? Possible Citalopram CYP2C19, 3A4 Use with caution; citalopram dose citalopram reduction may be necessary 3
12/2/2016 Impact of Aging on Drug Disposition Impact of Aging on Medication Taking and Tolerance • Older patients often have better adherence Pharmacokinetics: Pharmacodynamics: rates compared to younger patients • More predisposed to ADRs • Renal insufficiency: • However, other possible challenges: – sensitivity to central & – Cockcroft‐Gault for dosing – Managing side effects peripheral anticholinergic s/e • Hepatic dysfunction – benzodiazepine clearance – Scheduling HIV medications with other drugs – baroreceptor responsiveness – use Child‐Pugh for dose ( , ‐blockers, ‐agonists) – Changes in vision/hearing (labels, counselling) adjustment – CNS sensitivity to opioids and – Dexterity: opening pill vials, containers – e.g., abacavir, NNRTIs, PIs sedatives – Mobility: picking up refills • Avoid or use certain drug classes with caution – Memory: remembering to take medications – Financial: Rx deductibles, dispensing fees [Abrass et al. HIV & Aging Consensus Project, 2011.] Optimizing Medication Use in the Polypharmacy in the Older HIV Aging Population Population: A Double‐Edged Sword? More common compared to But still not enough? younger patients: • Potential under‐ treatment of non‐HIV • Often more HIV‐treatment related comorbidities experienced • Lack of care – may require more complex coordination regimens due to resistance • treatment bias? – may not be candidates for STRs • Higher rate of age‐related comorbidities versus age‐ matched controls 2. Co-morbidity Prevention & 1. Simplify/Update ART Treatment • E.g FDCs, STRs, once daily dosing, etc. • Ensure access to gold standard of care. – Fewer pills, adherence, fewer dispensing fees – HIV is not an exclusion to treatment or a • Select drugs with good tolerability and reason for suboptimal treatment! low interaction potential • May be limited by ARV resistance • Managing ART + co‐medications: – Dose‐adjust/monitor for efficacy & toxicity • May need to consider non‐traditional – Consider alternative therapeutic options ART combinations 4
12/2/2016 4. Consolidate Care/ 3. Home Organization Manage Transitions in Care • Medicine cabinet clean‐up • Encourage use of single pharmacy • Annual brown‐bag visit • Communicate/plan with other care providers • OT consult? Social/family supports • Medication reconciliation (annual outpatient, hospital admissions/discharge) • Communication between providers is essential! 5
Recommend
More recommend