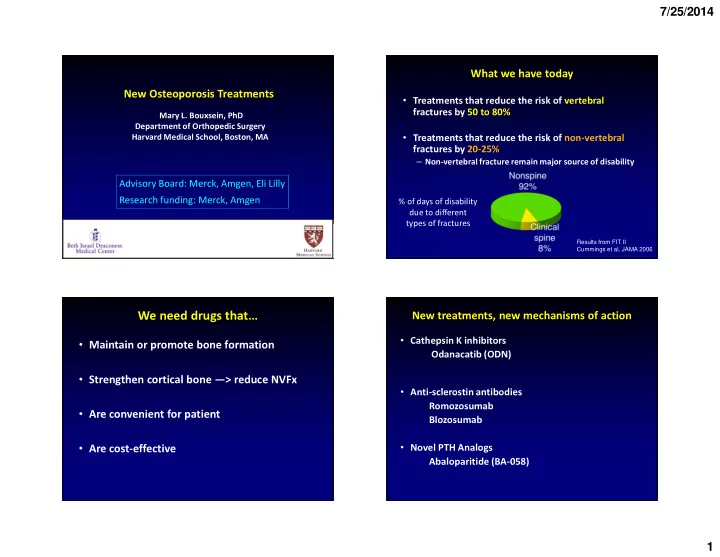
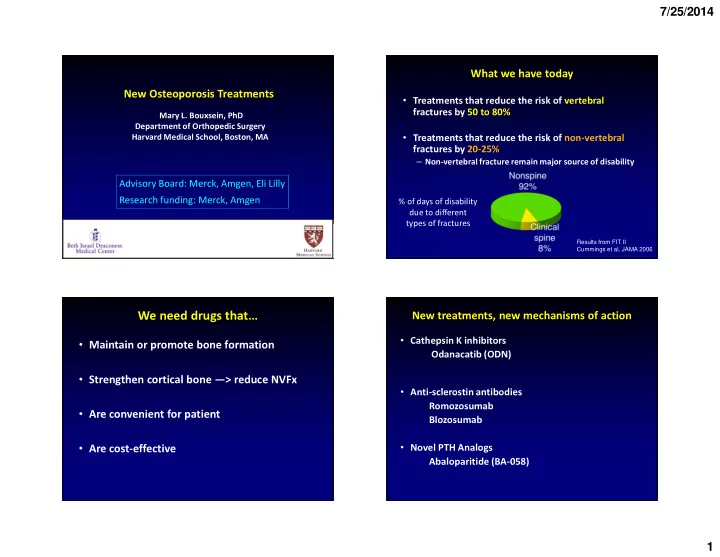
7/25/2014 What we have today New Osteoporosis Treatments • Treatments that reduce the risk of vertebral fractures by 50 to 80% Mary L. Bouxsein, PhD Department of Orthopedic Surgery • Treatments that reduce the risk of non-vertebral Harvard Medical School, Boston, MA fractures by 20-25% – Non-vertebral fracture remain major source of disability Advisory Board: Merck, Amgen, Eli Lilly Research funding: Merck, Amgen % of days of disability due to different types of fractures Results from FIT II Cummings et al, JAMA 2006 We need drugs that… New treatments, new mechanisms of action • Cathepsin K inhibitors • Maintain or promote bone formation Odanacatib (ODN) • Strengthen cortical bone —> reduce NVFx • Anti-sclerostin antibodies Romozosumab • Are convenient for patient Blozosumab • Are cost-effective • Novel PTH Analogs Abaloparitide (BA-058) 1
7/25/2014 Global deletion of Cathepsin K in mice decreases Cathepsin K and Bone Resorption bone resorption but increases bone formation • Distal femur CatK is a lysosomal protease highly expressed in osteoclasts, where it is Serum CTx WT released during bone resorption. • CatK is the major protease responsible for degradation of type I collagen WT KO BFR/BS KO KO WT Rodan SB et al. IBMS BoneKey. 2008;5:16–24. Pennypacker B. et al., Bone, 2009 Coupling of bone formation & resorption How can cathepsin K inhibition lead to “ “ Clastokines ” “ “ ” ” ” increased bone formation? OPG Revisiting the ‘ ‘ ‘ coupled ’ ‘ ’ process of ’ ’ RANKL bone remodeling MDGFs (IGF1, TGFß) Image courtesy of R. Baron • Direct effects on osteoblasts? • Indirect effects via the osteoclasts and coupling? 2
7/25/2014 Osteoclasts have a dual function Genetic deletion of CatK in osteoclasts ↑ Bone mass ↓ Bone resorption ↑ Bone formation Bone ↑ Osteoclast # Formation CON OC CatK KO BFR/TV (%/year) * # Oc BFR N.Oc/TA (/mm 2 ) * WT KO WT KO Bone Resorption Lotinun, et al. J Clin Invest, Feb 2013 Human Osteoclasts Pharmacologic inhibition of CathepsinK Effects of reducing CON Odanacatib activity of CatK in the osteoclast Odanacatib is a selective, and reversible nonbasic inhibitor of Cat K with minimal metabolism, which • Same or increased supports once weekly dosing in humans. number of F osteoclasts CF 3 IC 50 (nM) H N ODN-treated N N Cat K 0.2 H O • Shallow resorption Cat B 1,034 pits MeO 2 S Cat L 2,995 Cat S 60 IC 50 = 50% inhibitory concentration; Cat = cathepsin. Duong LT. BoneKey Reports . 2012;1. Article no. 67. Leung et al. Bone, 2011 Gauthier JY et al. Bioorg Med Chem Lett . 2008;18:923–928. 3
7/25/2014 ODN treatment increases avg. cortical thickness ODN increases periosteal bone formation in in femur of OVX monkeys proximal femur of OVX monkeys Proximal Femur Cortical Thickness, mm Central Femur # A # p<0.05 vs VEH 4.0 50 Mineralized Surface, % Proximal Femoral Periosteum (Rhesus monkeys @ 21-mo Tx) 40 VEH Veh. 30 TCY MS/BS 3.6 20 10 0 Veh 6 30 3.2 ODN, mg/kg B 0.8 0 Mineral Apposition # Veh 6 30 0.6 Rate, µm/d ODN, mg/kg 0.4 MAR ODN 0.2 Cortical Thickness, mm Femoral Neck TCY 0 ODN † Veh 6 30 1.6 † p = 0.08 vs VEH ODN, mg/kg C 120 # 1.4 Bone Formation Rate, µm 3 /µm 2 /y 90 60 BFR 1.2 30 0 0 Veh 6 30 Veh 6 30 ODN, mg/kg ODN, mg/kg # P <0.05 vs Veh. Cusick T et al. J Bone Miner Res . 2012;27:524–537. Cusick et al. J Bone Miner Res . 2012;27:524–537. Randomized trial (phase 2b) • Original: 2 year dose-ranging study • Postmenopausal women 45-85 years (N=399) Human trials • BMD T-score < -2.0 but not < -3.5 • 50 mg odanacatib vs. placebo (once weekly, oral) • After 2 years, randomly assigned to stop or continue to 5 years Langdahl et al. JBMR 2012 4
7/25/2014 Study design Lumbar spine BMD Years 4 & 5 a Years 1 & 2 Year 3 Women who entered the 15 PBO/PBO (n=14) (N=399) (N=189) (N=141) Year 4 to 5 extension 14 ODN 50 mg/50 mg/50 mg (n=13) 13 PBO 50 mg n=13 11.9% ODN 50 mg/PBO/PBO (n=14) 12 PBO 11 50 mg 50 mg 50 mg n=15 from baseline (SE) Mean % change 10 9 PBO 50 mg n=14 8 3 mg 7 50 mg 50 mg 50 mg n=14 6 5 PBO PBO n=13 4 Placebo 10 mg 3 50 mg 50 mg n=12 2 1 PBO n=14 PBO 0 –0.4% 25 mg 0.8% –1 Placebo 50 mg 50 mg n=16 –2 n=14 PBO PBO 0 3 12 24 36 48 60 50 mg 1 6 18 30 42 54 50 mg 50 mg n=16 PBO = placebo. Month a Year 6 to 10 extension in planning. Langdahl et al. JBMR 2012 Langdahl B et al. J Bone Miner Res . Nov 2012 Femoral neck BMD Effect of ODN on bone resorption markers PBO/PBO ODN 50 mg/50 mg/50 mg 15 PBO/PBO (n=14) ODN 50 mg/PBO/PBO 14 ODN 50 mg/50 mg/50 mg (n=13) uNTx/Cr ratio 13 100 ODN 50 mg/PBO/PBO (n=14) 12 11 75 % change rom baseline ± SE) 9.8% 10 from baseline (SE) Mean % change 50 9 50 mg (geometric mean ± ± ± 8 25 7 50 mg 6 0 5 4 -25 3 2 Placebo -50 1 0 -75 Placebo –1 –1.6% –0.5% –2 -100 0 6 12 18 24 30 36 42 48 54 60 0 3 12 24 36 48 60 Month 1 6 18 30 42 54 Month Langdahl et al. JBMR 2012 Langdahl et al. JBMR 2012 5
7/25/2014 Iliac crest bone biopsies at 24 mo ODN: Bone turnover markers (Ph III imaging study) ODN 50 mg OW N=74-76 Placebo OW N=78-80 ODN 50 mg OW Placebo OW (n=5) (n=5) ± SEM) ± SEM) Geometric LS Mean Percent Geometric LS Mean Percent CTX P1NP Osteoid Thickness, micron 5.06 (1.07) 5.60 (0.85) 20 -1.99 10 ± Change from Baseline ( ± ± 3.03 ± ± Change from Baseline ( ± Mineral Apposition Rate, micron/day 0.58 (0.05)* 0.56 (0.10) 10 0 Mineralizing Surface, % 5.52 (5.88) 6.32 (4.22) 0 -10 Mineralization Lag Time, day 21.03 (23.88)* 31.96 (36.63) -10 Bone Formation Rate, Total Volume Referent, -20 -20 -11.06 * 18.72 (16.29)* 23.14 (13.94) %/yr -30 * -30 Bone Formation Rate, Total Surface Referent, * -40 * 0.04 (0.03)* 0.03 (0.02) * micron 3 / micron 2 / day -40 * -50 -42.56 Eroded Bone Surface, % 1.90 (1.32) 1.66 (1.13) -60 -50 Activation Frequency /yr 0.47 (0.38)* 0.50 (0.30) 6 12 18 24 6 12 18 24 Month Month Osteoclast bone surface, % trab surface 0.93 (0.92) 0.35 (0.23) covered by OC * P<0.001 vs PBO *n=4 Brixen et al, JCEM 2013 98(2):571-80 Per-Protocol Population Brixen et al, JCEM 2013 98:571-80 Phase 3 Fracture Trial Phase 3 Fracture Trial: Updates “ The study met its primary efficacy outcomes … and is being concluded • July 2012: study stopped early • Randomized, placebo-controlled issues remain in certain selected areas ” • ODN (50 mg/wk) vs PBO early… Robust efficacy and a favorable benefit-risk profile… safety “ ODN reduced the risk of osteoporotic fractures vs. placebo, including • May 2014: press release • >16,000 subjects enrolled vertebral, non-vertebral and hip fractures, … Among adjudicated – Age > 65 yrs adverse effects associated with odanacatib, morphea was reported – Low hip BMD, with or without prior vertebral fx uncommonly (<0.2%), with improvement after discontinuation of reported cases of osteonecrosis of the jaw. “ treatment, and femoral shaft fractures of an atypical type were rare (<0.1%). Both were higher than placebo. There were no • Plan to file for FDA approval in second half of 2014 6
7/25/2014 Sclerostin: Osteocyte-derived cytokine that New treatments, new mechanisms of action inhibits bone formation • Sclerosteosis, van Buchem ’ ’ ’ ’ s disease • Cathepsin K inhibition Odanacatib (ODN) -- Due to mutations in gene SOST Courtesy of C Lowik/W Van Hul • Anti-sclerostin antibodies • Sclerostin: protein encoded by gene SOST – Potent inhibitor of Wnt signaling & Romozosumab bone formation Blozosumb – Deletion of SOST in mice: ↑ bone mass – Sclerostin expression localized to osteocytes Li et al, JBMR 2008 Treatment of rats & monkeys with Sclerostin Antibody Phase 2 Study of Sclerostin Antibody (Romozosumab) in Postmenopausal Women with Low BMD SHAM Li et al, JBMR 2009 OVX + VEH OVX + SclAb Vertebral Strength VEH SclAb Ominsky et al, JBMR 2011 7
7/25/2014 Phase 2 Study Design Phase 2 Study Design McClung et al, NEJM 2014 McClung et al, NEJM 2014 Lumbar spine BMD Total hip and femoral neck BMD Romosozumab TPTD ALN PBO McClung et al, NEJM 2014 8
7/25/2014 % Change in serum bone turnover markers: New treatments, new mechanisms of action P1NP and CTX • Cathepsin K inhibition CTX P1NP Odanacatib (ODN) • Anti-sclerostin antibodies Romozosumab Blozosumb • Novel PTH Analogs Abaloparitide (BA-058) Phase 2 Clinical Study: Spine BMD at 48 Weeks Abaloparatide (BA058): Introduction 16 Abaloparatide is a novel analog of hPTHrP (1-34) +12.9% 14 hPTH 12 +9.8% % Change in BMD 1 34 +8.6% 10 hPTHrP Week 12 1 22 34 Week 24 8 ABL Week 48 +5.1% 6 100% hPTHrP 38% hPTHrP 4 +0.7% 2 Abaloparatide was selected to achieve • Potent and rapid bone anabolic activity 0 Placebo ABL ABL ABL Teriparatide • Limited effect on bone resorption 40 µ g 20 µ g 80 µ g • Room temperature stability Mean (SE) % Change in Lumbar Spine BMD from Baseline (Ext. pop, N=55) 9
Recommend
More recommend