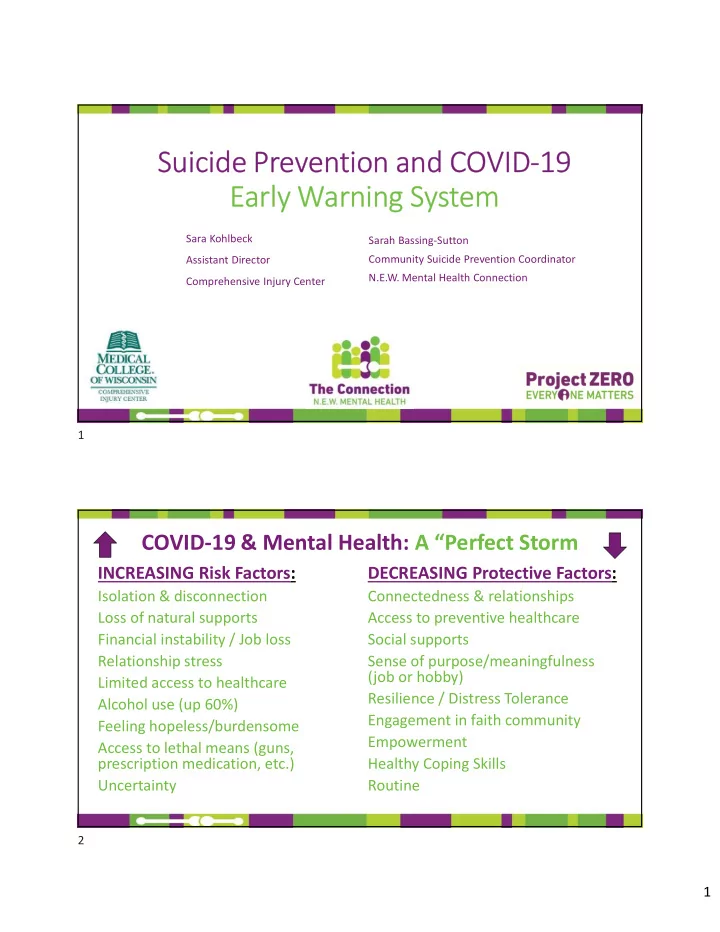
Suicide Prevention and COVID-19 Early Warning System Sara Kohlbeck Sarah Bassing-Sutton Community Suicide Prevention Coordinator Assistant Director N.E.W. Mental Health Connection Comprehensive Injury Center 1 COVID-19 & Mental Health: A “Perfect Storm INCREASING Risk Factors: DECREASING Protective Factors: Isolation & disconnection Connectedness & relationships Loss of natural supports Access to preventive healthcare Financial instability / Job loss Social supports Relationship stress Sense of purpose/meaningfulness (job or hobby) Limited access to healthcare Resilience / Distress Tolerance Alcohol use (up 60%) Engagement in faith community Feeling hopeless/burdensome Empowerment Access to lethal means (guns, prescription medication, etc.) Healthy Coping Skills Uncertainty Routine 2 1
Impact of COVID-19 on Mental Health & Suicide (Kaiser Family Foundation Poll) • 45% of adults say the crisis has had a “negative impact” on their mental health • 19% say it has had a “major impact” on their mental health • 65% of adults who lost income report worsened mental health • 50% increase in local police contacts for mental health crisis and suicide-related behaviors • 891% increase in calls to SAMHSA’s Disaster Distress Hotline 3 Wellbeing has declined significantly (General Public and Healthcare Professionals) https://suicidology.org/2020/05/05/ai-healthcare-professionals-mental-health/ 4 2
Projected Deaths of Despair Alongside the thousands of deaths from COVID-19, the growing epidemic of “deaths of despair” is increasing due to the pandemic—as many as 75,000 more people will die from drug or alcohol misuse and suicide (Well Being Trust (WBT) and Robert Graham Center for Policy Studies in Primary Care) WI Unemployment Rate in April 2020: 14.1% For every 1% increase in unemployment rate, over a year, we would lose 775 more Americans to suicide, 1,200 to overdose and increase by 10,000 those experiencing depression, anxiety and addiction 5 Assessing Need in Your Community Risk Factors: • What are they and how are they changing? Protective Factors • What are they and how are they changing? 6 3
Partnership and Collaboration 7 Formation of the Partnerships • Northeast Wisconsin Mental Health Connection • Backbone agency • Value added • Trust built • “All oars rowing in the same direction” • Other community collaborations preceding this • Project Zero: Every 1 Matters/Medical College of WI • Tri-County initiative • Coroners • Law Enforcement • County Mental Health Crisis providers 8 4
The Work of the Early Warning System • Entering data from law enforcement incident calls • Law Enforcement into a spreadsheet • Gender, Age, Race, Time, • Mental Health Crisis Divisions Date, Mechanism, Primary and Secondary Triggers, Location • Coroners Office • Regular contact with Coroners regarding suicides • Regular monitoring of Crisis Call volume 9 Bumps along the way…. • Community Partners have their own work to do • Capacity • System to collect and share data agreed upon by all partners • Confidentiality of information collected 10 5
New System Response for Suicide Related Behavior (5/22/20) GOALS: • Less “hot potato” • Law Enforcement more time to enforcing laws and less time evaluating • Consumers experience a more humane and less transactional process • Fewer Ch. 51’s • Educating the partners who regularly interact in the system response a clear understanding of the criteria they each use to make the decisions they do-ED/LE/Crisis 11 Building the Coalition • Current Suicide Prevention partners and roles in this effort? • Who NEEDS to be engaged and what will their role be? • Data Collection and analysis 12 6
Real Time Data on Suicide Related Behavior Data: March 13 – July8, 2020 Calumet, Outagamie and Winnebago Counties 13 Daily calls over time (n = 869) Shows a 32.8% increase over time 16 14 12 10 8 6 4 2 0 14 7
Percent by Call Type Mental Health Suicidal Ideation Suicide Attempt Completed Suicide 0 10 20 30 40 50 60 70 80 15 Percent Calls by Gender Transgender M-f 0% Male 54% Other 1% Transgender F- M 1% Female 45% 16 8
Percent Mechanism of Injury Gender 120 100 80 60 40 20 0 Female Male Transgender F-M Transgender M-F Firearm Sharp Object Hanging Poisoning Fall Other/Unknown 17 Percent Calls by Mechanism of Injury Top 3 Other/Unkno wn 23% 1. Poisoning-Rx Drug Poisoning (Prescription Drug) Jumping in 21% Front of 2. Sharp Object Vehicle 4% Fall from Sharp Object Heights 3. Firearm 20% 4% Hanging Poisoning 7% (Non- Prescription Firearm Drug) 14% 7% 18 9
Percent by Day of Week/time of Day 16 40 15.5 35 15 30 14.5 25 14 20 13.5 15 13 10 12.5 5 12 0 Midnight to 6:00 a.m. to Noon to 5:59 6:00 p.m. to 5:59 a.m. 11:59 a.m. p.m. 11:59 p.m. 19 Calls by age group over time 12 10 8 6 4 2 0 13-Mar 20-Mar 27-Mar 3-Apr 10-Apr 17-Apr 24-Apr 1-May 8-May 15-May 22-May 29-May 5-Jun 12-Jun 19-Jun 26-Jun 3-Jul Ages 25-54 Ages 10-24 Ages 55+ 20 10
Percent by Primary Triggering Event (41% had more than one event listed) Death of Unknown Other a Loved Top 3 5% 3% One Physical 3% Health 1. Mental Health 5% Financial Issue 5% 2. Relationship Mental Substance Health Use Issues 40% 12% Relationship 3. Substance Use Issue 27% 21 Outagamie and Winnebago County Suicides 12 12 10 10 8 8 6 6 4 4 2 2 0 0 March April May June 2018 2019 2020 2018 2019 2020 22 11
Data Considerations • Rates of suicide deaths and attempts in your community? • How do you access information on suicide ideation and attempts in your community • What other types of data do you need to implement and evaluate this effort? • How will you access that? 23 “Dream” Team Multi-disciplinary team • Law Enforcement • Mental Health Provider • County Crisis • Lived Experience • Academic Partners • Representation of communities at highest risk 24 12
Opportunities for System Innovation 25 Ideal System Response- First Responders 26 13
Ideal System Response: Emergency Department 27 Ideal System Response: Completed Suicide 28 14
Barriers and Facilitators • What forces will facilitate this effort in your community? How might you leverage those? • What forces will present a barrier to this effort in your community? How might you work to dismantle those? 29 Q & A /Thank you Sarah Bassing-Sutton sarah@newmentalhealthconnection.com 920-420-4903 This project is funded by the Sara Kohlbeck Advancing a Healthier Wisconsin skohlbeck@mcw.edu Endowment at the Medical College of Wisconsin Beth Clay beth@newmentalhealthconnection.com 920-202-0117 30 15
Recommend
More recommend