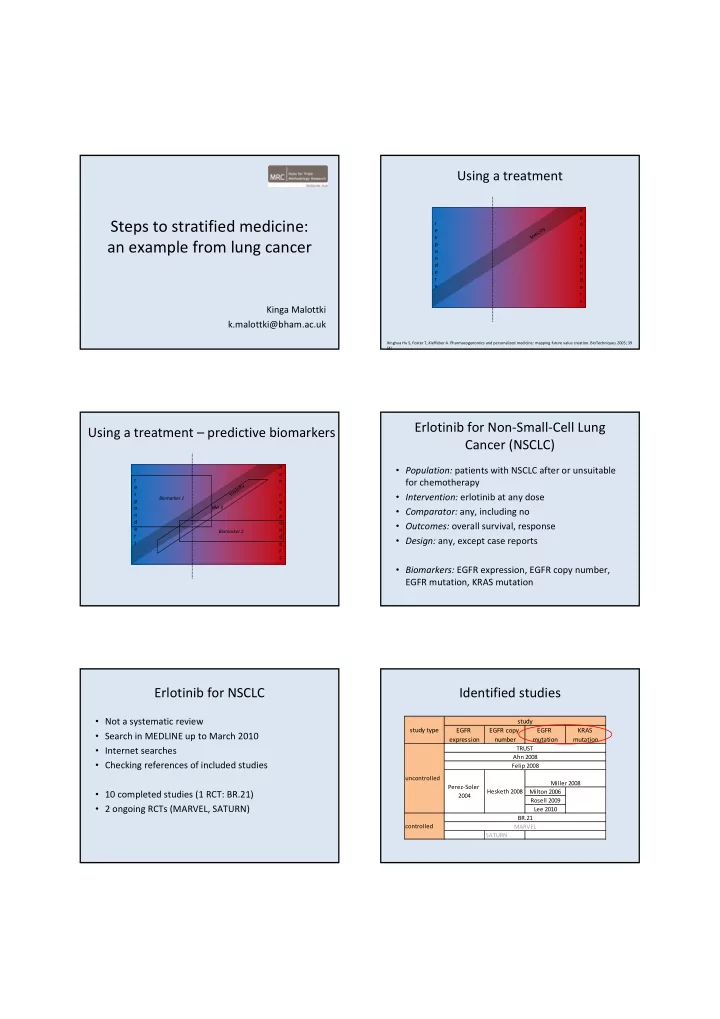
Using a treatment n o Steps to stratified medicine: r n toxicity e ‐ s r an example from lung cancer p e o s n p d o e n r d s e r s Kinga Malottki k.malottki@bham.ac.uk Xinghua Hu S, Foster T, Kieffaber A. Pharmacogenomics and personalized medicine: mapping future value creation. BioTechniques 2005; 39 (4) Erlotinib for Non ‐ Small ‐ Cell Lung Using a treatment – predictive biomarkers Cancer (NSCLC) n • Population: patients with NSCLC after or unsuitable o r n for chemotherapy toxicity e ‐ s r • Intervention: erlotinib at any dose Biomarker 1 p e o BM 3 s • Comparator: any, including no n p d o • Outcomes: overall survival, response e n Biomarker 2 r d • Design: any, except case reports s e r s • Biomarkers: EGFR expression, EGFR copy number, EGFR mutation, KRAS mutation Erlotinib for NSCLC Identified studies • Not a systematic review study study type EGFR EGFR copy EGFR KRAS • Search in MEDLINE up to March 2010 expression number mutation mutation • Internet searches TRUST Ahn 2008 • Checking references of included studies Felip 2008 uncontrolled Miller 2008 Perez ‐ Soler Hesketh 2008 • 10 completed studies (1 RCT: BR.21) Milton 2006 2004 Rosell 2009 • 2 ongoing RCTs (MARVEL, SATURN) Lee 2010 BR.21 controlled MARVEL SATURN
Using a treatment – predictive biomarkers EGFR mutations in NSCLC • Found in: n – ~30 ‐ 50% East ‐ Asian o r n – ~10% Western Europe and North America toxicity e ‐ s r • More frequent in: EGFR mutation p e – Never smokers o s n p – Females d o – Adenocarcinomas e n r d – East ‐ Asian s e • Prognosis unclear (some studies seem to show increased r s survival in patients with mutations) • Exons 18 ‐ 21, most common deletions in exon 19 and missense mutation in exon 21 (L858R) – ~85% Reference list available on request EGFR mutation – overall survival EGFR mutations in included studies BR.21 survival HR: erlotinib vs. placebo Survival HR: EGFR mutation vs. wild type • 8 studies (N: 21 ‐ 731) assessed EGFR mutations study N HR group N ERL vs. PL 6 mutation 0.33 • Mutation status available for 19 ‐ 100% of patients all patients 731 HR 0.7 (0.58, 0.85) TRUST 85 wild type (0.12, 0.91) wild type 137 HR 0.73 (0.49, 1.10) 5 mutation 0.902 Felip 2008 34 wild type (p=0.8468) • 7 studies used polymerase chain reactions (PCR), 1 mutation 40 HR 0.77 (0.40, 1.50) study did not report the method Median survival (months): all patients, EGFR mutation and wild type • Mutations assessed: – 5 studies: exons 19 and 21, – 2 studies: exon 18 , 19 and 21 – 1 study: exon 18 ‐ 21 Ahn 2008: mutation assessed in 92 of 120; OS longer in mutation (p=0.023 vs. wild type) – possibly long OS in patients in whom mutation could not be assessed EGFR mutation – predicting response EGFR mutation – response OR (RECIST) Index test: EGFR mutation Reference test: response EGFR mutation EGFR wild type Odds Ratio Odds Ratio Study or Subgroup Events Total Events Total Weight M-H, Random, 95% CI M-H, Random, 95% CI Ahn 2008 14 24 11 68 29.8% 7.25 [2.57, 20.46] BR.21 4 15 7 101 22.4% 4.88 [1.23, 19.37] Felip 2008 2 5 1 34 8.7% 22.00 [1.51, 319.48] Study TP FP FN TN Sensitivity Specificity Sensitivity Specificity Lee 2010 2 3 1 9 6.5% 16.00 [0.67, 383.02] Ahn 2008 14 10 11 57 0.56 [0.35, 0.76] 0.85 [0.74, 0.93] Miller 2008 15 18 4 63 18.7% 73.75 [14.88, 365.52] BR.21 4 10 7 94 0.36 [0.11, 0.69] 0.90 [0.83, 0.95] Milton 2006 1 1 0 3 3.6% 21.00 [0.27, 1646.18] TRUST 2 4 2 68 10.3% 33.00 [2.96, 368.36] Felip 2008 2 3 1 33 0.67 [0.09, 0.99] 0.92 [0.78, 0.98] Lee 2010 2 1 1 8 0.67 [0.09, 0.99] 0.89 [0.52, 1.00] Total (95% CI) 70 346 100.0% 14.41 [6.08, 34.13] Miller 2008 15 3 4 59 0.79 [0.54, 0.94] 0.95 [0.87, 0.99] Total events 40 26 Heterogeneity: Tau² = 0.37; Chi² = 8.44, df = 6 (P = 0.21); I² = 29% Milton 2006 1 0 0 3 1.00 [0.03, 1.00] 1.00 [0.29, 1.00] 0.01 0.1 1 10 100 Test for overall effect: Z = 6.06 (P < 0.00001) TRUST 2 2 2 66 0.50 [0.07, 0.93] 0.97 [0.90, 1.00] Favours EGFR wild type Favours EGFR mutation 0 0.2 0.4 0.6 0.8 1 0 0.2 0.4 0.6 0.8 1 Linardou H, Dahabreh IJ, Kanaloupiti D, Siannis F, Bafaloukos D, Kosmidis P, Papadimitriou CA, Murray S. Assessment of somatic k ‐ RAS mutations as a mechanism associated with resistance to EGFR ‐ targeted agents: a systematic review and meta ‐ analysis of studies in advanced non ‐ small ‐ cell lung cancer and metastatic colorectal cancer. Lancet Oncol 2008; 9 (10):962 ‐ 972
Could EGFR mutation be used in KRAS mutations in NSCLC clinical practice? • Found in: • Test varies across studies • ~ 12 ‐ 30% Caucasian • Possible confounding • ~ 5 ‐ 10% East ‐ Asian • Mostly uncontrolled studies or relatively small • More common in: subgroups of patients – History of smoking • Prognostic rather than predictive? Both? – Adenocarcinomas • Patients in whom assessment could not be carried – Caucasian out – selection bias? • Prognostic value unclear (some studies seem to • Alternative treatments? show shorter survival in patients with mutations) • Exons 2 ‐ 3, most common in exon 2 Reference list available on request Using a treatment – predictive biomarkers KRAS mutations in included studies • 5 studies (N: 83 ‐ 731) assessed KRAS mutations n o • Status known in 29 ‐ 79% r n toxicity e ‐ • 4 studies used PCR and 1 direct sequencing s r p e • Mutations assessed: o s n p – 2 studies: exon 2 d o e n KRAS mutation – 3 studies: exon 2 and 3 r d s e r s KRAS mutation – overall survival KRAS mutation – response OR (RECIST) BR.21 survival HR: erlotinib vs. placebo Survival HR: mutation vs. wild type study N HR group N ERL vs. PL 11 mutation 1.64 (0.97, TRUST 78 wild type 2.80) all patients 731 HR 0.7 (0.58, 0.85) 7 mutation 0.81 favours KRAS wild type KRAS wild type Odds Ratio Odds Ratio Felip 2008 32 wild type (NR) wild type 137 HR 0.69 (0.49, 0.97) Study or Subgroup Events Total Events Total Weight M-H, Random, 95% CI M-H, Random, 95% CI BR.21 1 20 10 98 48.3% 0.46 [0.06, 3.84] mutation 40 HR 1.67 (0.62, 4.50) Miller 2008 0 11 7 78 25.2% 0.41 [0.02, 7.76] TRUST 0 18 20 62 26.5% 0.06 [0.00, 0.98] Total (95% CI) 49 238 100.0% 0.26 [0.06, 1.12] Total events 1 37 Heterogeneity: Tau² = 0.00; Chi² = 1.63, df = 2 (P = 0.44); I² = 0% Median survival (months): all patients, KRAS mutation and wild type 0.01 0.1 1 10 100 Test for overall effect: Z = 1.81 (P = 0.07) favours KRAS wild type favours KRAS mutation median lci uci Felip 2008 all patients 4 3.4 6.4 KRAS wild type 3.7 2.9 6.8 KRAS mutation 4.5 2 7.3 Miller 2008 all patients 17 NR NR KRAS wild type 21 NR NR KRAS mutation 13 NR NR 0 5 10 15 20 25
Could KRAS mutations be used in KRAS mutation – predicting response clinical practice? Index test: KRAS mutation • Test varies across studies Reference test: lack of response • Possible confounding • Small number of studies Study TP FP FN TN Sensitivity Specificity Sensitivity Specificity BR.21 19 1 88 10 0.18 [0.11, 0.26] 0.91 [0.59, 1.00] • Mostly uncontrolled studies or relatively small Miller 2008 11 0 71 7 0.13 [0.07, 0.23] 1.00 [0.59, 1.00] TRUST 18 0 42 20 0.30 [0.19, 0.43] 1.00 [0.83, 1.00] 0 0.2 0.4 0.6 0.8 1 0 0.2 0.4 0.6 0.8 1 subgroups of patients • Patients in whom assessment could not be carried out – selection bias? • Prognostic rather than predictive? Both? • Patients with KRAS mutation should not be treated? Linardou H, Dahabreh IJ, Kanaloupiti D, Siannis F, Bafaloukos D, Kosmidis P, Papadimitriou CA, Murray S. Assessment of somatic k ‐ RAS mutations as a mechanism associated with resistance to EGFR ‐ targeted agents: a systematic review and meta ‐ analysis of studies in advanced non ‐ small ‐ cell lung cancer and metastatic colorectal cancer. Lancet Oncol 2008; 9 (10):962 ‐ 972 Conclusions • Different properties of biomarkers depending on purpose and context • Might only identify a subgroup of patients with an increased probability of (not) benefiting from treatment • Predictive vs. prognostic biomarkers • Possible confounding • Possible bias: patients who cannot be tested • Need for RCTs designed to evaluate both biomarker and treatment • Assessment across similar indications and/or drugs with similar mechanism of action?
Recommend
More recommend