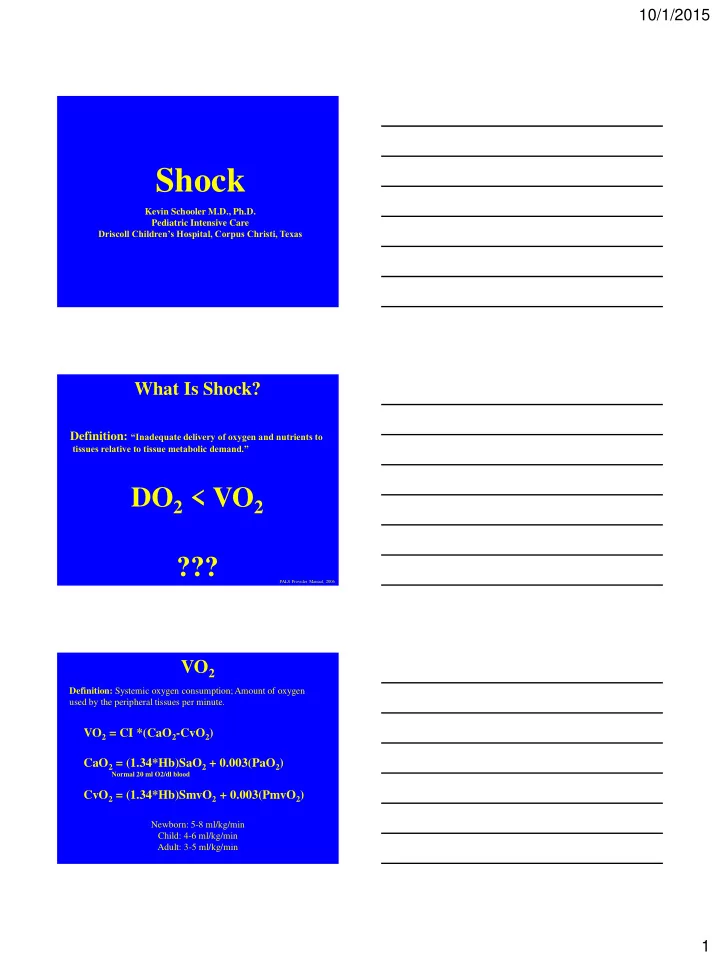
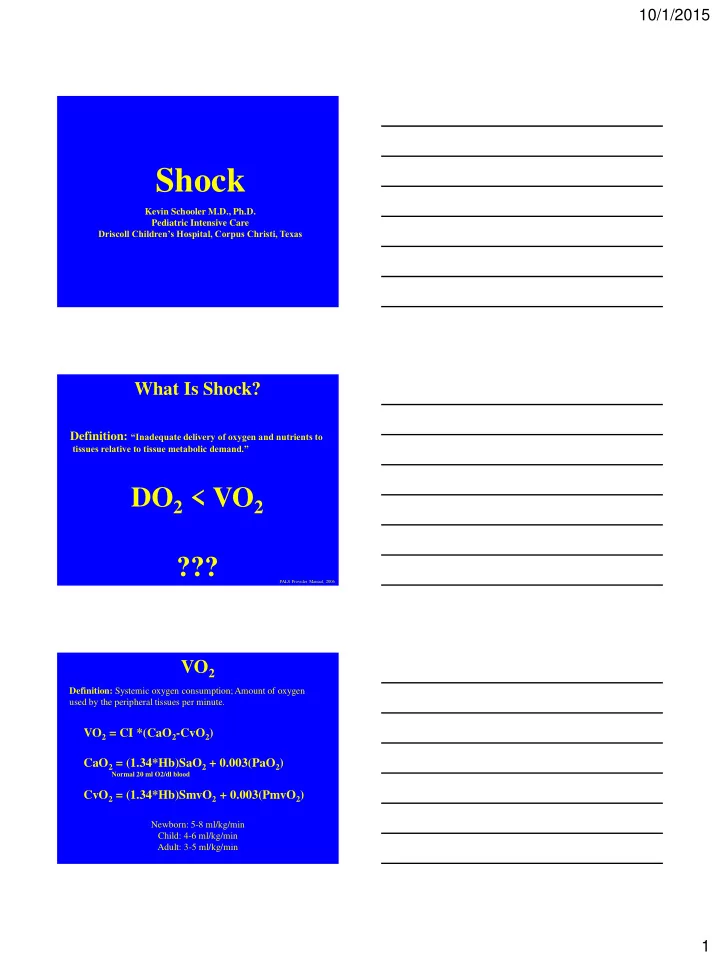
10/1/2015 Shock Kevin Schooler M.D., Ph.D. Pediatric Intensive Care Driscoll Children’s Hospital, Corpus Christi, Texas What Is Shock? Definition: “Inadequate delivery of oxygen and nutrients to tissues relative to tissue metabolic demand.” DO 2 < VO 2 ??? PALS Provider Manual, 2006 VO 2 Definition: Systemic oxygen consumption; Amount of oxygen used by the peripheral tissues per minute. VO 2 = CI *(CaO 2 -CvO 2 ) CaO 2 = (1.34*Hb)SaO 2 + 0.003(PaO 2 ) Normal 20 ml O2/dl blood CvO 2 = (1.34*Hb)SmvO 2 + 0.003(PmvO 2 ) Newborn: 5-8 ml/kg/min Child: 4-6 ml/kg/min Adult: 3-5 ml/kg/min 1
10/1/2015 DO 2 Definition: Systemic oxygen delivery; Amount of oxygen delivered to the peripheral per minute. DO 2 = CI*(CaO 2 ) CaO 2 = (1.34*Hb)SaO 2 + 0.003(PaO 2 ) Normal 20 ml O2/dl blood DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] Normal: 5 times VO 2 regardless of size Notice: BP is NOT a part of the DO 2 equation!!! Relationship Between DO 2 and VO 2 5 Increase in DO2 (A-B) or decrease in DO2 (A-C), does not affect VO2 unless DO2:VO2 drops below 2:1 (A-D) 4 VO 2 (ml/kg/min) 3 C A B 2 D 1 0 0 5 10 15 20 DO 2 (ml/kg/min) Adapted from R.H. Bartlett, “Physiology of Extracorporeal Life Support.”, ECMO Support in Critical Care, 2 nd Edition, 2000 2
10/1/2015 DO 2 < VO 2 By More Than 2:1 Translation: If tissues use (VO 2 ) oxygen faster than it is delivered (DO 2 ) the patient is in shock. So… Now What? Aerobic Glycolysis Glucose 2 Pyruvate + 2 ATP + 2 NADH Glucose G6P Pyruvate The Core Metabolic Pathway NAD + ATP Lactate Anerobic Glycolysis Glucose 2 Lactate + 2 ATP + 2 NAD 3
10/1/2015 Great. But how does that help me recognize and treat shock? Stages of Shock Compensated- Blood Pressure Maintained - end organ function not yet showing evidence of being terminally compromised Uncompensated- Blood pressure falls -end organs dysfunction becomes clinically significant Irreversible- Multi-organ failure - extensive damage that can no longer be repaired What Is Normal SBP? Newborn: SBP >= 60 1 month – 1 year: SBP >= 70 > 1 year SBP >= 70 + 2 * Age in years > 10 years SBP >= 90 Adapted from PALS Provider Manual, 2002 4
10/1/2015 What About MAP? 5 th percentile = (1.5 * years) + 40 50 th percentile = (1.5 * years) + 55 But... I thought BP was NOT a part of the definition of shock!!! Why Is Low BP A Late Sign Of Shock? Since Q = D P/SVR Then MAP a CO * SVR 5
10/1/2015 Compensated vs. Uncompensated Shock? SVR Normal MAP CO 10% 20% 30% Blood V olume Lost Adapted from PALS Provider Manual, 2002 So Let’s Change That: Stages of Shock Reversible- end organ function not yet showing evidence of being terminally compromised -BP is lost at some point Irreversible- Multi-organ failure - extensive damage that can no longer be repaired What End Organs Can We Evaluate Easily? Brain: Mental status normal? Changing? Declining? Kidneys: Urine becoming concentrated? UOP volume falling off? Skin: Warm? Cold? Capillary refill? - reflects CO Heart: Tachycardia worsening? Improving? - reflects volume status or dysfunction Lungs: Tachypnea worsening? Improving? -reflects acidosis 6
10/1/2015 Therefore: Treatment Goals “Prevent end -organ injury and halt progression to cardiopulmonary failure and cardiac arrest.” PALS Provider Manual, 2006 Lowering VO 2 Sedate: decreases pain, agitation and neurologic electrical activity Intubate: eliminating WOB, decreases CO by 20-30% Decrease Temperature: higher T is higher metabolic demand Paralyze: eliminates muscle activity What Are The DO 2 Components? Anemia Hypoxia DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] CI = CO/BSA Rhythm Preload CO = HR * SV Contractility Afterload 7
10/1/2015 Relationship Between Hb, PO 2 And O 2 Content 25 V A Hb 15 20 O2 Content (ml/dl) Hb 10 15 Hb 7.5 10 5 0 0 25 50 75 100 125 150 PO 2 Adapted from R.H. Bartlett, “Physiology of Extracorporeal Life Support.”, ECMO Support in Critical Care, 2 nd Edition, 2000 In Other Words: Doubling Hgb Will Double The DO 2 ! Shock Reversal Requires You To Know The Type Of Shock You Are Dealing With! 8
10/1/2015 Shock Classification Hypovolemic Cardiogenic Distributive Obstructive Dissociative Balanced Input and Output O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 DO 2 VO 2 O 2 O 2 Mechanisms of BP Homeostasis Blood Pressure Falls 1) Hyperacute: -Carotid and aortic baroreceptors -sense fall in blood pressure -Medullary stimulus increases Sympathetic (adrenergic) and decreases Parasympathetic (vagal) tone -HR and SVR increase to maintain BP -Acidosis sensed in carotid bodies -HR and SVR increases to improve BP -RR increases to alleviate acidosis -Serum Osmolality rises -ADH released from pituitary -SVR increases -water channels in collecting ducts close to increase volume 9
10/1/2015 Mechanisms of BP Homeostasis 2) Acute: -Decreased blood pressure causes decreased perfusion of kidney JG apparatus -Renin secretion increases -Renin cleaves Angiotensinogen to Angiotensin I -ACE cleaves Angiotensin I to Angiotensin II -Angiotensin II -Direct increase in SVR -Pituitary gland secretes ADH -SVR increases -water channels in collecting ducts close to increase volume -aldosterone secreted from adrenal cortex -sodium retained to increase volume 3) Acute: Increased water volume increases RAP -CO increases -Increased water volume increases EDV -CO increases Continued Stress Increased EDP Pulmonary Edema More volume needed etc…. Increased Ventilator Support Decreased CO Decreased Venous Return Hypovolemic Shock O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 Pipes are empty O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 VO 2 DO 2 O 2 O 2 10
10/1/2015 Hypovolemic Shock Anemia Hypoxia DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] CI = CO/BSA Rhythm Preload CO = HR * SV Contractility Afterload Hypovolemic Shock Etiology: Decrease in total circulating volume Subtypes: Hemorrhagic Shock Burns Osmotic Diuresis (DKA) Third Spacing Diarrhea/Vomiting Symptoms: tachycardia, tachypnea, cold extremities, narrow pulse pressure, prolonged CR Diagnosis: ↑ Rate ↓ Preload ↑ ↔ Contractility, ↑ Afterload Treatment: Blood, Fluid Cardiogenic Shock O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 Pump is Broken O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 VO 2 DO 2 O 2 O 2 11
10/1/2015 Cardiogenic Shock Anemia Hypoxia DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] CI = CO/BSA Rhythm Preload CO = HR * SV Contractility Afterload Cardiogenic Shock Etiology: Inadequate cardiac output Diagnosis: ↓ or ↑ Rate ↔ Preload ↓ Contractility ↑ Afterload Symptoms: tachycardia, tachypnea, cold extremities, narrow pulse pressure, prolonged CR, weak pulses diaphoresis, CHF symptoms, cyanosis Treatment: Optimization of preload, afterload, contractility, rhythm, and rate Distributive Shock O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 Pipes Are Too Big O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 O 2 12
10/1/2015 Distributive Shock Anemia Hypoxia DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] CI = CO/BSA Rhythm Preload CO = HR * SV Contractility Afterload Distributive Shock Etiology: Inappropriate distribution of blood volume Subtypes: Septic shock Anaphylactic shock Neurogenic shock Diagnosis: ↑ ↔ Rate ↓ ↔ Preload, ↓ ↔ Contractility, ↔ ↓ Afterload Symptoms: tachycardia, tachypnea, warm or cold extremities, wide or narrow pulse pressure, brisk or prolonged CR, weak or strong pulses Treatment: Fluid, vasopressor etc . Septic Shock Dellinger et al. “Surviving Sepsis Campaign: International Guidelines for Management of Severe Sepsis and Septic Shock: 2012.” Crit .Care Med . V41: 2, 2013 13
10/1/2015 Relationship Between DO 2 and SVO 2 300 DO 2 /VO 2 ratio: 2 3 4 5 SVO 2 : 50 66 75 80 240 180 VO 2 (ml) 120 60 0 0 300 600 900 1200 DO 2 (ml) Adapted from R.H. Bartlett, “Physiology of Extracorporeal Life Support.”, ECMO Support in Critical Care, 2 nd Edition, 2000 Anaphylactic Shock Epinephrine: 0.15 mg IM < 30 Kg 0.3 mg IM >30 Kg Albuterol: 0.5 mg/kg/hr Antihistamine: H1-diphenhydramine H2-ranitidine Corticosteroids: Solumedrol 1 mg/kg Neurogenic Shock Volume & Norepinephrine 14
10/1/2015 Obstructive Shock O 2 O 2 O 2 O 2 Pipes Are Clogged VO 2 DO 2 Obstructive Shock Anemia Hypoxia DO 2 = CI *[(1.34*Hb)SaO 2 + 0.003(PaO 2 )] CI = CO/BSA Rhythm Preload CO = HR * SV Contractility Afterload Obstructive Shock Etiology: Impaired CO caused by physical obstruction of blood flow Subtypes: Cardiac Tamponade Tension Pneumothorax Ductal Dependent CHD Pulmonary embolism Symptoms: tachycardia, tachypnea, cold extremities, narrow pulse pressure, prolonged CR, weak pulses Treatment: Fluid and Relief of Obstruction 15
10/1/2015 Relieve The Obstrtuction Cardiac Tamponade- emergent pericardiocentesis Tension Pneumothorax- 18-20G needle decompression, over third rib mid-clavicular line Ductal Dependent CHD- Prostaglandin E1 Pulmonary Embolus- Anticoagulants, thrombolytics Dissociative Shock Etiology: Impaired oxygen delivery despite normal heart, blood flow, blood volume and vascular tone Subtypes: Poisons (Cyanide, CO) Inborn Errors of Metabolism Abnormal hemoglobin Symptoms: tachycardia, tachypnea, acidosis Treatment: Reverse underlying cause 16
Recommend
More recommend