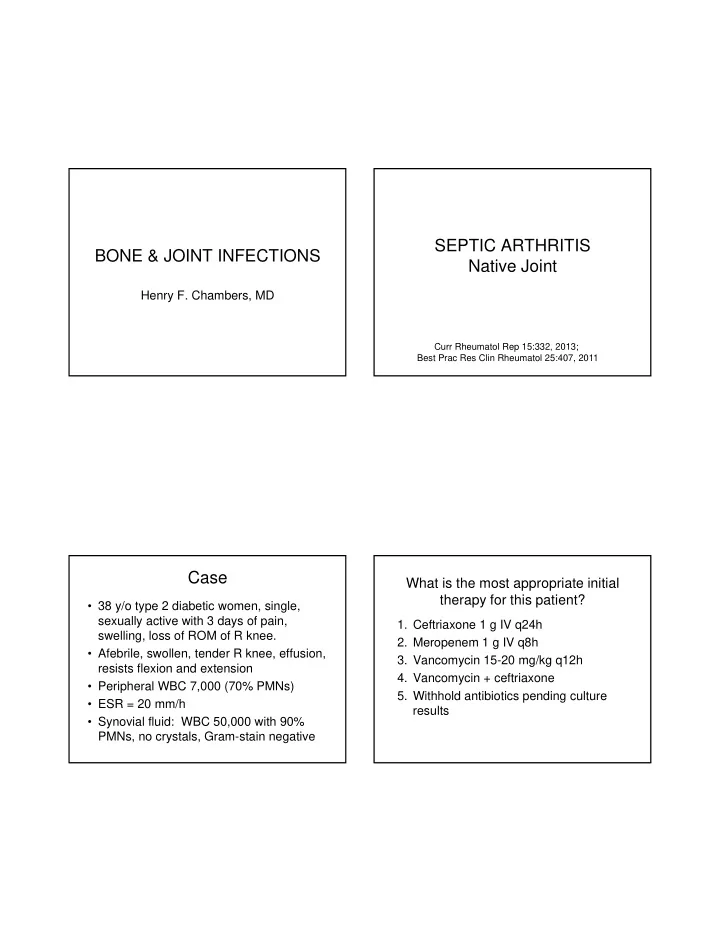
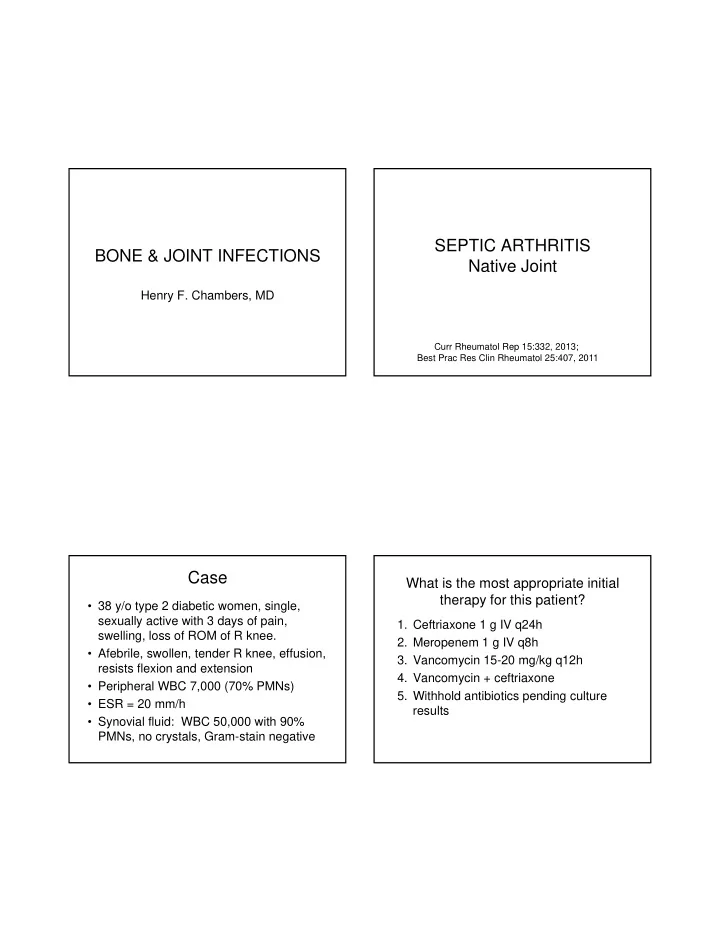
SEPTIC ARTHRITIS BONE & JOINT INFECTIONS Native Joint Henry F. Chambers, MD Curr Rheumatol Rep 15:332, 2013; Best Prac Res Clin Rheumatol 25:407, 2011 Case What is the most appropriate initial therapy for this patient? • 38 y/o type 2 diabetic women, single, sexually active with 3 days of pain, 1. Ceftriaxone 1 g IV q24h swelling, loss of ROM of R knee. 2. Meropenem 1 g IV q8h • Afebrile, swollen, tender R knee, effusion, 3. Vancomycin 15-20 mg/kg q12h resists flexion and extension 4. Vancomycin + ceftriaxone • Peripheral WBC 7,000 (70% PMNs) 5. Withhold antibiotics pending culture • ESR = 20 mm/h results • Synovial fluid: WBC 50,000 with 90% PMNs, no crystals, Gram-stain negative
Differential Diagnosis of Acute Joints Affected in Septic Arthritis in the Adult Arthritis • Infection (bacteria, fungi, mycobacteria, Hip 30-40% viruses, spirochetes) • Rheumatoid arthritis, JRA Knee 40% • Crystal arthropathy (gout, pseudogout) Ankle 5-10% • Reactive arthritis, adult Still’s • Systemic lupus erythematosis Wrist, elbow, hand 10-15% • Osteoarthritis Multiple joints 5-10% • About 10 other things Microbiology of Septic Arthritis Septic Arthritis: Presentation Children Adults • Staph. aureus (40- • Staph. aureus (40- Joint Pain 85% 60%) 60%) • Streptococci (30%) • Streptococci (30%) History of joint 78% – S. pneumoniae – GAS swelling – GAS – S. pneumoniae • Gram-negative • Gram-negative Fever 57% bacilli (5-20%) bacilli (5-20%) – H. influenzae rare – Enterics • Neisseria sp. • Neisseria sp. Margaretten, et al. JAMA 297:1478, 2007 Culture-negative: 15-30%
Risk Factors for Septic Serum Lab Values Arthritis Factor Likelihood Ratios Factor Likelihood Ratios Positive Negative Positive Negative Diabetes 2.7 0.93 WBC > 10,000 1.4 0.28 Recent joint 6.9 0.78 surgery ESR > 30 mm/h 1.3 0.17 Hip or knee 15.0 0.77 prosthesis + skin CRP > 100 mg/L 1.6 0.44 infection RA 2.5 0.45 Margaretten, et al. JAMA 297:1478, 2007 Margaretten, et al. JAMA 297:1478, 2007 Initial Management Of Acute Synovial Fluid Studies Septic Arthritis Factor Likelihood Ratios • Drain the joint (controversy as to which is better) Positive Negative – Arthrocentesis (knee, ankle, elbow, wrist, hand) – Arthroscopy (hip and shoulder) WBC > 100,000 28 0.75 – Open drainage (hip and shoulder) • Obtain cultures WBC > 50,000 7.7 0.42 – Blood (~30% to 50% positive) – Synovial fluid, aerobic and anaerobic (consider fungal WBC > 25,000 2.9 0.32 and mycobacterial if subacute/chronic presentation) – STD risk, or polyarticular signs and symptoms, rash: PMNs > 90% 3.4 0.34 culture blood, fluid, rectum, cervix/urethra, throat for GC Margaretten, et al. JAMA 297:1478, 2007
Initial Antimicrobial Therapy of Disseminated Gonococcal Septic Arthritis Infection • Synovial fluid crystals: withhold antibiotics • Gram stain positive – Gram-positive cocci: Vancomycin 15-20 mg/kg q8- 12h for suspected S. aureus , strep – Gram-negative cocci: Ceftriaxone 1 g q24h – Gram-negative bacilli: Cefepime 2 gm q8h, meropenem 1 gm q8h, or levofloxacin 750 mg q24h • Gram-stain negative – Vancomycin 15-20 mg/kg q8-12h + ceftriaxone 1 g q24h (or as above for Gram-negative bacilli) Initial Therapy of Culture-Positive Duration of Therapy Septic Arthritis • Gonococcal septic arthritis: 7 days • Staphylococcus aureus • Septic arthritis in a child – MSSA: cefazolin 2 g q8h or nafcillin 2g q4h – MRSA: vancomycin 15-20 mg/kg q8-12h – 2 weeks (3 weeks if accompanying osteo) (Ped Clin NA 60:425, 2013) • Streptococci – 10 days of therapy probably as effective as a 30- – Pen G 2 mU q4h or ceftriaxone 2 g q24h day treatment course (Clin Infect Dis 48:1201, • Gonococci 2009) – Ceftriaxone 1 g q24h (plus azithro, doxy, FQ for • Septic arthritis in an adult: 2-4 weeks chlamydia) • May be a combination of IV (typically ~ 3-7 • Gram-negative bacilli days) and oral therapy – See previous slide and based on results of susceptibility testing
Outcomes in Children Outcomes in Adults • CRP normalizes in 9-10 days • CRP should normalize in 9-10 days – Faster resolution in those with needle (longer if arthrotomy performed) aspiration versus more invasive drainage • WBC and ESR not useful for f/u procedure • WBC and ESR not useful for f/u • Relapse or recurrence rare (<1%) • Relapse or recurrence rare (<1%) • Except for GC duration of therapy • Clindamycin and 1 st generation ceph poorly defined, recommendations vary with similar efficacy Clin Infect Dis 48:1201, 2009; Clin Micro Infect 18:582, 2011 Oral Regimens Agent Comments Clindamycin 40 mg/kg/d Children, max dose 450 mg qid SEPTIC ARTHRITIS 1 st gen ceph 150 mg/kg/d Children, max dose 1 g qid Prosthetic Joint Infection (PJI) FQ (e.g., cipro 750 mg bid, levo Adult, susceptible Gram-neg. 750 mg q24h, moxi 400 mg qd) SMX-TMP (10-15 mg/kg/d) Susceptible Gram-neg. SMX-TMP + rifampin 300 mg bid Susceptible MRSA, MSSA FQ + rifampin 600 mg/d Adult, susceptible MRSA, MSSA Clin Infect Dis 56:e1, 2013; Tsai et al, J Micro Immunol Infect, 2013 Amox-clav, linezolid, doxycycline Limited data J Antimicrob Chemother 65 (Suppl 3): iii45), 2010 Clin Infect Dis 56:e1, 2013; J Antimicrobi Chemother 69:309, 2014
Diagnosis of PJI Microbiology of PJI • Orthopedic referral for Organisms Rate Comment – Sinus tract or persistent drainage – Acutely painful prosthesis MSSA, MRSA 20-40% Typically early (w/in 3 mo) or late – Chronically painful prosthesis (> 2 years post implantation) • ESR, CRP, blood cultures, arthrocentesis Coag-neg. staph 30-40% Typically delayed or late – Stop if no evidence of infection Strep, enterococci, 10-20% Also diphtheroids, P. acnes – Suspected infection: Intraoperative Gram-neg. bacilli 10-15% Enterics, Ps. aeruginosa exploration for cultures, path, debridement Culture-negative 15-20% Hate that! – Avoid empirical therapy if at all possible Orthopedic Device Related Infections Orthopedic Device Related Infections Cumulative Treatment Failure Rate Cumulative Treatment Failure Rate Ferry et al. Eur J Clin Microbiol Infect Dis 29:171-80, 2009 Ferry et al. Eur J Clin Microbiol Infect Dis 29:171-80, 2009
Total Knee/Hip S. aureus Infections IDSA Prosthetic Joint Infection Cumulative Treatment Failure Rate Treatment Guidelines FQ + rif • Obtain cultures prior to starting Rx • Treatment based on surgical option chosen other – Debridement, hardware retention – 1-stage, direct exchange – 2-stage debridement later re-implantation Clin Infect Dis 56:e1, 2013 Senneville, et al. Clin Infect Dis 53:334, 2011 Device Retention vs Removal Synopsis of IDSA Treatment Guidelines • Prosthesis retained – Staph: use iv/po rif combo for 3-6 mo – Others: iv/po regimen for 4-6 weeks • 1-stage procedure – Staph: use iv/po rif combo for 3 mo – Others: iv/po regimen for 4-6 weeks • 2-stage procedure – Staph: use iv/po rif combo for 4-6 weeks – Others: iv/po regimen for 4-6 weeks
Positive PCR Results in Culture- Culture-Negative Osteoarticular “Infections” negative Cases* • Prospective study, 3840 bone and joint samples from 2308 patients Organism % positive (N = 141) – Marseille University Hospitals, 2007-09 – 50% had prosthetic devices • PCR (16S) performed on culture-neg specimens Fastidious organisms 25 • Culture results Staph. aureus § 25 – Positive: 33.1% (S. aureus [33%], CoNS [21%], Gram-neg Coag-neg. staph. 21 bacilli [23%] Strep/enterococci [13%] Streptococci, enterococci 16 – Negative: 67.9% Gram-negative bacilli 11 • PCR results – 6.1% of all patients PCR positive § 65% neg on repeat PCR * Prior antibiotic in 42% of cases – 9.1% of culture-neg cases PCR positive Levy, et al, Am J Med 126:e25, 2013 Causes of Culture-negative Oral Regimens for Osteoarticular “Infections” Culture-negative Septic Arthritis • Non-infectious cause Antibiotic Comments • False-negative culture Moxifloxacin Misses some MRSA, MRCNS, some GNB – Low inoculum infection, sampling error Clindamycin Misses GNRs, fastidious Gram-negs, enterococci, few to some MRSA – Prior antibiotics – Fastidious organisms Augmentin Misses MRSA, MRCNS, resistant GNB • Other organisms: fungi, MTB, other SMX-TMP Misses enterococci, some GNB, anaerobes mycobacteria, brucella, nocardia Linezolid Misses GNBs, anaerobes
Recommend
More recommend