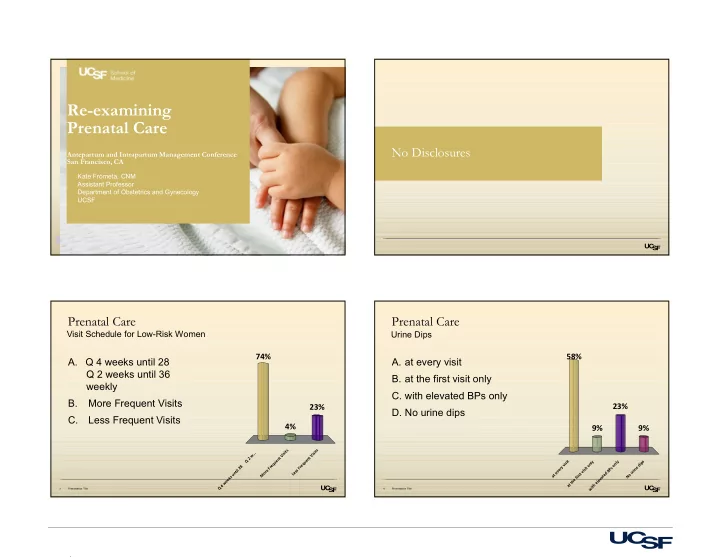
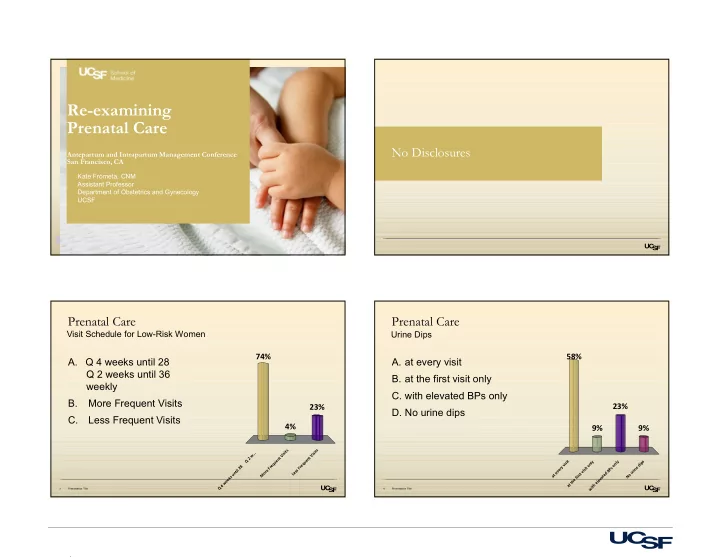
Re-examining Prenatal Care No Disclosures Antepartum and Intrapartum Management Conference San Francisco, CA Kate Frómeta, CNM Assistant Professor Department of Obstetrics and Gynecology UCSF Prenatal Care Prenatal Care Visit Schedule for Low-Risk Women Urine Dips 74% 58% A. Q 4 weeks until 28 A. at every visit Q 2 weeks until 36 B. at the first visit only weekly C. with elevated BPs only B. More Frequent Visits 23% 23% D. No urine dips C. Less Frequent Visits 4% 9% 9% s s t t i i . s s . . i i w V V t t 2 n n Q e e t y y s u u i p q s n l l q i n i e e v o o d 8 r r y e 2 F F t s r i P n e s i l e s i B i t r s v v r n e e u o t d u M L t s e o a r t N s i k f a v e e e e h l w t e t h 4 a t Q i w 3 Presentation Title 4 Presentation Title 1
Prenatal Care History of Prenatal Care Integration of Support Services A. Routinely have women see a provider 73% Adolphe Pinard and midwife who is not an OB or Midwife or Family Madame Bequet Practice MD/NP. - Refuge de L'Avenue du Maine B. Only see another type of provider if 1892 27% indicated . . . . . . e r p e s f o n e e m p y o t w r e e h v t a o h n a y e e l e n s i t y u n l o O R 5 Presentation Title 6 Presentation Title History of Prenatal Care History of Prenatal Care: US First models out of Europe in early 20 th century Children’s Bureau started in 1912 By 1930: UK ministry of health - Focused on preventing infant mortality - PNV at 16, 24, 28, then q 2 w until 36 then weekly - Promotion of the idea of prenatal care - Measure fundal height at 32 and 36 weeks in the European model - Fetal heart rate monitoring and urine testing q visit “More Ritualistic than Rational” 7 OB/Anesthesia Symposium 8 Presentation Title 2
Reasons for PNC Our Failures Decrease LBW through nutrition/substance abuse intervention Identifying infectious disease US Obstetric care is the most expensive in the world Identify Rh negative mothers and give Rhogam as needed Identification and rectification of breech presentation One of the highest rates of both infant and maternal mortality of Identification of preeclampsia to decrease eclampsia industrialized countries Identification and treatment of severe anemia Assure appropriate delivery setting Major opportunities for improvement - Anomalies, breech, preterm Build trust, anticipatory guidance ETC. ETC. ETC. 9 OB/Anesthesia Symposium 10 Presentation Title Quantity: Difficulty of Assessing Prenatal Care Schedule of Visits Never studied before implementation US standard: Considered standard of care therefore RCT are not a Possibility - First visit in 1 st trimester Relationship between care seeking and other positive health - f/u q 4 weeks until 28 then q2 until 36 then weekly (13-14) behaviors - ACOG “frequency of obstetric visits should be individualized” Measuring quantity vs quality NICE guidelines: - content, provider, setting - First visit before 10 weeks - f/u at 16, 25 , 28, 31,34, 36,38,40,41 WHO (2016) - 8 visits = adequate prenatal care - first 12 weeks - f/u at 20, 26, 30, 34, 36, 38 and 40 weeks’ gestation. 11 OB/Anesthesia Symposium 12 OB/Anesthesia Symposium 3
UCSF Schedule Of Prenatal Care Visits US Expert Panel on Prenatal Care (1989) First visit in 1 st trimester 8 visits for multip, 10 for primip Q 6 weeks until 28 weeks - Including preconception visit Q 4 weeks until 36 weeks More integration of support services “team approach” Q 2 weeks * Individualized to risk status* Antenatal Testing Eliminate “Visits that are not meaningful are counterproductive” 9-10 visits 13 Presentation Title 14 OB/Anesthesia Symposium Quantity Of Visits: Quantity Of Visits: Standard vs. Reduced Visit Schedule Standard vs. Reduced Visit Schedule McDuffie et al. (1996) JAMA RCT N=2764 Binstock and Wolde-Tsadik (1995) and Walker and Koniak-Griffin (1997) 9 for primips, multips 8 (+ 1 phone call at 12 weeks) vs. 14 - Smaller sample sizes (n=549, 81), both in CA, homogenous populations - No difference: - White, highly educated, women PTB - Latina women on Medicaid attending a birth center LBW PreE - ~8 visits vs. 11-14 C/S - No change in perinatal outcomes Satisfaction (reduced more likely to rate # of visits as “just right”) - greater satisfaction with reduced visits 15 OB/Anesthesia Symposium 16 Presentation Title 4
Quantity Of Visits: Quantity Of Visits: Standard vs. Reduced Visit Schedule Standard vs. Reduced Visit Schedule Sikorski et al (1995) - n=2794 (reduced =6-7 vs 13) 2015 Cochrane Review randomized/cluster-randomized - Fewer ultrasounds and antenatal admissions 7 trials, n=60,000 Reduced vs Standard PNC - Less suspicion of IUGR (no difference in diagnosis of IUGR) High, medium and low-income countries - No change in perinatal outcomes (PreE, IOL, C/S, SGA, PPH etc) High Income - Less satisfaction - Reduced = 8-12 visits (13-14 in regular schedule ~ 3 less) Low and middle income - Reduced = 4-5 visits (regular schedule about 7 ~2-4 less) Dowswell et al. (2015) 17 Presentation Title 18 OB/Anesthesia Symposium Quantity of Visits: Quality Of Visits: Standard vs. Reduced Visit Schedule Components of Prenatal Care No difference between groups BP - Maternal mortality Fundal Height - Hypertensive d/o FHR auscultation - PTB Urine Dip - SGA Warning signs Perinatal mortality Questions/Anticipatory - Associated with reduced visits in low and middle income countries Guidance - No difference in high income countries Satisfaction 19 OB/Anesthesia Symposium 20 OB/Anesthesia Symposium 5
Fundal Heights Fundal Heights Sparks et al, 2011 Vasilly Sutugin St. Petersberg 1875 - Retrospect cohort - Fundal height to determine gestational age/length - N=3627, u/s for abnormal fundal height = 448 Alfred Baker Spalding, Stanford 1904 “Measure….the height of the fundus above the symphysis in Sensitivity LGA (>90%) 16.6% SGA (<10%) 17.3% cm….and add two to measurements between 22 and 26 cm, - Lower for overweight/obese women three to measurements between 26 and 30, four to - Higher for multips measurements between 30 and 32 and five to measurements above 32, which sum will equal the probable week of Specificity 94.9-95.4% LGA and SGA 92.4-93.1% pregnancy” - Outcomes occurred about 10% of the time 21 OB/Anesthesia Symposium 22 OB/Anesthesia Symposium Assessing Fetal Growth Fundal Height WHO 2016 ? 3 rd trimester u/s - Sensitivity 46-93% for SGA and 6.7-89% for LGA NICE says no 3 rd trimester u/s for LGA in “low-risk” population. Replacing abdominal palpation with symphysis-fundal height (SFH) Customized growth charts measurement for the assessment of fetal - (GROW software – UK, endorsed by RCOG) growth is not recommended to improve perinatal outcomes. A change from what - Ethnic/racial and gender differences (NICHD, WHO) is usually practiced (abdominal palpation Deter-Rossavik model or SFH measurement) in a particular - Base 3 rd tri growth on 2 nd tri growth (u/s) setting is not recommended 23 OB/Anesthesia Symposium 24 OB/Anesthesia Symposium 6
Fetal Heart Rate Auscultation Urine Dips Protein In the US is standard of care at every visit (appropriate to - Proteinuria common in pregnancy 10-40% (≥+1) gestational age) - Protein dipstick has ppv of PreE of 2-11% - High false positive when compared to 24 hr urines NICE (UK) recommends against fhr auscultation at routine visits New Guidelines place less emphasis on proteinuria - “Auscultation of the fetal heart may confirm that the fetus is alive but is unlikely to have any predictive value and routine listening is therefore Glucose not recommended.” - False positive 11: 1 - Glucose loading test much better Alto, W (2005) 25 OB/Anesthesia Symposium 26 OB/Anesthesia Symposium Urine Dips “The time-honored inclusion of routine urine dipstick assessment for all pregnant women can be modified…In the absence of risk factors….there has not been shown to be a benefit in routine urine dip- stick testing” ACOG GUIDELINES FOR PERINATAL CARE, 2017 - 28 OB/Anesthesia Symposium 7
Innovations Innovations OB Nest (HCD) Centering Pregnancy http://centerforinnovation.mayo.edu/files/2016/05/ob-nest-experiment-report.pdf - CHI Butler Tobah et al, (2016) Expect with me - RCT, N=150 - United Health 8 office and 6 RN phone visits vs. 12 office visits BabyScripts - RN moderated online community - Home weight and BP monitoring Nest = greater satisfaction, OB Nest less pregnancy-related stress - Mayo Clinic No difference: - Maternal/fetal outcomes - Unplanned visits - Perceived quality of care 29 OB/Anesthesia Symposium 30 OB/Anesthesia Symposium Thank You Innovations OB Nest Now Go Innovate! Self-Monitoring (home and drop-in) Telemedicine Text-based communication Online community “The intent behind the design is (to)...anticipate (patients’) needs and provide access to reassurance in a way that fits patients’ lives. The place of care becomes home based instead of clinic based, and the pregnant woman is no longer a passive recipient of care but instead an engaged partner” 31 Presentation Title 32 Presentation Title 8
9
Recommend
More recommend