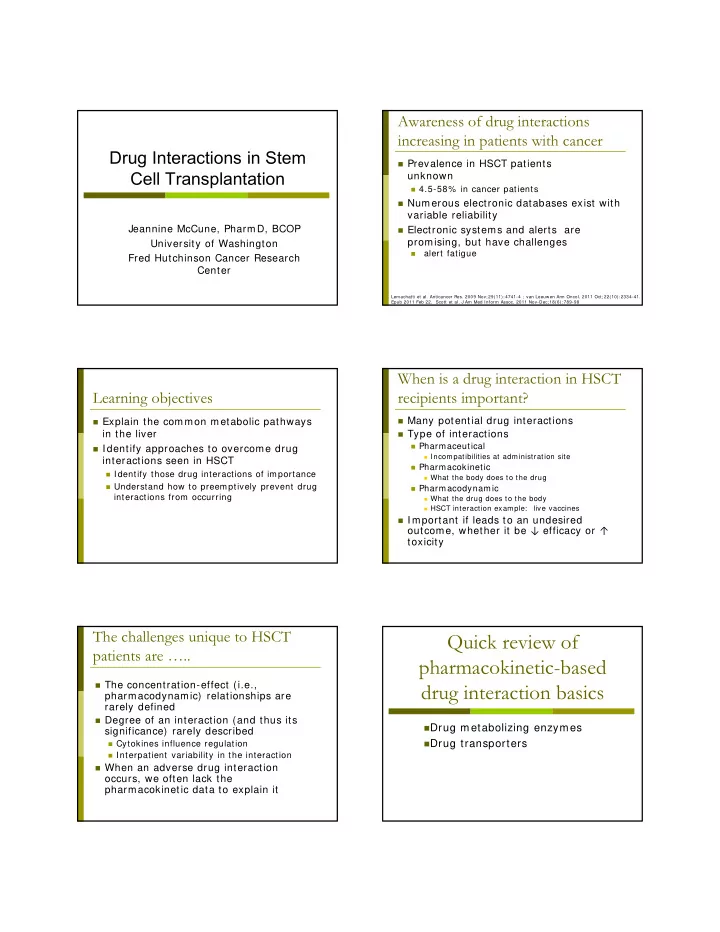
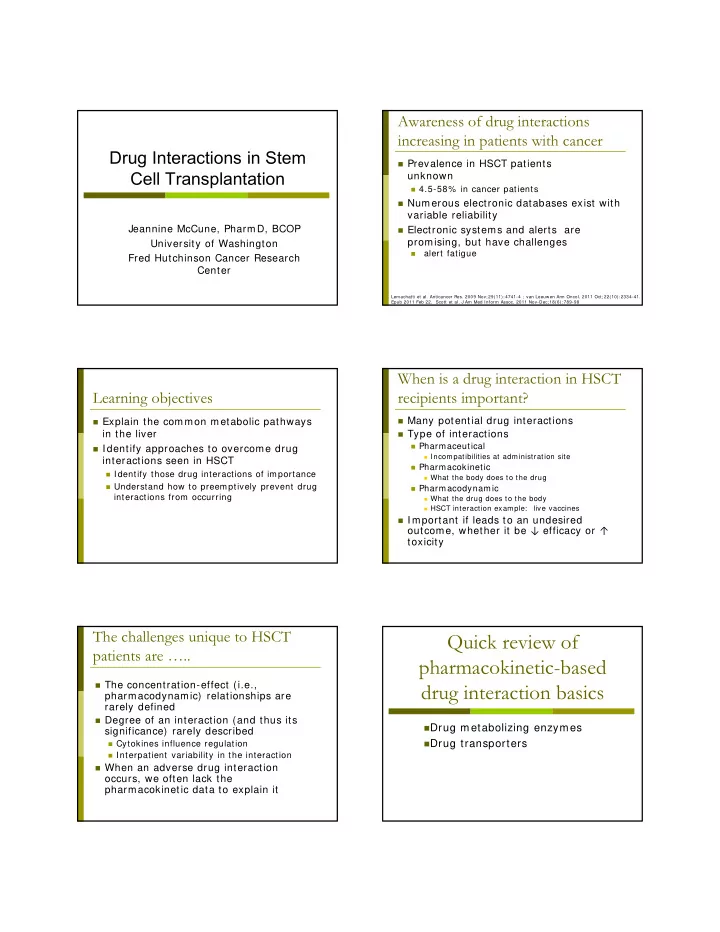
Awareness of drug interactions increasing in patients with cancer Drug Interactions in Stem Prevalence in HSCT patients Cell Transplantation unknown 4.5-58% in cancer patients Numerous electronic databases exist with variable reliability Jeannine McCune, PharmD, BCOP Electronic systems and alerts are promising, but have challenges University of Washington alert fatigue Fred Hutchinson Cancer Research Center Lemachatti et al. Anticancer Res. 2009 Nov; 29(11): 4741-4 ; van Leeuwen Ann Oncol. 2011 Oct; 22(10): 2334-41. Epub 2011 Feb 22. Scott et al. J Am Med Inform Assoc. 2011 Nov-Dec; 18(6): 789-98 When is a drug interaction in HSCT Learning objectives recipients important? Many potential drug interactions Explain the common metabolic pathways in the liver Type of interactions Pharmaceutical Identify approaches to overcome drug Incompatibilities at administration site interactions seen in HSCT Pharmacokinetic Identify those drug interactions of importance What the body does to the drug Understand how to preemptively prevent drug Pharmacodynamic interactions from occurring What the drug does to the body HSCT interaction example: live vaccines Important if leads to an undesired outcome, whether it be ↓ efficacy or ↑ toxicity The challenges unique to HSCT Quick review of patients are ….. pharmacokinetic-based The concentration-effect (i.e., drug interaction basics pharmacodynamic) relationships are rarely defined Degree of an interaction (and thus its Drug metabolizing enzymes significance) rarely described Cytokines influence regulation Drug transporters Interpatient variability in the interaction When an adverse drug interaction occurs, we often lack the pharmacokinetic data to explain it
Relationship between pharmacokinetics and Pharmacology is multifactorial pharmacodynamics Can affect both the pharmacokinetics and Dose pharmacodynamics Absorption Distribution Factors include… Metabolism Age Excretion Sex Total serum concentration Receptor Site Ethnicity Weight Unbound serum concentration Pharm acologic Condition being treated Response Protein Bound Concentration Pharmacogenetics Therapeutic Idiosyncrasy Outcom e Drug interaction Slide courtesy of Gail Anderson, PhD Pharmacokinetic parameters: Pharmacokinetic parameters elimination Absorption Metabolism The rate at which a drug leaves the site of Predominately liver administration and the extent to which it Other sites: kidney, lung, gastrointestinal occurs tract (GI), plasma HSCT interaction example: proton pump HSCT interaction example: many inhibitors with mycophenolate mofetil Distribution Excretion Process of reversible transfer of a drug to and Kidneys and hepatic/ GI tract from the site of measurement Other sites: milk, sweat, saliva, tears HSCT interaction example: non-steroidal anti- HSCT interaction example: cyclosporine with inflammatory drugs (NSAIDs) with mycophenolic acid methotrexate (also interacts at kidney) Biotransformation (Metabolism) Phase I metabolism Theory Oxidation, reduction, hydrolysis Drug inactivation Cytochrome P450 family of enzymes Increased elimination from the body 7 primary enzymes responsible for majority of drug metabolism Reality Can predict drug interactions based on Metabolites may have biological activity; knowledge of metabolizing enzymes similar or different than parent Various family, subfamily, individual genes May contribute to toxic and/ or beneficial CYP1A2, CYP2A6, CYP2C9, CYP2C19, CYP2D6, effects CYP2E1, CYP3A4/ 5 Example: Cyclophosphamide metabolized by Inhibition CYP, concentration, dose cytochrome P450 (CYP) to Induction CYP, concentration, dose 4hydroxycyclophospham ide
Cytochrome P450 (CYP) enzyme system Examples of important CYP in HSCT Large (but not only) source of drug interactions Drug Substrate Reaction Cyclosporine 3A4/ 5 Elimination Many in vitro methods to identify which “ Tacrolimus 3A4/ 5 CYP metabolizes a drug, and potential drug “ Sirolimus 3A4/ 5 interactions “ Prednisone 3A4/ 5 However, magnitude of drug interaction “ Dexamethasone 3A4/ 5 difficult to predict Cyclophos- 2C9, 2C19 Activation to 4hydroxyCY (HCY) ‘Cocktail’ studies in healthy volunteers phamide (CY) 2 2B6, 3A4/ 5* Cytokines (e.g., IL6) affect CYP 3A4/ 5 Detoxification to dechloroCY Hebert. Metabolic Drug Interactions 2000; Shimada Transplant International 2003. Ren Cancer Research 1997; Huang Biochem Pharmacol 2000; Qiu Clin Pharm Ther 2004 Phase II metabolism Phase II: Relevant conjugation reactions Glutathione S -transferase Term coined to represent metabolism Mediate conjugation of electrophilic occurring after oxidation, reduction or compounds to glutathione hydrolysis associated with bioactivation Important detoxifying pathway for alkylating Many drugs don’t require Phase I metabolism agents Functional group created conjugated to less Glucuronidation toxic or inactive compound Most common conjugation reaction for drugs UGT (UDP-glucuronosyl transferase) Conjugation of endogenous substances, bilirubin, mycophenolic acid, morphine ABC transporters relevant to HSCT Drug transporters patients Transporter Substrate Of the 400 transporters in the human genome, 30 are relevant to ABCB1 (MDR1)* calcineurin inhibitors, sirolimus pharmacokinetics corticosteroids ABCC1 (MRP1) methotrexate ATP-binding cassette (ABC) superfamily ABCC2 (MRP2) cyclophosphamide metabolite Relevant to systemic mycophenolic acid pharmacokinetics and ABCC3 methotrexate intracellular transport ABCG2 (BCRP) etoposide, topotecan * codes for pglycoprotein (pgp) Endres et al. Eur J Pharm Sci. 2006 Apr; 27(5): 501-17
Additional transporters Excretion Organic anion transporting polypeptide (OATP) Drugs are eliminated from the body methotrexate, opioids, corticosteroid metabolites unchanged or as metabolites Organic anion transporters (OAT) Complex, for example renal excretion beta-lactams, metabolites of corticosteroids, NSAIDs involves Equilibrative nucleoside transporter 1 (ENT) Glomerular filtration fludarabine Active tubular transport Concentrative pyrimidine-preferring nucleoside Passive tubular absorption transporter 1 (CNT) fludarabine HSCT interaction example: NSAIDs inhibit renal tubular secretion of methotrexate and/ or reduce renal blood flow by inhibiting prostaglandin synthesis Zhang et . Clin Pharmacol Ther. 2011 Apr; 89(4): 481-4; Pauli-Magnus Pharmacogenetics 2003; 13: 189; Sekine Annals of Oncology 2001; 12: 1515; Oleschuk Am J Physiol Gastrointest Liver Physiol 2003 Feb; 284(2): G280; Elimination half-life Pharmacokinetic parameters Example: Plasma Concentrations Drug with T 1/2 = 12 hrs Clearance measures body ’ s ability to Dose 100 mg 200 mg eliminate drugs C 0 20 g/ ml 40 g/ ml Elimination half-life is time it takes for the amount of drug in the body to be reduced by C 12hr 10 g/ ml 20 g/ ml 50% C 24hr 5 g/ ml 10 g/ ml T 1/ 2 = 0.693• Vd Cl C 36hr 2.5 g/ ml 5 g/ ml where Vd = volume of distribution and C 48hr 1.2 g/ ml 2.5 g/ ml Cl = total body clearance Impact of CYP interactions on clearance C 60hr < 1 g/ ml 1.2 g/ ml Inhibition CYP, clearance, concentration, dose C 72hr < 1 g/ ml < 1 g/ ml Induction CYP, clearance, concentration, dose Slide courtesy of Gail Anderson, PhD Approximate half-lives of relevant Steady state immunosuppressants Calcineurin inhibitors: 11-35 hours (hr) Css = the concentration at which the rate of drug input is equal to the rate of drug elimination Sirolimus: 62 hr Can be defined as area under the curve/ dosing interval (busulfan) Mycophenolic acid: 0.6-11.9 hr Takes approximately 5 T 1/ 2 to reach steady state Methylprednisolone, prednisone: 1.7 to 4.1 hr Take approximately 5 T 1/ 2 to completely eliminate a drug after discontinuation Css is dependent on dosage and clearance
Recommend
More recommend