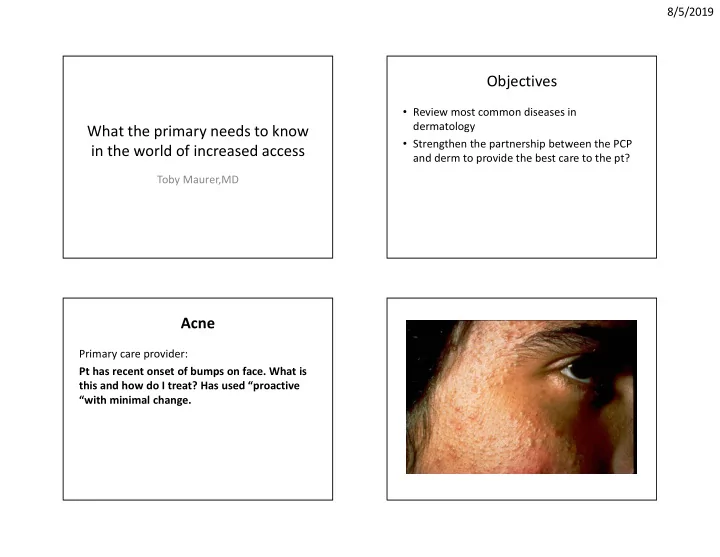
8/5/2019 Objectives • Review most common diseases in dermatology What the primary needs to know • Strengthen the partnership between the PCP in the world of increased access and derm to provide the best care to the pt? Toby Maurer,MD Acne Primary care provider: Pt has recent onset of bumps on face. What is this and how do I treat? Has used “proactive “with minimal change. 1
8/5/2019 Topicals Primary Care Provider: Pt with acne –used Retin -A but very • BP 5% gel (10% - more drying) irritating. What is the next step? • Retin A 0.025% - 0.1% ( vehicle determines strength - start with crème) • Cleocin T or erythromycin topically – Use 1 qam and 1qhs – If NO success after 8 weeks, go to p.o.’s • Pt has cystic/scarring acne-topicals won’t work and in Asians-Retin A is very irritating. • Start p.o. antibiotics • Adapaline-topical agent that may shrink scars 2
8/5/2019 P.O. Antibiotics • TCN - 500 bid x 8 weeks • Doxycycline - 100 bid x 8 weeks • Minocycline - 100 bid x 8 weeks • Taper - Do NOT STOP ABRUPTLY. Once pt’s skin is clear, taper the dose in ½ for another month and then stop the medication Scarring, keloidal, cystic acne • Record treatments • If failed 2 or more systemic meds, consider Accutane • Check depression history, CBC, LFT’s, TG, Chol and pregnancy counselling 3
8/5/2019 Acne Rosacea • Rosacea-if just red-laser or makeup • If papules-start doxy 100 bid x 8 wks then topical flagyl daily for maintenance • Seb derm: topical HC 1% oint plus econazole crème bid and seb derm shampoo (tar, ketaconazole,selenium, zinc) Acne Keloidalis Nuchae • Never buzz cut hair again • Primary Care Provider: • Topical clobetasol qam and topical retin a 0.1% Pt told he has psoriasis-used some crème in crème/gel qhs x 3 months Mexico-can’t remember name. Worried that his • If very inflamed, add doxycyline 100 bid x 2 months grandchildren could catch this. • See pt back in 3 months • If no change, send back another consult-we can book him in clinic for intralesional kenalog • New association with metabolic syndrome (especially HTN) 4
8/5/2019 • Psoriasis is fast growing skin-can’t get it from anyone and can’t give it to anyone • What meds is he on? Certain meds might unmask this like atenelol, lithium, NSAIDS • Start Clobetasol oint and dovonex crème together. Apply M-F bid-weekends off • Primary see pt again in 6 weeks. If not better-send another telederm consult and we will readvise or book pt in derm clinic Pt did not get better…… Psoriasis-when topicals don’t work • New pictures show increased total body • Acitretin -safer to use in liver disease-monitor TG, Chol surface area involvement • Methrotrexate- titrate dose, follow LFT’s and CBC, • Dermatology triage: I see that pt has liver needs liver biopsy after 1.5 gm-great drug if there disease (seen on EMR). First choice systemic is psoriatic arthritis drug is acitretin. Please order up baseline • Biologics -good drugs, expensive, subcu injections LFT’s , fasting TG and cholesterol. except for ompremilast, presecreen for TB and • We will book pt for derm clinic in 3 weeks- Hep B and cancer risk please order baseline labs and start him on • Ultraviolet light -is pt able to spend the time; is it acitretin 25 qd accessible to pt? 5
8/5/2019 Psoriasis and Metabolic Syndrome NO PREDNISONE • associated with HTN and cardiac disease • associated with renal disease • Chronic inflammation-no evidence that the TNF blockers or aictretin are helpful in down regulating systemic inflammatory markers • Did not check against MTX 6
8/5/2019 Atopic Dermatitis Body Treatment • Topical steroids and antihistamines still mainstay of treatment • Avoid prednisone (oral and injectable) • Clobetasol ointment qd for 5 days when severe then • Fluocininide (lidex) oint bid for 2 weeks then • Triamcinolone 0.1 % oint bid maintenance • FACE: HC or aclomethasone oint bid Gentle Skin Care discussion • Steroids are okay to use-not going to thin out the skin BUT give limited amts of potent steroids • Use steroids with grease-bid when disease is active • Otherwise JUST GREASE • Bathing or showering 1-2x’/wk and don’t even dry off after bathing • Grease up immediately • Antihistamine (benadryl, atarax, doxepin) at night so pt can sleep and break the itch/scratch cycle 7
8/5/2019 Dupilumab • Anti-IL4 receptor • Expensive • SEVERE atopic derm Scabies: Classic treatment • Permethrin 5% crème-2 applications 1 week apart • Must treat all intimates • Clothing instructions essential-wash 3 days of clothing and linens, then apply permethrin- start using clean clothes next morning • Everything else goes into garbage bags-tie off for 3 days 8
8/5/2019 • Primary Care Provider: Pt notes changing mole-also itchy. Worried she has melanoma • Seborrheic keratosis-OBSERVE over time-Alert to pt-if bleeds or grows rapidly-return to you ASAP! • You can apply cryotherapy 2 x 15 sec thaw cycles or • Private derms in your county will do this for a fee 9
8/5/2019 • Primary Care Provider: • Teledermatology Response: 24 year old with new black bump Looks like seb keratosis but that is unusual in pt under the age of 29. I want to biopsy this • No others noted • We will contact pt for next live derm clinic • Cc scheduler-book for live derm in 1 week • Pt notes these get caught on shirt-sometimes get inflamed 10
8/5/2019 • Skin tags-benign • Primary can snip them off-services not covered by county New red/brown bump • Primary Care Provider: • Dermatofibroma-often on arms and legs of women 30 yr old with multiple previous biopsies to rule out melanoma. Here for skin check. • Banal-reaction to bug bite or trauma • No recent changes in moles • Resolves in 20 yrs • No family history of melanoma • Don’t excise • Please see in live derm clinic • Teledermatology response: Agree and will book within 1-2 months 11
8/5/2019 Melanoma • Melanoma may be INHERITED or occur SPORADICALLY • 10% of melanomas are of the INHERITED type Familial Atypical Multiple Mole-Melanoma Syndrome (FAMMM) Ask these questions: Risk Factors for Sporadic (Nonhereditary) Melanoma 1) Personal or family history of melanoma? 2) History of atypical nevus that has been • Numerous normal nevi, some atypical nevi removed? • Sun sensitivity, excessive sun exposure 3) Presence of new or changing mole- i.e. change in size or color? 12
8/5/2019 Clinical Features of FAMMM • Often numerous nevi (30-100+) • Nevi > 6mm in diameter • New nevi appear throughout life (after age 30) • Nevi in sun-protected areas (buttocks, breasts of females) • Family history of atypical nevi and melanoma Prevention • Self examination/spousal exam for low-risk individuals • Self examination/spousal exam and regular physician examination (yearly to every several years) for intermediate risk individuals • Self examination and examination by a dermatologist every 3-12 months for FAMMM kindred 13
8/5/2019 If not sure: • Measure and see pt back in 3-6 months for reevaluation!! Teledermatology Response: • Have pt come back-take another picture and let’s compare • Primary Care Provider: • Epidermoid cyst-not inflamed. Does not need to be excised unless repeatedly On pts back-Sometimes wife squeezes out inflamed. smelly cheese –like material. Advice? • Wife should stop squeezing this-could cause cyst contents to be released into surrounding tissue-causing inflammation • If pt wants this excised-please send to surgery for excision-may not be covered by insurance 14
8/5/2019 • Primary Care Provider: Pt came in with 2 day history of enlarging lesion and increasing pain. • Started doxycyline Inflamed Epidermoid Cysts • Antibiotics-USELESS-this is abscessed-6 papers and metanalysis shows that antibiotics will not help • Cysts smaller than 1 cm- try intralesional Kenalog injection ; see them back in few days-you can exacerbate the inflammation • This cyst is bigger than 1 cm • INCISE and DRAIN and PACK-send to surgery or ER today • 6 weeks later, inspect for residual cyst and send pt for excision to surgery 15
8/5/2019 Keloids • These are keloids • Did they come from acne-if so-look for other acneiform lesions and let me know-I can discuss systemic acne treatment so that pt does not get new keloids after every acne breakout. • Will need intralesional kenalog-will book with derm clinic for monthly injections-book within next two months Vitiligo • Immune system hyperactive • thyroid disease (19%) and other autoimmmune diseases-screen for thyroid dz every 3 yrs • Trial of clobetasol oint qd x 3 months; if not working tacrolimus bid x 3 months then leave it alone • Makeup, counselling 16
8/5/2019 Alopecia areata • Non-scarring alopecia-we have no idea why it starts and we don’t have preventive treatment in terms of halting future episodes • Inject with intralesional kenalog 10mg/cc q month for at least 6 months to see if there is hair regrowth • For widespread areas :Trying to understand the immune pathway-opremilast and JAK2 inhibitors 17
Recommend
More recommend